Chapter 10
Dizziness
Introduction
Definition
Dizziness has typically been divided into four subtypes (Box 10.1). In practice, however, older people frequently report symptoms that suggest more than one subtype (1). In addition to this, patients may use the term ‘dizziness’ to describe sensations of weakness, lethargy or lassitude.
Background
Dizziness is a common symptom in older people, with studies suggesting a prevalence of 21–29% in people aged over 65 in the community in the United Kingdom and the United States. It is responsible for 3.3% of ED visits (3).
The causes of dizziness are varied, ranging from the benign and self-limiting to life-threatening conditions and time-sensitive emergencies (Figure 10.1).
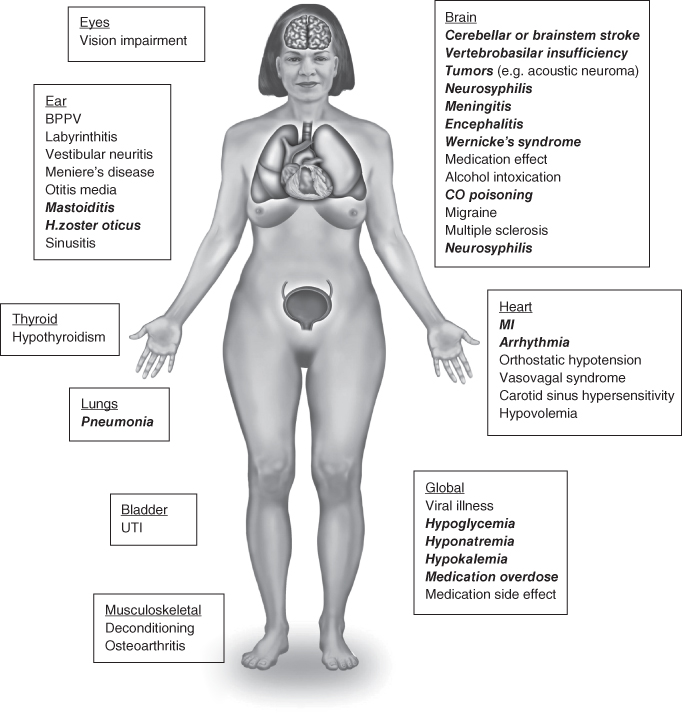
Figure 10.1 Causes of dizziness in older patients. Conditions requiring rapid diagnosis in the ED are shown in bold italic type.
Source: From Lo AX, Harada CN. Geriatric dizziness: evolving diagnostic and therapeutic approaches for the emergency department. Clin Geriatr Med. 2013 Feb;29(1):181–204. Reproduced with permission of Elsevier.
History
A detailed history is very helpful in directing further investigations and identifying potentially life-threatening conditions that may necessitate more timely management (Table 10.1).
Table 10.1 Common causes of dizziness in older patients for different types of symptoms
| Symptom | Subtype | Likely cause | Comment |
| Vertigo | Position induced | Benign paroxysmal positional vertigo (BPPV) | If nystagmus does not match BPPV (it should rotational with the fast phase towards the affected side), consider central pathologies; if induced by neck rotation, consider cervical vertigo |
| Acute onset persistent with neurologic signs | Stroke/tumour/neuro-degenerative disease | Acute ischaemia involving vestibular structures can mimic vestibular neuronitis | |
| Acute onset persistent without neurologic signs | Labyrinthitis Vestibular neuronitis | Differential diagnosis is based on the presence of hearing loss | |
| Recurrent with no neurologic signs | Ménière’s disease Migraine | Late onset Ménière’s disease is possible but not common. Migraines lack progressive auditory symptoms. Transient ischaemic attacks (TIA) should be considered in patients with risk factors | |
| Disequilibrium | Acute or rapidly progressive | Stroke | Autoimmune post-infectious diseases should also be considered; may also include severe occulomotor problems |
| Worse in the absence of other sensory inputs | Bilateral vestibular loss | Check for ototoxicity. Hearing loss or oscillopsia may be present | |
| Worse in the absence of vision with numbness/weakness | Proprioception and somatosensory loss | Often associated with peripheral neuropathy from metabolic, renal failure, toxic or diabetic causes | |
| With bradykinesia/rigidity/tremor | Parkinsonism | Frontal lobe or other basal ganglia disorders | |
| With speech disorder/ incoordination/intention tremor | Cerebellar lesion | The imbalance is usually the same with and without vision | |
| Isolated disequilibrium/gait difficulty/light-headedness | Disequilibrium of ageing | Often accompanied by borderline diffuse central findings but no other specific complaints | |
| Presyncope | With BP drop on standing | Postural hypotension | Associated with reduced blood volume, autonomic disorders or chronic use of antihypertensives |
| Abnormal cardiac examination | Heart valve disease, arrhythmia | Warrants consideration of 24-hour ECG | |
| Introduced by fear or anxiety | Vasovagal | Decline in heart rate and blood pressure leads to decrease in cerebral blood flow | |
| Light-headedness (nonspecific) | Associated with fear, anxiety or depression | Psychogenic | Often accompanied by autonomic symptoms |
Source: From Barin K, Dodson EE. Dizziness in the elderly. Otolaryngol Clin North Am. 2011 Apr;44(2):437–454, x. Reproduced with permission of Elsevier.
What is the nature of the dizziness?
Is there a sensation of movement or spinning, a feeling of light-headedness, or feeling of being about to faint? Is there a sensation of being on a boat or merry-go-round?
Precipitants of the dizziness
Is dizziness experienced when the patient stands up, or moves from lying to sitting or standing? Is it precipitated by the patient turning their head or whilst turning over in bed?
Timescale
The causes of abrupt onset vertigo are different from the causes of chronic unsteadiness or light-headedness, and a careful distinction should be made.
Frequency of attacks
The number and frequency of attacks should be established, along with tempo and duration.
Past medical history
The patient’s medical history should be explored with particular focus on previous conditions causing dizziness such as Ménière’s disease, falls, malignancy, previous head trauma, and cardiac or vascular risk factors that may place the patient at increased risk of stroke.
Medication and alcohol history
Alcohol excess can cause dizziness by either direct cerebellar toxicity or chronic cerebellar damage Cardiovascular medication, particularly antihypertensives, may result in postural hypotension leading to presyncopal dizziness.
Examination
General examination
A comprehensive physical examination is important for evaluating a dizzy patient (Table 10.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree