Maria Papaleontiou, Nazanene Helen Esfandiari
Disorders of the Thyroid
As an individual ages, several morphologic and physiologic changes occur in the entire endocrine system, including the thyroid gland. These changes can be explained by the amount of hormones secreted due to changes in target organs or by changes in the rate of metabolism of hormones.1 Thyroid dysfunction is common in older adults1 and may be associated with significant morbidity if not treated. Subclinical thyroid disease is the most common thyroid disorder in this population.2 The classic symptoms of thyroid dysfunction are usually absent or may be overlooked in older patients, making the diagnosis and subsequent management challenging. In addition, interpretation of thyroid function tests in older adults can be challenging due to age-dependent physiologic changes in thyroid function, coexistent chronic illness, and polypharmacy.1,3–6 Moreover, the risk of harm from treatment in the older adult population further complicates the decision-making process.
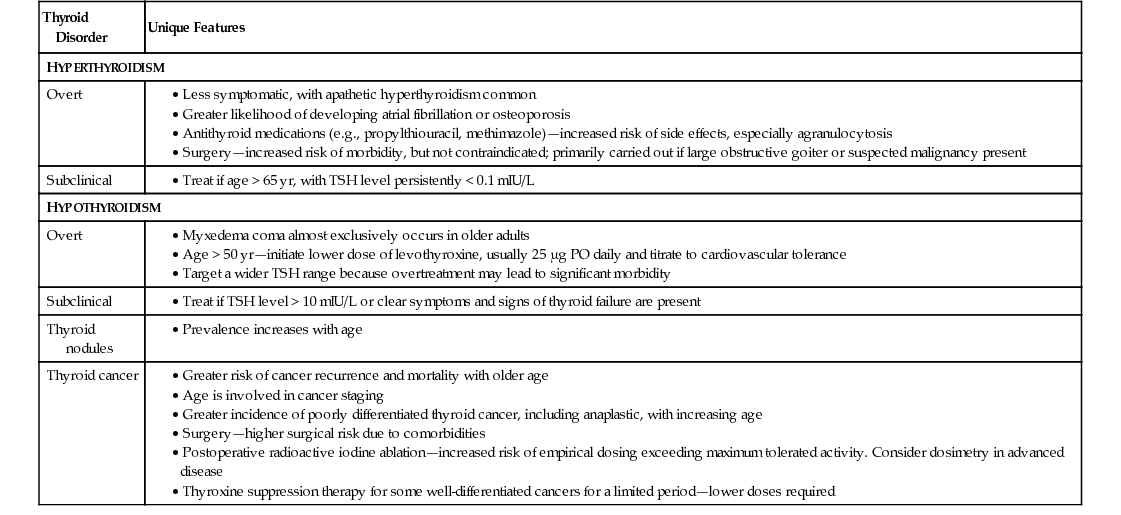
In this chapter we will review the epidemiology, clinical presentation, risks and complications, and management of thyroid disorders, including hyperthyroidism, subclinical hyperthyroidism, hypothyroidism, subclinical hypothyroidism, thyroid nodules, and thyroid cancer, in older adults. Unique features in the approach and management of thyroid disorders in older adults are summarized in Table 88-1.
TABLE 88-1
Unique Features in Approach and Management of Thyroid Disorders in Older Adults
| Thyroid Disorder | Unique Features |
| HYPERTHYROIDISM | |
| Overt | |
| Subclinical | |
| HYPOTHYROIDISM | |
Overt | |
| Subclinical | |
| Thyroid nodules | |
| Thyroid cancer | |
Thyroid Morphology and Aging
The normal aging process is associated with changes in the gross and microscopic appearance of the thyroid gland. Several studies have examined the relationship between the size of the thyroid gland and aging. Volumetric analyses performed using ultrasound, computed tomography (CT), or magnetic resonance imaging (MRI) have yielded varying results, with some studies documenting an increase7 and others no change8 or a decrease in the size of the thyroid gland occurring with age.9–11 This discrepancy may be related to diverse dietary iodine intake and because the gland also becomes more nodular with age.1
Age-associated histopathologic findings of the thyroid gland have also been documented. These include a reduction in follicle number and size, reduction in colloid content, degeneration and flattening of epithelial cells, increased interfollicular fibrosis of the connective tissue, and varying lymphocytic infiltration.1,12–16 In addition, the number of parafollicular cells (C cells) in the thyroid gland has been shown to increase with advancing age, with the formation of clusters and micronodular hyperplasia.15–17
Thyroid Function and Aging
Several studies have investigated the role of thyroid function in the aging process. Studies have shown increased serum thyroid-stimulating hormone (TSH) levels with increasing age, independent of antithyroid antibody presence2; in contrast, others have demonstrated decreased serum TSH levels in older adults.1,4 Populations in which the dominant thyroid pathology is thyroid deficiency secondary to Hashimoto thyroiditis display a trend for the TSH upper limit to increase with age.18–20 On the contrary, an inverse relationship between TSH and age is seen in iodine-deficient populations in which the dominant thyroid pathology is nodularity and increasing thyroid autonomy with age.21 In regard to free triiodothyronine (T3) levels, most studies have demonstrated an age-dependent decline, whereas free thyroxine (T4) levels remain relatively unchanged,1,4 and reverse T3 (rT3) levels increase with increasing age. However, interpretation of thyroid function tests in older adults is often complicated by the presence of chronic illness, (in which free T3 levels can be low and rT3 levels high), and polypharmacy.5 Furthermore, differences in iodine intake and the presence of autoimmune thyroid disease make the distinction between age-related and disease-related thyroid function abnormalities even more challenging.22
There is convincing evidence that higher levels of TSH are associated with longevity. Serum TSH levels have been shown to be significantly higher in centenarians (mean age, 98 years) as compared to controls (P < .001).23 Increased TSH levels and low to low-normal free T4 levels have also been shown to be associated with better survival in older adults.11,12,24,25 It is hypothesized that the association of a higher TSH level with longevity may be due to a correlated lower bioactivity of thyroid hormone, which in turn leads to a lower basal metabolic rate and thus potentially may serve as an adaptive mechanism to prevent catabolism in older adults.12
Moreover, the offspring of individuals with longevity were also shown to have higher TSH levels than age-matched controls without familial longevity (mean age, 70 years), indicating a genetic predisposition.26
Screening for Thyroid Dysfunction
Thyroid function disorders become increasingly frequent with advancing age. As a consequence, several organizations have issued recommendations regarding screening for thyroid dysfunction in the general population as a means of early detection of altered thyroid function. However, expert panels have continued to disagree about TSH screening of the general population (Table 88-2).
TABLE 88-2
Recommendations Regarding Screening for Thyroid Dysfunction in Adults
| Organization | Recommendations for Screening |
| American Academy of Family Physicians (AAFP) | Patients ≥ 60 yr |
| American Association of Clinical Endocrinologists (AACE) | Older patients, especially women |
| American College of Physicians (ACP) | Women ≥ 50 yr with incidental finding suggestive of symptomatic thyroid disease |
| American Thyroid Association (ATA) | Women and men ≥ 35 yr should be screened every 5 yr |
| U.S. Preventive Services Task Force | Insufficient evidence for or against screening |
| Institute of Medicine | Screening not cost-effective in Medicare population |
The American College of Physicians (ACP) has recommended that women older than 50 years with one or more general symptoms that could be caused by thyroid disease should be screened with serum TSH testing initially, followed by measurement of free T4 if the TSH level is undetectable or greater than 10 mIU/L.27 The American Academy of Family Physicians (AAFP) has recommended routine thyroid function screening in asymptomatic patients older than 60 years.28 The American Thyroid Association (ATA) has recommended screening in all adults beginning at age 35 years and every 5 years thereafter.29 The American Association of Clinical Endocrinologists (AACE) has recommended routine measurement of TSH in older patients (age not specified).29 In contrast, the U.S. Preventive Services Task Force (USPSTF) has not recommended routine screening for thyroid disease in children or adults,30,31 and the Institute of Medicine has issued a statement that screening is not cost-effective in the Medicare population.32
Hyperthyroidism
Hyperthyroidism, or overactive thyroid, is a condition that involves excess synthesis and secretion of the free thyroid hormones, T3 and/or T4, by the thyroid gland, leading to the hypermetabolic condition of thyrotoxicosis. It can be primary, indicating thyroid gland pathology, secondary, indicating stimulation of the thyroid gland from excess TSH, or tertiary, indicating excess thyrotropin-releasing hormone (TRH; rare).
Epidemiology and Pathophysiology
The prevalence of hyperthyroidism in older adults is estimated to be 0.5% to 4%.32 Even though Graves disease still remains the most common cause, the prevalence of multinodular goiter and toxic nodular adenomas tends to increase with age.33,34 All can present as apathetic thyrotoxicosis.35 Graves disease is an autoimmune disorder that results from the stimulatory effects of thyroid receptor antibodies (also known as thyroid-stimulating immunoglobulins) on the thyroid gland. These antibodies stimulate thyroid gland growth and thyroid hormone synthesis and release.36 Multinodular goiters are common in older adults and may not always be clinically obvious.37 It has been observed that long-standing euthyroid multinodular goiters can undergo changes and insidiously become toxic, with overproduction of thyroid hormones.38 A less common cause of hyperthyroidism in older adults is toxic adenoma. This is usually found on thyroid scintigraphy as a solitary hyperfunctioning nodule with suppression of activity in the remaining thyroid gland.39,40 Toxic multinodular goiter and toxic adenoma are due to focal and/or diffuse hyperplasia of thyroid follicular cells, whose functional capacity is independent of regulation by TSH.
Hyperthyroidism can also rarely occur in a previously euthyroid person following exposure to iodine-containing substances. Ingestion of iodine can lead to hyperthyroidism in areas of iodine deficiency, especially in persons with a nodular goiter.41,42 Following an increase in iodine supply, underlying areas of autonomy within the thyroid gland produce thyroid hormone independently of normal regulatory mechanisms (Jod Basedow phenomenon), leading to hyperthyroidism.43 This is usually a self-limiting disorder lasting several weeks to several months.44 Usually, this occurs following administration of iodinated contrast radiographic agents or exposure to iodine-rich drugs, such as amiodarone.45 Up to 40% of persons taking amiodarone will have serum T4 levels above the normal range, but only about 5% will develop clinical hyperthyroidism.46 Amiodarone is fat-soluble and has a long half-life, so amiodarone-induced hyperthyroidism can last for months and is difficult to treat.47,48
Iodine-induced hyperthyroidism is particularly important in the geriatric population because the prevalence of thyroid nodular disease is higher in older than in younger patients, clinical detection of hyperthyroidism is more challenging, and older adults are more likely to have underlying heart disease.43,49 The risk of iodine-induced hyperthyroidism should always be considered in older patients with known multinodular goiter and/or subclinical hyperthyroidism (see later), and alternatives to imaging with contrast should be pursued when appropriate.
Moreover, the possibility of hyperthyroidism must always be considered in the elderly person who is receiving thyroid hormone, especially if the dosage is greater than 0.15 mg of L-thyroxine daily. Patients who have received such dosages for many years without evidence of hyperthyroidism may insidiously develop features of hyperthyroidism as they age past 60 years because of age-associated slowing in thyroid hormone metabolism.50
Rare causes of hyperthyroidism in older adults include TSH-producing pituitary tumors51,52 and ectopic TSH production by nonpituitary tumors. These can be recognized by the finding of unsuppressed levels of serum TSH in the presence of increased amounts of circulating thyroid hormone. Additional uncommon causes of hyperthyroidism include overproduction of thyroid hormone by metastatic follicular carcinoma and thyroid hormone resistance.
Transient hyperthyroidism may occur in patients with subacute thyroiditis as a result of increased leakage of thyroid hormone into the circulation during the inflammatory phase of the illness.53 Similarly, radiation injury to the thyroid can be accompanied by a transient increase in circulating thyroid hormone levels with associated symptoms.
Subclinical hyperthyroidism (low or suppressed TSH levels, with normal free T4 and normal free T3 levels) is more common than overt hyperthyroidism in older adults. It is estimated to have a prevalence of 3% to 8%.54–56 It is more common in women than men, especially in patients older than 70 years,57 smokers, and areas of the world with mild to moderate iodine deficiency.18,58 In a study of the natural history of subclinical hyperthyroidism in female patients 60 years of age and older (N = 102), the progression to overt hyperthyroidism was infrequent, at 1%/year.59
Clinical Presentation
Two thirds of older adults with hyperthyroidism present similarly to younger patients.60 Symptoms are consistent with sympathetic overactivity and include tremors, anxiety, palpitations, weight loss, and heat intolerance. Clinically detectable thyroid gland enlargement (goiter), present in almost all younger patients, is absent in as many as 37% of older patients with Graves disease.38 Lid lag and lid retraction are frequently seen.35,38,60–62
One third of older adults will present with apathetic hyperthyroidism.35 The paucity of clinical signs and symptoms of hyperthyroidism in older adults has been confirmed by several studies,60,63–66 with weight loss, apathy, tachycardia, and atrial fibrillation the most commonly occurring symptoms (P < .001). However, tachycardia is absent in up to 40% of older hyperthyroid patients, primarily due to coexisting cardiac conduction system disease.64 Progressive functional decline, muscle weakness with wasting, and depression could also be presenting features in older adults.38 A large cross-sectional study (N = 3049) has shown an increased prevalence of weight loss in older patients (>61 years) and identified shortness of breath as a symptom commonly reported in older adults (P < .001). This study also demonstrated a higher proportion of older adults reporting only one or two symptoms, versus five or more in the younger patients.66 Deep tendon reflexes are often not hyperreflexic. The absence of classic symptoms and signs in older adults presents a diagnostic challenge and may lead to delay in treatment and worse outcomes.60,66 Often, the initial impression in such patients is that of depression, malignancy, or cardiovascular disease.35,63
Patients with subclinical hyperthyroidism have no or very mild clinical features suggestive of hyperthyroidism.67 However, these patients are at increased risk of developing atrial fibrillation, increased cardiovascular and all-cause mortality, accelerated bone loss, and impaired quality of life.24,68–72
Diagnosis
The diagnosis of primary hyperthyroidism is based on thyroid function test results. As in younger patients, the initial diagnostic test for suspected hyperthyroidism in older adults is a serum TSH. Free T4 and free T3 levels should also be measured if the TSH level is low or suppressed. However, hospitalized elderly who are acutely ill may demonstrate a depressed TSH without actually being hyperthyroid. A low or suppressed serum TSH level with a high free T4 and/or high free T3 level indicates overt primary hyperthyroidism. A low serum TSH level with normal free T4 and free T3 levels indicates subclinical hyperthyroidism. Demonstration of anti-TSH receptor antibodies can be helpful in making a diagnosis of Graves disease.73,74
In a small proportion of cases of hyperthyroidism, measurement of serum thyroid hormone concentrations results in the expected increase in the serum T3 level but with the finding that the serum T4 level is within the normal range, although often at the upper end. This condition has been termed T3 toxicosis and can occur with any type of hyperthyroidism, but is found more commonly in older patients with toxic multinodular goiter or solitary toxic adenoma.40
When the clinical presentation of thyrotoxicosis is not diagnostic of Graves disease, a radioactive iodine uptake should be performed to help determine the cause. A thyroid scan should be added if thyroid nodules are also identified.6
Risks, Complications, and Sequelae
Atrial Fibrillation
It has been clearly demonstrated that age is independently associated with an increased risk of developing atrial fibrillation. Atrial fibrillation is estimated to be present in up to 20% to 35% of older patients suffering from hyperthyroidism59–60,75 and is especially common in those with hyperthyroidism secondary to toxic nodule(s).60 Long-standing low serum TSH concentrations in older patients are associated with a threefold increased risk of developing atrial fibrillation.69 In a population-based study, euthyroid individuals with a TSH level in the lowest quartile had a higher risk of atrial fibrillation than those in the highest quartile.76 Because of the greater incidence of underlying cardiac disease, the risk of developing atrial fibrillation is increased in patients older than 60 years. Atrial fibrillation in older adults may sometimes be the only clinical sign of hyperthyroidism. However, the degeneration of the sinus node and fibrotic changes in the cardiac conduction system make the presence of palpitations less likely in this population. In addition, frequent use of β-blockers or amiodarone in these patients can mask the arrhythmia. In contrast, younger hyperthyroid patients often present with sinus tachycardia.66 Many older adults with hyperthyroidism and atrial fibrillation are at increased risk for thromboembolic events, especially those with a prior history of thromboembolism, hypertension, or congestive heart failure or who have evidence of left atrial enlargement or left ventricular dysfunction.77
Cardiovascular Effects and Mortality
Thyroid hormones act on the myocardium to sensitize the heart to β-adrenergic stimulation, with a resultant increase in heart rate, stroke volume, cardiac output, left ventricular mass, ejection fraction, and shortened left ventricular ejection time.77–79 Overt hyperthyroidism, and less often subclinical hyperthyroidism, can be accompanied by several cardiovascular changes, including widened pulse pressure, increased systolic blood pressure, exercise intolerance, increased risk for atrial fibrillation, exacerbation of angina in patients with preexisting coronary artery disease, increased cardiac mass, and precipitation of congestive heart failure, which responds less readily to digoxin treatment because of increased renal clearance of the drug.80
Echocardiographic data further define the cardiac changes in hyperthyroidism. Specifically, it has been demonstrated that diastolic function is enhanced, as evidenced by increased isovolemic relaxation and left ventricular filling in hyperthyroid patients.81 These alterations in hemodynamic parameters may explain many of the cardiovascular signs and symptoms of hyperthyroidism and many of the cardiac complications associated with hyperthyroidism, including decreased exercise tolerance and increased risk of congestive heart failure.
Several cross-sectional and case-control studies have found that decreased levels of serum TSH are associated with increased cardiovascular mortality in older adults.82 Collet and colleagues have demonstrated an increased risk of total and ischemic heart disease mortality when the TSH level is lower than 0.10 mIU/L in patients with endogenous subclinical hyperthyroidism.83 In addition, subclinical hyperthyroidism has been shown to be associated with left ventricular hypertrophy, which is a predictor of cardiovascular mortality.80
Osteoporosis and Fracture Risk
Overt hyperthyroidism is a well-recognized risk factor leading to low bone mineral density and osteoporotic fractures, especially in older women.84 This is critical because hip fracture mortality rates within the year of fracture reach up to 37% in older adults.85–88 Thyroid hormone acts on osteoblasts and osteoclasts to increase bone turnover, leading to net bone loss.89 Notably, most studies investigating the relationship between thyroid dysfunction and fracture risk have been specific to women. Bauer and associates, in a large prospective fracture study (N = 686), reported that women older than 65 years with a TSH level of 0.1 mIU/L had a threefold increased risk for hip fracture and a fourfold increased risk for vertebral fracture as compared to euthyroid counterparts.72 In a study of subclinical hyperthyroidism in older adults (mean age, 72.8 years) with gender-specific analyses, men were found to have an increased incidence of hip fractures compared to women (13.8% vs. 12%; P < .01).90
Ophthalmopathy
There have been contradictory studies regarding the association of symptoms and signs of ophthalmopathy in Graves disease with increasing age. Most studies published on this subject have demonstrated a positive correlation between prevalence and severity of ophthalmopathy with increasing age.60,91 However, one prospective cohort study has found infiltrative ophthalmopathy with severe proptosis and exophthalmos to be more frequent in younger patients with Graves as compared to older adults (46% vs. 6%; P < .001).66
Dementia and Cognitive Impairment
Data are also conflicting regarding the link of dementia with hyperthyroidism, but many studies have suggested an association between subclinical hyperthyroidism and increased risk of dementia.92–94 In a prospective study, women with a mean age of 71 years and a TSH level in the lowest tertile had a twofold increased risk of developing Alzheimer disease compared with those in the middle tertile.92 In other studies, subclinical hyperthyroidism with a TSH level less than 0.46 mU/L was associated with cognitive dysfunction and increased risk of dementia.93,95 In addition, it has been shown that a lower serum TSH level within the reference range is independently associated with the risk of cognitive impairment, including mild cognitive impairment and dementia, in older patients.95 There is a lack of evidence suggesting that antithyroid treatment might ameliorate dementia.96
Management
Symptomatic treatment for hyperthyroidism in older adults consists of β-adrenergic blockade. β-Adrenergic blockers act by interfering with some peripheral actions of thyroid hormone but do not correct the hypermetabolic state. They decrease heart rate and systolic blood pressure and can also relieve tremors, irritability, emotional lability, and exercise intolerance. Anticoagulation may be indicated in patients who present with atrial fibrillation. β-Blockers do not interfere with the laboratory assessment of thyroid function and can allow control of symptoms until definitive treatment can be undertaken.
Treatment modalities for overt and subclinical hyperthyroidism are the same. These include radioactive iodine ablation therapy, antithyroid medications, and thyroidectomy.97
Radioactive iodine ablation is often used for older adults because of its efficacy, safety, and cost-effectiveness.98 An appropriate dose is calculated from a thyroid radionuclide uptake and scan obtained prior to radioactive iodine ablation. A drawback to this treatment approach is that hyperthyroidism is reversed gradually over months, and cardiac issues may need to be managed aggressively until the thyrotoxic state is reversed. Over 80% of these patients subsequently develop hypothyroidism and require lifelong thyroid hormone replacement therapy.99 Periodic monitoring of thyroid function is a necessity for any patient treated with radioactive iodine who has not yet become hypothyroid. Side effects of radioactive iodine treatment include dry mouth (xerostomia), metallic taste, salivary gland swelling, lacrimal duct dysfunction and, rarely, secondary malignancy, such as leukemia. Radiation thyroiditis can also rarely occur.
In regard to antithyroid medications, methimazole is preferred. Propylthiouracil is no longer recommended in this setting unless there is an allergy to methimazole due to its black box warning of severe liver injury and acute liver failure, which may be fatal. Antithyroid medications impair the biosynthesis of thyroid hormone and lead to depletion of intrathyroidal hormone stores and, consequently, to decreased hormone secretion. A decline in the serum T4 concentration is usually seen by 2 to 4 weeks after initiation of antithyroid drug therapy; the dose can be tapered once thyroid hormone levels reach the normal range to avoid development of hypothyroidism. However, older adults may be at greater risk of recurrence of hyperthyroidism after drug therapy and for medication side effects.98 Long-term antithyroid drugs are rarely successful in inducing sustained remission in older patients with toxic multinodular goiter. There are data that older adults taking propylthiouracil or high doses of methimazole may be at greater risk for side effects. Agranulocytosis is the major adverse event in this population, occurring in 0.5% of those treated.99 Routine periodic monitoring of the white blood cell count has not been recommended, but measurement is necessary if the patient experiences the onset of fever, sore throat, or oral ulcerations, and the drug must be discontinued if there is evidence of neutropenia.99 Rash, arthralgias, and myalgias also occur more frequently.98
Depending on comorbidities, surgical approaches are less commonly used in older adults with hyperthyroidism due to the perceived increased risk of morbidity.100 They are reserved for large goiters with obstructive symptoms or known or suspected malignancy.101 However, it has been found that thyroid surgery in patients aged 70 years or older is safe, and age alone should not be a consideration factor.102 Possible complications following thyroid surgery include pain, bleeding, infection, vocal cord paralysis due to recurrent laryngeal nerve damage, and hypocalcemia due to hypoparathyroidism (transient or permanent).
Regarding subclinical hyperthyroidism in older adults, guidelines have recommended periodic clinical and biochemical assessment. Recent ATA/AACE guidelines have recommended that patients older than 65 years be treated if their TSH level is lower than 0.1 mIU/L and that treatment can be considered if their TSH level is 0.1 to 0.5 mIU/L.55,97 Treatment modalities include antithyroid drugs, radioiodine treatment, and thyroid surgery, as mentioned earlier.
Hypothyroidism
Hypothyroidism, or underactive thyroid, is a condition in which there is thyroid hormone deficiency (T4 and T3) due to decreased synthesis or tissue unresponsiveness to the presence of adequate thyroid hormone levels. Primary hypothyroidism occurs due to dysfunction of the thyroid gland. Secondary hypothyroidism refers to the inadequate release of TSH from the pituitary gland, causing decreased production of T4 from the thyroid gland. Failure of synthesis or release of hypothalamic TRH leads to rare cases of tertiary hypothyroidism.
Epidemiology and Pathophysiology
Estimates of the prevalence and incidence of hypothyroidism among older adults are variable, depending on the populations studied and criteria used to define the condition.103 A large screening study (N = 25,000) has revealed that 10% of men and 16% of women aged 65 to 74 years had TSH levels above the upper limit of the reference range.104 The most recent National Health and Nutrition Examination Survey (NHANES III) has reported that a significantly greater number of women aged 50 to 69 years met criteria for subclinical and clinical hypothyroidism compared to men in the same age range.18 Moreover, a study evaluating geriatric patients under medical care has demonstrated that 15% of the women and 17% of the men had previously undiagnosed hypothyroidism.105
The incidence of hypothyroidism steadily increases with advancing age, predominantly due to a rising incidence of autoimmune thyroiditis.106–108 In a survey by Reinhardt and Mann, the reported incidence of Hashimoto thyroiditis was 67% in a patient population with a mean age of 73 years (N = 24).109 A survey of endocrinology clinic patients has revealed that 47% of patients aged 55 years and older presenting with primary hypothyroidism had a diagnosis of autoimmune thyroiditis, whereas 27% had postsurgical hypothyroidism and 10% had postradioiodine hypothyroidism.110
Subclinical hypothyroidism is defined as a normal serum free T4 level in the presence of an elevated serum TSH level. The prevalence of subclinical hypothyroidism rises with age, is higher in women than men, and is lower in blacks than in whites.18,104,111,112 The prevalence of subclinical hypothyroidism was reported to be 4.3% in 16,533 subjects from NHANES III.18 In population-based studies, subclinical hypothyroidism prevalence has ranged from 4% to 15%.104,105,111–114
Progression of Subclinical Hypothyroidism to Overt Hypothyroidism
Many patients with subclinical hypothyroidism eventually develop overt hypothyroidism, and the cumulative incidence of overt hypothyroidism ranges from 33% to 55% in prospective studies after a 10- to 20-year follow-up.115–117 In a recent study evaluating 4000 patients older than 65 years, subclinical hypothyroidism persisted in almost 50% of patients at 2- and 4-year follow-up. The highest rates of reversion to euthyroidism were in those patients with lower TSH levels (<7 mIU/L) and a negative thyroid peroxidase antibody titer.118
Clinical Presentation
The onset of hypothyroidism in older adults is insidious, and the development of symptoms may take many years, leading to late recognition of the condition in this population. Hypothyroidism can affect several organ systems, including the cardiovascular system, central nervous system (CNS), gastrointestinal tract, and skin.
The most common cardiovascular manifestations are bradycardia and narrow pulse pressure.77 CNS abnormalities include depression, cognitive impairment, and excessive lethargy. Hypothyroidism has also been studied as a cause of dementia.119 Constipation is seen in hypothyroidism; however, this is also a common symptom in euthyroid older adults. Integumentary changes are comprised of dry skin, yellowing of the skin, face puffiness, periorbital edema, coarsened and thinned hair, thinning of the outer part of the eyebrows, and brittle nails.120 Hypothermia and weight gain or loss may also be seen in older adults.
A high index of suspicion is required for the diagnosis of hypothyroidism in older adults because symptoms and signs such as fatigue, weakness, constipation, dry skin, and cold intolerance may be attributed to other diseases common in older patients, medication side effects, or aging itself.4,121 A prospective study by Doucet and colleagues122 has compared 24 clinical symptoms and signs of hypothyroidism between older (N = 67; mean age, 79.3 years) and younger patients (N = 54; mean age, 40.8 years). It was concluded that the mean number of clinical symptoms and signs in older adults was 6.6 versus 9.3 in the younger population. Fatigue and weakness were the most common symptoms in older adults, whereas cold intolerance, paresthesiae, weight gain, and abdominal cramps were less common.
Diagnosis
An elevated serum TSH level with a low serum free T4 level is indicative of overt primary hypothyroidism. There is no diagnostic value in measuring a serum free T3 level. A low free T4 level with an inappropriately normal or low TSH level indicates secondary hypothyroidism.
Risks, Complications, and Sequelae
Cognitive Impairment
Hypothyroidism in older adults has been associated with impairment of several cognitive domains, including memory, attention and concentration, language, executive function, and perceptual and visuospatial function.123,124 Severe hypothyroidism may mimic depression and dementia. Neuropsychiatric symptoms usually improve with treatment and restoration of a euthyroid state.125 The relationship between subclinical hypothyroidism and cognition is less clear. It has been postulated that older adults may be more vulnerable to the effects of subclinical hypothyroidism, given age-related changes to the hypothalamic-pituitary-thyroid axis. However, several studies in older adults have not shown a significant association between mildly elevated TSH levels and reduced cognitive performance.126,127
There have been conflicting data on the role of levothyroxine replacement in subclinical hypothyroidism and improvement in cognition. Several studies have shown improvement in cognition with levothyroxine replacement therapy,128–130 but others showed no benefit.126,131
Cardiovascular Effects
The cardiovascular consequences of hypothyroidism in older adults are thought to be due to a reduction in stroke volume and heart rate, leading to decreased cardiac output.132,133 Decreased cardiac output contributes to reduced exercise capacity and shortness of breath during exercise. Congestive heart failure and angina can worsen when hypothyroidism develops in patients with preexisting heart disease, which is commonly seen in older adults.
Other cardiovascular effects include increased risk of atherosclerosis, increased arterial stiffness, endothelial dysfunction, and altered coagulation parameters.134 An increase in peripheral vascular resistance can lead to hypertension. All these abnormalities regress with levothyroxine replacement.
In subclinical hypothyroidism, thyroxine therapy can improve cardiovascular risk factors such as dyslipidemia, markers of inflammation, vascular smooth muscle proliferation, vascular reactivity, ventricular function, endothelial function, and carotid intima media thickness, but the data on decreasing cardiovascular events are limited.135–145 The Cardiovascular Health Study cohort has shown that in patients aged older than 65 years, subclinical hypothyroidism is not associated with an increased risk of cardiovascular disease, mortality, or heart failure, although the latter was significantly higher in those with serum TSH levels above 10 mIU/L.68,82 A large prospective cohort of community-dwelling older adults (aged 70 to 79 years) has shown that subclinical hypothyroidism with a TSH level above 10 mIU/L is associated with an increased likelihood of prevalent, not incident, metabolic syndrome.146
Mortality
Some studies, but not all, have shown an increased risk of cardiovascular and/or all-cause mortality in patients with subclinical hypothyroidism. In a recent population-based, prospective cohort study (307 participants aged 85 years at baseline), there was no association of TSH or subclinical hypothyroidism with 3-year mortality in the oldest old.147 Another prospective study of patients older than 65 years with a 7-year follow-up has concluded that alterations in thyroid function test results during hospitalization were associated with long-term mortality in older patients. In particular, low free T4 levels were significantly related to all-cause and cardiovascular mortality.148 On the contrary, a prospective study of older individuals (>85 years) in the Netherlands with untreated subclinical hypothyroidism has shown that they actually had a lower rate of cardiovascular and all-cause mortality when the TSH level was between 4.8 and 10 mIU/L.149
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







