Fig. 24.1
Schematic cross-sectional view demonstrating the resection area of distal pancreatectomy with en bloc celiac axis resection (DP-CAR). The dotted line indicates the dissection plane. adr adrenal gland, Ao aorta, CA celiac axis, CHA common hepatic artery, crus crus of the diaphragm, Du duodenum, g celiac ganglion, IVC inferior vena cava, pl celiac plexus, PV portal vein, SA splenic artery, SV splenic vein
24.1.1 Development of DP-CAR
This procedure was originally designed as en bloc lymphadenectomy combined with total gastrectomy and resection of the celiac axis for advanced gastric cancer by Appleby in 1953 [3]. It was first adopted by Nimura in 1976 [4] for patients with advanced pancreatic body cancer with invasion of the celiac axis. A modification to the procedure with preservation of the entire stomach was made by Ogata and his colleagues [5] in 1991 (in Japanese with English abstract) and Kondo [6] in 2001, which resulted in better postoperative nutritional status. The first report regarding the long-term outcome of DP-CAR was published by Kondo and Hirano in 2007 [7], which included the results of 24 consecutive patients with favorable postoperative survival. Since then, the procedure and the term “DP-CAR” have been widely acknowledged. Nowadays, several pancreatic surgeons have performed this procedure for carcinoma of the body and tail of the pancreas.
24.1.2 Resected and Preserved Organs in DP-CAR
Perineural invasion in patients with pancreatic body cancer can spread toward the celiac plexus and ganglions directly or via the nerve plexuses surrounding the splenic and common hepatic arteries. Although DP-CAR includes en bloc resection of these arteries and plexuses, reconstruction of the arterial system is not required because of early development of a collateral arterial circulation via the pancreaticoduodenal arcades from the superior mesenteric artery. The entire alimentary tract, including the stomach and bile duct, which are not invaded by the cancer, is preserved. Cholecystectomy is, however, performed for preventing postoperative ischemic rupture of the gall bladder. If the tumor of the pancreatic body invades other organs directly, concomitant resection of the organs, including the alimentary tract, could be performed. However, in the case that a tumor has invaded the stomach to a depth that necessitates full-thickness resection, total gastrectomy should be considered because healing of the anastomosis might be disturbed by an insufficient collateral arterial flow. As far as possible, the entire stomach should be preserved in cases without cancer invasion of the stomach, to maintain the patient’s nutritional status and tolerance of oral anticancer agents. SMA preservation, even with complete eradication of the surrounding plexus, is the key feature of this procedure, which maintains arterial supply to the hepatobiliary system and stomach. Resection of the portal vein and middle colic vessels is an optional procedure.
24.1.3 Arterial Supply to the Liver and the Stomach After DP-CAR
After division of the CA with the CHA and splenic artery (SA), the hepatic and gastric arterial flow depend on the flow from the gastroduodenal artery (GDA), which should, therefore, definitely be preserved with the pancreatic head during DP-CAR. The collateral pathways via the SMA, pancreaticoduodenal arcades, and GDA maintain the arterial blood supply to the hepatobiliary system. Since the collateral pathways also ensure arterial flow to the right gastroepiploic artery, the entire stomach can be preserved (Fig. 24.2).
Fig. 24.2
Schematic drawing of collateral arterial pathways via the pancreaticoduodenal arcades from the superior mesenteric artery following DP-CAR. The arrows show the direction of arterial flow from the superior mesenteric artery to the liver and stomach via the pancreaticoduodenal arcades. APD anterior pancreaticoduodenal arcade, CA celiac axis, CHA common hepatic artery, GDA gastroduodenal artery, GEA right gastroepiploic artery, LGA left gastric artery, PHA proper hepatic artery, PPD posterior pancreaticoduodenal arcade, SA splenic artery, SMA superior mesenteric artery
Preoperative coil embolization of the CHA is routinely used to enlarge the collateral arterial pathway, so as to reduce ischemia-related complications such as ischemic gastropathy, liver abscess, and perforation of the biliary system [8] (Fig. 24.3).
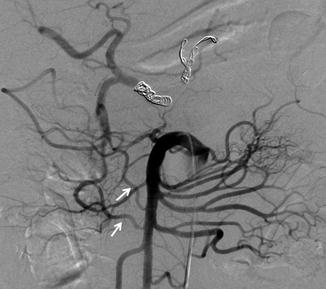
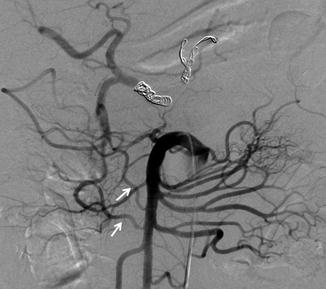
Fig. 24.3
Angiography image of the superior mesenteric artery just after embolization of the common hepatic artery. The arrows show the enlarged collateral arterial pathway in the pancreatic head via the posterior and anterior pancreaticoduodenal arteries
24.1.4 Selection of Candidates for DP-CAR
Tumor progression is cautiously evaluated mainly with preoperative multi-detector row computed tomography (MDCT), with supplemental use of magnetic resonance imaging (MRI) and endoscopic ultrasonography (EUS). The indication for DP-CAR is locally advanced ductal adenocarcinoma of the body of the pancreas, such as that involving or abutting the CHA, the root of the SA, and/or the CA, without involvement of the GDA, SMA, and inferior pancreaticoduodenal artery. Patients with involvement of less than approximately half the circumference of the SMA plexus should be considered candidates for DP-CAR because complete dissection of the SMA plexus without exposing the cancer can be achieved by dividing the plexus on the side opposite to that of the tumor. For oncologically safe ligation and division of the root of the CA in front of the aorta, a 5–7 mm noncancerous length of the CA from the adventitia of the aorta is required.
24.1.5 Surgical Procedure of DP-CAR
DP-CAR usually includes resection of the distal pancreas and the spleen, together with en bloc resection of the celiac, common hepatic and left gastric arteries, the celiac plexus and bilateral ganglions, and the circumferential nerve plexus around the SMA. The left perirenal fat tissue, the left adrenal gland, the entire retroperitoneal fat tissue containing lymph nodes cranial to the left renal vein, the transverse mesocolon covering the body of the pancreas, and the inferior mesenteric vein are also resected (Fig. 24.4 ).
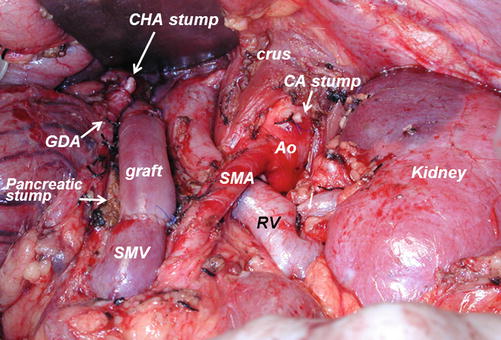
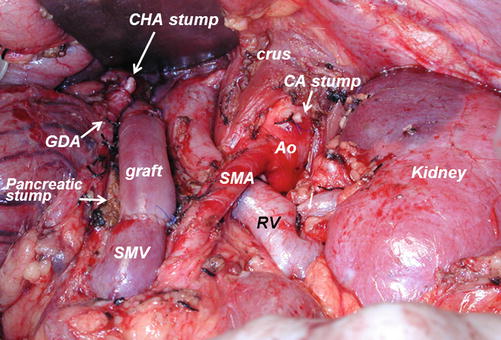
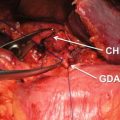
Fig. 24.4




Post-resection view during distal pancreatectomy with en bloc celiac axis resection (DP-CAR). Ao aorta, CA celiac axis, CHA common hepatic artery, crus crus of the diaphragm, GDA gastroduodenal artery, graft interposed iliac vein graft, IVC inferior vena cava, RV renal vein, SMA superior mesenteric artery, SMV superior mesenteric vein
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree