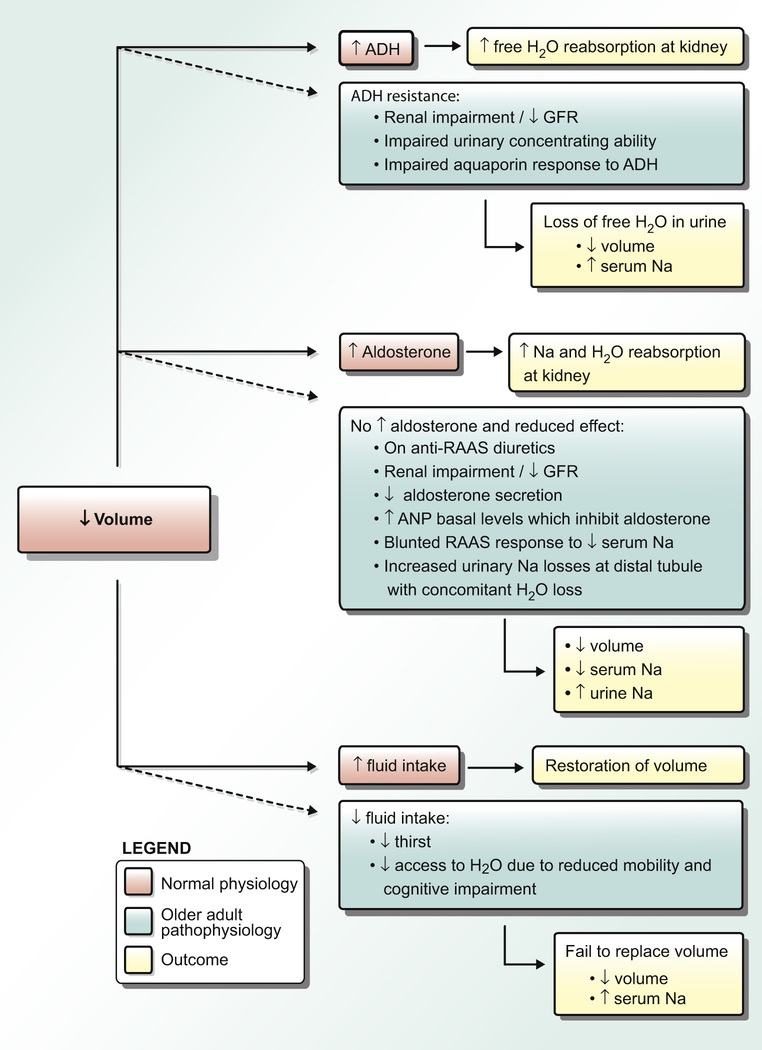
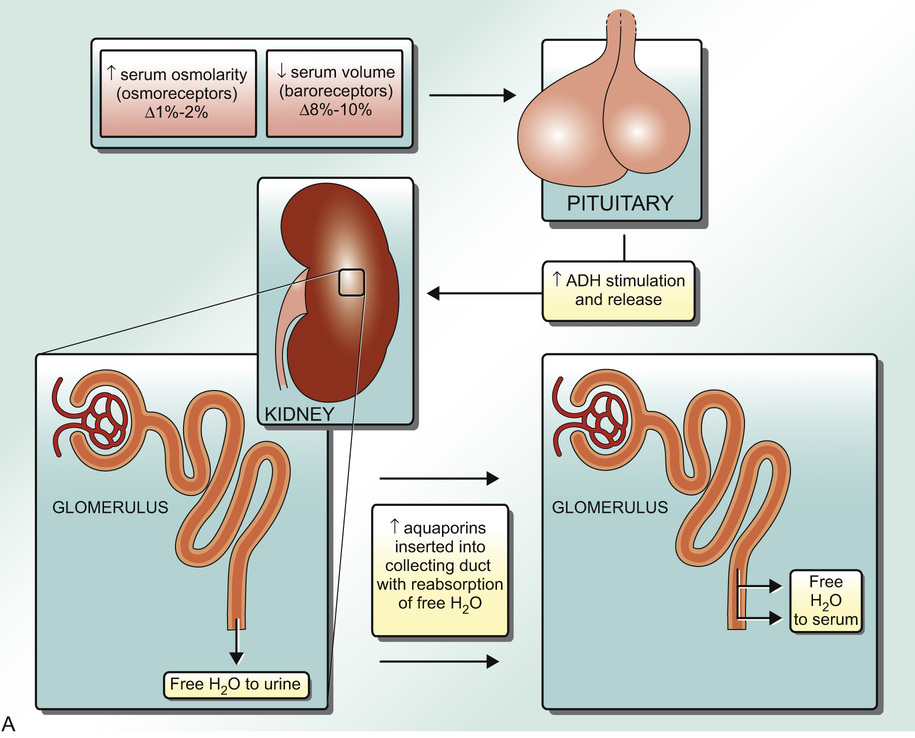
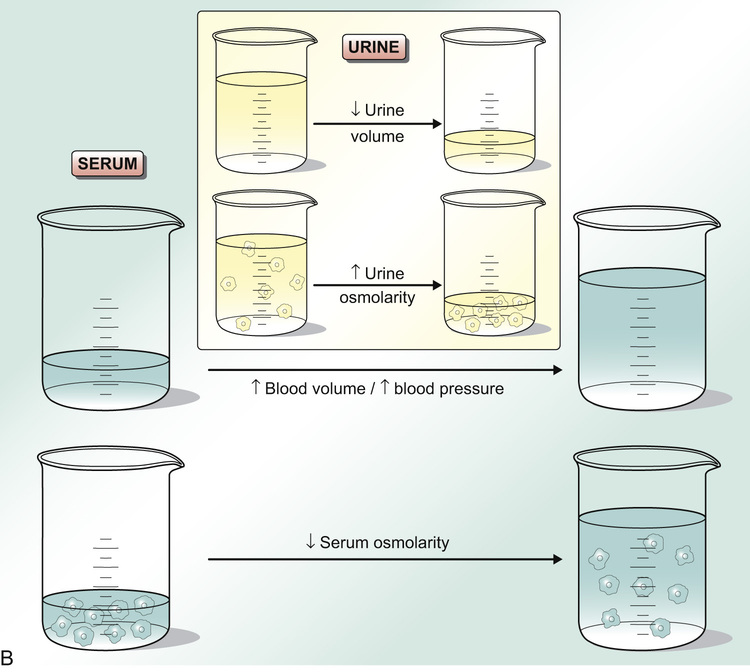
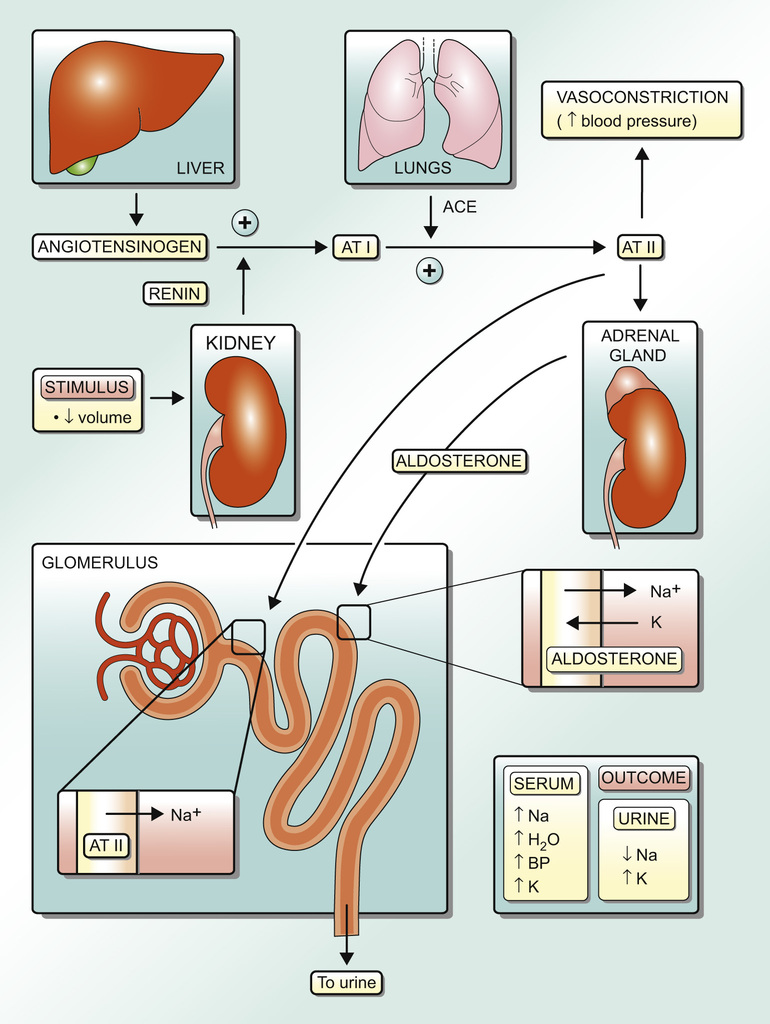
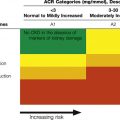
Amanda Miller, Karthik Tennankore, Kenneth Rockwood With aging, several changes to the regulation of water and electrolyte homeostasis can occur. Total body water (TBW) is commonly reduced. Older adult patients are less responsive to hormonal mediators of water, electrolyte, and mineral balance. Commonly, older adults have impairments in thirst sensation, renal function, and factors that regulate salt and water balance, making them more vulnerable to age-associated diseases and iatrogenic events involving water and electrolytes disturbances.1 These and other factors make older adults more susceptible to physiologic disturbance and less able to correct or compensate for these metabolic derangements than their younger counterparts. Therefore, with any perturbation in fluid or electrolyte balance, older adult patients are at a significantly increased risk of adverse outcomes. The occurrence and severity of electrolyte abnormalities appear to be increased in older people who are frail. This may result in catastrophic consequences in this population if fluid and electrolyte abnormalities are not promptly recognized and treated. An awareness of this impairment in fluid and electrolyte regulation in aging individuals will help health care providers to better manage these issues.1 TBW content is maintained through a number of physiologic responses to changes in fluid status. In middle age, roughly 60% to 65% of body weight is made up of water. With changes in body composition caused by aging (including decreased muscle mass and increased fat mass), the percentage of body water is reduced, such that by 75 years of age TBW comprises only 50% of a person’s weight.1 TBW is reduced by 10% to 15% in older adults,2 and this reduction is more pronounced in women.1 In consequence, a given volume of fluid represents a greater relative percentage of TBW, and so older adults may experience more profound derangements in serum electrolyte concentrations as a result of fluid shift compared to younger people.1 In young adults, TBW is controlled primarily through the thirst and renal responses to either increased or decreased extracellular fluid (ECF) volume and/or serum osmolality. The thirst response is triggered by hypovolemia, often manifested as hypotension, or by an increased serum osmolality. This leads to increased fluid intake, allowing restoration of normal physiologic parameters. Contrarily, thirst is generally suppressed in situations of increased ECF volume or low serum osmolality, a situation in which drinking excess dilute fluid could lead to worsening volume overload and further reduction of serum osmolality. In addition to less TBW, older adults face challenges in maintaining water homeostasis (and stable ECF volume status) on the basis of a number of impaired physiologic processes (Figure 82-1). Given that frailty results in impaired physiologic reserve, these problems may occur more frequently in frail patients. First, older adult patients have a reduced thirst response with decreased desire for and intake of fluid following a period of water deprivation compared with younger individuals.3 The mechanism for this is unknown but may be related to the fact that older adults have a higher baseline serum osmolality set point and thus require a greater change in serum osmolality to trigger the thirst center (albeit suboptimally).4 Additionally, they may have limited access to fluid replacement on the basis of reduced mobility or cognitive deficits.1 As such, older adults are at higher risk for both dehydration (net water loss) and hypovolemia because of decreased fluid intake. This is especially true after periods of water/fluid deprivation. As is typical in age-related disorders, the mechanisms behind water homeostasis in older adults are complex: commonly, multiple deficits accumulate to impair function.5,6 Therefore, it is no surprise that impairment of water homeostasis in older adults is associated with decreased renal mass,7 reduced cortical blood flow,8 and a decreased glomerular filtration rate (GFR).9 The renal response to hypovolemia and increased serum osmolality is reabsorption of free water through stimulation of antidiuretic hormone (ADH). ADH is a peptide hormone secreted by the hypothalamus and stored in the posterior pituitary, which functions to insert water channels (aquaporins) in the renal collecting duct to reabsorb free water and reduce urinary water losses10 (Figure 82-2, A). This results in a more concentrated urine and a decrease in serum osmolality with a concomitant increase in blood volume (Figure 82-2, B). Free water retention is valuable in situations where an increase in TBW is required to restore normal physiologic ECF volume status and osmolality, for example, in dehydration. In periods of hypotension, stretch receptors in the aorta and carotid arteries are activated to stimulate ADH secretion so that the body can retain enough fluid to restore blood pressure. Likewise, serum hyperosmolality is detected by osmoreceptors in the hypothalamus, which act to stimulate both ADH secretion and thirst. This leads to free water retention and increased water intake, with reduction of serum osmolality back toward normal level.9 Osmoreceptors are much more sensitive at stimulating ADH than are stretch receptors. The body tolerates changes in serum osmolality of only 1% to 2% before stimulating or suppressing ADH secretion. On the contrary, it takes a volume change of 8% to 10% (change in mean arterial pressure by 20% to 30%) before stretch receptors are triggered and ADH secretion is affected.11 Incomplete coordination of compensatory responses is one manifestation of the impaired repair process associated with frailty,12 and occasionally there is a mismatch between serum osmolality and ECF volume status. For example, when older adults have solute and volume losses of gastrointestinal (e.g., diarrheal) or renal (e.g., diuretic) cause with access to only solute-poor fluid replacement (e.g., water at the bedside), they can develop progressive hypo-osmolality without full restoration of ECF volume. In this situation, low serum osmolality suppresses ADH, whereas hypovolemia stimulates it. Intuitively, given that preservation of volume status is most essential, ADH will be influenced by ECF volume alone in the face of worsening serum osmolality. In consequence, free water will be reabsorbed and the patient’s serum sodium will be further reduced as volume status is corrected. Further complicating the issue, many older patients have an impaired urinary concentrating ability (see Figure 82-1). As such, in settings where ADH is maximally stimulated (hyperosmolar hypovolemia), the aged kidney is only able to achieve urine osmolalities half that of younger individuals.1 This submaximal urine osmolality is a result of inappropriate loss of free water in the form of dilute urine, which is maladaptive in the face of reduced TBW and perpetuates the problem of either reduced volume or, in some cases, increased serum osmolality.1 ADH levels in older adults are greater than those demonstrated in younger patients, both at baseline and in stimulated states. Thus, inadequate urinary concentrating ability is likely caused by an impaired aquaporin response or a medullary concentrating defect which increases free water excretion in the face of an intact ADH system.1 It is interesting that in patients with Alzheimer dementia, some studies report a subphysiologic ADH response to dehydration, in comparison to older patients without dementia.1 The mechanism for this has yet to be elucidated. In combination with functional constraints that may limit a patient’s access to water, this inadequate ADH response puts people with Alzheimer disease at an even higher risk for dehydration than other older individuals.1 Many other factors can contribute to fluid disturbances in older adults. Those with urinary incontinence often drink less to avoid frequent micturition. Diarrhea, vomiting, and gastrointestinal bleeding can contribute to volume loss in older adult patients, as can decreased intake in the context of anorexia and depression. Poorly controlled diabetes, stroke, draining wounds, fever, rapid breathing, infection, and burns can also impair water and electrolyte balance in aged individuals. In addition to volume loss (with resultant ADH stimulation and increased fluid intake), other conditions such as the syndrome of inappropriate antidiuretic hormone (SIADH) and hypotonic fluid administration can result in hypo-osmolar euvolemia/hypervolemia in older adult patients. In such cases, compared with younger people, many older adults have a reduced ability to excrete free water, taking 50% longer to return to baseline volume and serum osmolality.1 This can place them at an increased risk of dilutional hypo-osmolality or volume overload after intake of large volumes of liquids, for example, when receiving hypo-osmolar intravenous fluids during hospitalization. The consequences of impaired water homeostasis in older individuals include abnormal volume status and electrolyte abnormalities, most notably hyper- and hyponatremia.1 Sodium is the major cation in ECF and is the major contributor to serum osmolality in the body. Hyper- and hyponatremia are common in older adults and most evident in hospitalized patients or individuals living in long-term care facilities. Cross-sectional studies have found that hyponatremia may be present in as many as 15% to 18% of nursing home residents.8 In contrast, approximately 30% of nursing home residents requiring acute hospitalization were shown to be hypernatremic in one study,13 a result that has been reproduced in studies over a period of almost three decades.14,15 Hypovolemia may be a major precipitant of both hyper- and hyponatremia, depending largely on a patient’s access to free water. Older patients are at an increased risk of free water loss because of impaired water concentrating abilities in the aged kidney, but they are also prone to urinary sodium losses as a result of dysfunction at the loop of Henle.16 Taken together, this results in reduced ECF volume status, which is corrected by increased stimulation of ADH and a resultant dilutional hyponatremia in patients with access to water and increased water intake. Conversely, in patients with an impaired thirst mechanism, or in those who don’t have access to water because of their impaired mobility or altered cognitive status, the effect on serum sodium is variable. This is because even though ADH is still maximally stimulated in this circumstance, lack of access to water prohibits the development of dilutional hyponatremia. Renal sodium losses are ongoing, if only to a mild degree, and are generally accompanied by some degree of concurrent water loss despite maximal stimulation of ADH. As such, the resulting serum sodium may be either increased or decreased depending on whether relatively more sodium or free water is lost in the urine. In addition to ADH, sodium status is also influenced by the renin-angiotensin-aldosterone system (RAAS). In periods of low sodium intake, many older patients show an impaired ability to restrict urinary sodium losses compared to their younger counterparts.1 This may result in hyponatremia and, because water follows sodium along osmotic gradients, in hypovolemia with renal water losses. In addition to loop of Henle dysfunction, the mechanism for reduced sodium concentrating ability in the kidneys of older adults has been proposed to be partially due to a blunted RAAS response to low serum sodium (see Figure 82-1).17 In younger individuals, hypovolemia stimulates RAAS, resulting in reabsorption of sodium and excretion of potassium in the renal tubules as a means of maintaining euvolemia and electrolyte homeostasis, respectively (Figure 82-3). An impaired RAAS, with less absorption of sodium and excretion of potassium in the face of hypovolemia, may thereby result in both hyponatremia and hyperkalemia in older hypovolemic patients. In addition, in older people, aldosterone is present at lower levels16 and is under a greater degree of inhibition on the basis of increased basal atrial natriuretic peptide (ANP) levels, which negatively feed back on RAAS, and on aldosterone directly. Furthermore, the renal tubules of older patients are less responsive to the effects of aldosterone.16 In consequence, in cases of hypovolemia, older adults can develop hyponatremia as a result of both serum sodium dilution via ADH and reduced conservation of sodium via an impaired RAAS. The obligatory renal sodium losses common in older adults is demonstrated by the fact that older people have been shown to have increased 24-hour urinary sodium losses compared with younger adults despite lower renal tubular sodium levels in the older adult population.17 Increased urinary sodium losses may also be influenced by the fact that older adults have been shown to have an increased ANP level, which fails to suppress in periods of hypovolemia.1 In younger adults, ANP is stimulated by hypervolemia and serves to stimulate renal sodium wasting with corresponding volume loss. In older patients, elevated ANP levels in periods of hypovolemia can exacerbate volume loss and put patients at increased risk of related complications.
Disorders of Water and Electrolyte Metabolism
Introduction
Water Balance
Electrolyte Balance
Sodium Metabolism
Disorders of Water and Electrolyte Metabolism
82