Distal Humeral Resection with Prosthetic Reconstruction
James C. Wittig
Martin M. Malawer
BACKGROUND
The distal humerus is a relatively rare site for primary bone sarcomas. It is more commonly involved by neoplasm through metastatic spread. The distal humerus or elbow joint also can be secondarily involved by soft tissue sarcomas arising from the adjacent musculature or intermuscular soft tissues. Sarcomas that arise from the most proximal portions of the flexor-pronator group or common forearm extensor muscles may involve the distal humerus by direct invasion or by growing around the circumference of the distal humerus. Sarcomas that arise from the distal brachialis muscle or triceps muscle also may secondarily involve the distal humerus.
Tumors arising in this area that involve the soft tissues are technically challenging to resect. These tumors usually are juxtaposed to and displace the adjacent neurovascular structures that lie in immediate proximity to the distal humerus and within the antecubital fossa.
The key to a safe and successful resection lies in identifying and mobilizing all important neurovascular structures (eg, brachial artery and vein, median nerve, ulnar nerve, and radial nerve) away from the neoplasm and distal humerus. The biceps muscle must be preserved in order to restore elbow flexion after reconstruction.
Each of the neurovascular structures is identified proximal to the tumor, in normal tissue, in the distal one-third of the arm. These structures are dissected in a proximal to distal direction, separated from the neoplasm, and mobilized across the elbow joint. Once these structures are mobilized and protected, it is safe to proceed with removing the distal humerus and tumor en bloc.
In most cases, even the most extreme cases, the neurovascular structures are displaced and not encased by neoplasm, making limb-sparing surgery an option in lieu of an amputation (FIG 1). Gross tumor involvement of a single nerve is not an absolute indication for an above-the-elbow amputation. Involvement of more than one major nerve or the main vascular supply is an indication for an above-the-elbow amputation when treating a sarcoma with curative intention. In cases of metastatic carcinomas, where treatment is palliative, adjuvant treatments such as radiation or chemotherapy should be considered before proceeding with an amputation.
Prosthetic reconstruction of the distal humerus and elbow joint with a modular, segmental, tumor prosthesis including a semiconstrained, hinged elbow joint is a reliable means of skeletal reconstruction following resection. Multiple muscle rotation flaps, retensioning the biceps muscle, and flexorplasty of the forearm musculature are key steps to restoring elbow flexion power.
ANATOMY
To resect tumors involving the distal humerus safely and adequately, the major neurovascular structures around the distal humerus should be exposed and identified.
In the middle one-third of the arm, most of the important neurovascular structures lie within a fibrous sheath, in the groove between the biceps and triceps muscles, along the medial side of the arm, just medial to the brachialis muscle. These structures include the following:
The brachial artery, which is surrounded by two small brachial veins
The median nerve, which lies directly anterior to the brachial artery
The cephalic vein and medial antecubital cutaneous nerve, which lie superficial to the brachial artery
The ulnar nerve, which is surrounded by the superior ulnar recurrent artery and two veins that lie just medial and posterior to the brachial artery
The medial brachial cutaneous nerve, which lies in the superficial subcutaneous tissue at this level
At this level, the radial nerve lies within the spiral groove of the humerus along the posterolateral aspect of the arm.
The brachial artery and veins are the continuation of the axillary artery and vein at the level of the lower border of the subscapularis muscle. The brachial artery and veins travel distally along the medial side of the arm, deep to the fascia, in the interval between the biceps and triceps muscles, medial to the brachialis muscle.
The profunda brachii artery arises proximally from the brachial artery at the lower border of the latissimus dorsi
muscle. It traverses dorsally and laterally with the radial nerve and enters the spiral groove.
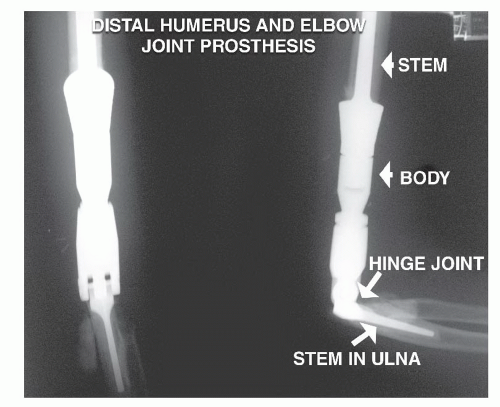
FIG 1 • Postoperative radiograph showing a distal humeral prosthesis and elbow joint. This prosthesis was inserted to avoid an amputation.
The brachial artery gives off several branches along its course to the biceps, brachialis, and triceps muscles. In the antecubital fossa, the brachial artery lies on the anterior surface of the brachialis muscle, immediately adjacent and lateral to the median nerve. The brachial artery passes just deep to the bicipital aponeurosis to enter the forearm. The inferior ulnar collateral artery arises from the brachial artery just proximal to the bicipital aponeurosis and passes medially just along the proximal aspect of the medial condyle of the humerus. After the brachial artery passes underneath the bicipital aponeurosis, it branches into the ulnar artery, radial recurrent artery, and radial artery.
The median nerve travels distally in the arm, closely applied to the anterior aspect of the brachial artery. As the median nerve approaches the antecubital fossa, it crosses over medially so that it occupies a position immediately medial to the brachial artery and lateral to the pronator teres muscle in the antecubital fossa.
The ulnar nerve occupies a position slightly more medial and posterior to the brachial artery in the midarm. In the distal one-third of the arm, the ulnar nerve travels posteriorly and pierces the medial intermuscular septum. It travels along the medial side of the triceps muscle and enters a groove (cubital tunnel) along the posterior aspect of the medial epicondyle of the humerus. The ulnar nerve is tethered within this groove by ligamentous tissue. It then travels distally and enters the forearm by passing through the humeral and ulnar heads of the pronator teres muscle. In the forearm, the ulnar nerve lies along the deep surface of the flexor carpi ulnaris muscle.
The medial antebrachial cutaneous nerve is a small nerve that lies deep to the fascia between the median and ulnar nerves at the midarm level. In the distal one-third of the arm, the nerve occupies a more superficial position in the subcutaneous tissue.
The radial nerve arises from the posterior cord of the brachial plexus. At the inferior border of the latissimus dorsi muscle, the radial nerve passes posteriorly, along with the profunda brachii artery, through the interval between the long head of the triceps and the humerus. The radial nerve enters the spiral groove of the humerus and travels distally, wrapping around the posterior aspect of the humerus, in the interval between the medial and lateral heads of the triceps muscle. In the distal one-third of the arm, the radial nerve passes through the lateral intermuscular septum and enters the anterior compartment of the arm, where it resides in the interval between the brachioradialis muscle and brachialis muscle. The radial nerve continues distally into the forearm. At the lower, lateral border of the brachialis muscle, just proximal to the supinator muscle, the radial nerve divides into the posterior interosseous nerve and the superficial radial nerve. The posterior interosseous nerve passes through the substance of the supinator muscle. The superficial radial nerve travels distally along the deep surface of the brachioradialis muscle.
INDICATIONS AND CONTRAINDICATIONS
Indications
High-grade and some low-grade bone sarcomas
Soft tissue sarcomas that surround or invade the distal humerus or elbow joint secondarily
Solitary metastatic carcinomas to the distal humerus
Metastatic carcinomas that have destroyed a significant portion of the distal humerus, which precludes other methods of resection and fixation
Local complications resulting from other treatments for tumors involving the distal humerus (eg, nonunion of a pathologic fracture following radiation, untreatable infection of bone after prior surgery)
Contraindications
Absolute contraindications include tumor involvement of the neurovascular bundle.
Involvement of a single major nerve is not an absolute contraindication. The nerve can be resected with the neoplasm.
Encasement of the brachial artery and veins or two or more major nerves usually precludes a limb-sparing resection.
Final determination regarding the need for an amputation is made at the time of surgery, after the neurovascular structures are explored. Adjuvant treatments such as radiation and chemotherapy should be considered for palliation of metastatic carcinomas prior to proceeding with an amputation.
Relative contraindications include tumor contamination of the operative site from hematoma following a poorly performed biopsy or pathologic fracture or a previous or active infection. Recently, we have successfully treated patients with pathologic fractures with induction chemotherapy, immobilization, and limb-sparing surgery if there is a good clinical response and fracture healing; survival has not been compromised, and local recurrence is less than 10%.
IMAGING AND DIAGNOSTIC STUDIES
The most useful imaging studies are plain radiography, computed tomography (CT), magnetic resonance imaging (MRI), arteriography, and bone scan. These studies are useful for diagnosis; evaluating local and distant extent of disease; and, for select sarcomas, gauging the response to preoperative chemotherapy. Radiologic studies are necessary to determine the exact anatomic extent of the neoplasm so that the surgical procedure can be planned accurately.
Plain Radiographs
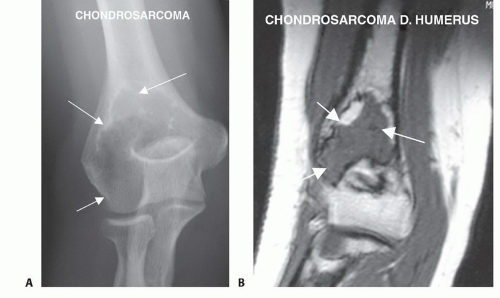
Plain radiographs of the humerus and elbow are used to localize the anatomic origin of the tumor, formulate a differential diagnosis, and estimate tumor extent (FIG 2A).
After preoperative chemotherapy for an osteosarcoma, plain radiographs can be used to estimate the response of the tumor to the chemotherapeutic agents. A good response (>90% tumor necrosis) is indicated by extensive tumor calcification, periosteal new bone formation, and healing of pathologic fractures.
Computed Tomography
CT is most useful for evaluating cortical bone changes and extent of cortical destruction by tumor. In the case of a metastatic carcinoma, it aids with decision making regarding the indication for a resection and prosthetic reconstruction versus curettage and internal fixation. Extensive cortical destruction throughout a significant circumference of the bone is an indication to proceed with a resection of the distal humerus and prosthetic reconstruction.
CT also is useful for detecting subtle mineralization, calcification, or ossification within the neoplasm that may assist in diagnosis.
CT is considered complementary to MRI in evaluating the soft tissue component of the neoplasm and proximity to the neurovascular structures, particularly a contrast-enhanced CT scan.
CT also assists with detection of subtle cortical erosion and frank invasion of the distal humerus by adjacent soft tissue sarcomas that may not be clearly delineated on MRI or plain radiographs.
After preoperative chemotherapy of an osteosarcoma, CT characteristically shows a rimlike calcification in those tumors that have had a good response.
Chest CT is most sensitive for detecting lung metastases.
Magnetic Resonance Imaging
MRI is most accurate for determining intra- and extraosseous tumor extent as well as for detecting skip metastases. An appreciation of intraosseous extent is necessary for determining the length of bone resection. A post-chemotherapy MRI is fundamental in the preoperative plan.
The humerus usually is transected approximately 2 to 3 cm proximal to the intramedullary extent of the neoplasm as visualized on a T1-weighted MRI scan.
Proximity of the extraosseous component to the brachial vessels, median nerve, ulnar nerve, and radial nerve also can be evaluated, as can secondary involvement of the distal humerus and elbow joint by adjacent soft tissue sarcomas.
Standard T1-weighted, T2-weighted, fat-suppressed, and gadolinium-enhanced images are recommended (FIG 2B).
Bone Scintigraphy
Bone scintigraphy is used to determine intraosseous tumor extent and is compared to the MRI scan to ensure accuracy. It also is used to detect bony metastases and skip metastases.
Positron Emission Tomography/Computed Tomography
Positron emission tomography (PET)/CT is an imaging technique that allows measurement of the level of metabolic activity and perfusion in different organs. The most frequent radioactive substance used is fluorodeoxyglucose (FDG). PET/CT is used to detect the primary or metastatic tumors and recurrences after tumor treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree