and Winfried G. Rossmanith2
(1)
Lenzkirch, Germany
(2)
Ettlingen, Germany
14.1.1 Kallmann Syndrome
14.1.2 Craniopharyngioma
14.2 Pituitary Defects
14.2.1 Genetic Deficits
14.2.2 Pituitary Tumors
14.3 Thyroid Diseases
14.4.1 Pancreatic Tumors
14.4.2 Diabetes Mellitus
14.5 Adrenal Dysfunctions
14.5.2 Hypercorticism
14.5.5 Aldosterone Deficiencies
The endocrine system is so intimately tied to elementary body functions that malfunctions within the endocrine system are pathogenic and potentially life threatening. To understand human endocrinology, the elucidation of defects is even more required because from the defects the healthy, normal situation might be inferred. If, for example, an enzyme defect inhibits steroid hormone biosynthesis and results in major, fatal imbalances of water homeostasis, we recognize the central role of steroidogenic enzymes for the control of renal functions. Since aromatase mutations not only cause sex reversal, but also lead to growth failures, we perceive the action of estrogen for chondrocyte maturation (see Sect. 11.6.3). Experiments in humans, for example, to knock out target genes by molecular biological means which in mice have given stunning and astonishing results are generally forbidden; therefore, endocrinologists depend on the analysis of genetic variations, even though this may be very difficult in certain situations. Information on genes defects in endocrine diseases will complete the discussion of the endocrine system and its elements, especially with respect to an extended description of genes and their products.
We describe different forms of malfunctions: In the endocrine system, release of hormones might be too high or too low. An untimely release of a hormone might occur and disturb homeostasis. The most frequent faults are oversecretion or undersecretion or tumors of endocrine active cells. Other failures involve autoimmune diseases where the immune systems rejects endocrine cells as “foreign” and destroys them, with the consequence of major endocrine dysfunctions. And there are genetic defects: either inherited or individually acquired. These might result in disturbances of the endocrine circuits presented so far. Some genetic defects give rise to infertility and are not handed down.
Many defects involve the fetus in utero. If elementary functions are blocked, fetal death occurs. In these instances, the analysis of the causes is most often impossible. If maternal hormones, however, can substitute for the lacking fetal ones, the child may survive until parturition. Once the umbilical cord has been cut, the newborn is in mortal danger in congenital adrenal hyperplasia, for example, since no cortisol is provided by the adrenal glands. The lack of aldosterone biosynthesis is as dangerous for the newborn. If identified early, such diseases can be controlled.
Other malfunctions become apparent after several weeks or much later. A growth hormone (GH) deficit is not life threatening but may lead to much reduced growth. When the defect is related to the biosynthesis of GH, recombinant GH can be used as a substitute, and its use may lead to relatively normal growth. The individual is, however, resistant to GH therapy if the GH receptor is defective either by mutations or by deletions of the receptor gene. Here the therapy is inefficient. There are, for example, two murine strains with inherited obesity: In the ob/ob mouse, the leptin gene is mutated. Here obesity is controlled by administration of leptin, and adipose tissue already acquired is removed. In the db/db mouse, however, the leptin receptor is mutated and administered leptin does not change adiposity. In human society adiposity, however, is rarely caused genetically. Not enough exercise or activity and an extremely lipid-rich diet are causal for most of the adiposeness.
Since many genetic defects of the endocrine systems involve the CNS, they might be reflected in mental development of a child.
14.1 Defects in the CNS/Hypothalamus
14.1.1 Kallmann Syndrome
Precursor cells of gonadotropin-releasing hormone (GnRH ) neurons migrate from the olfactory anlage into the preoptic area of the hypothalamus. This migration depends on neuronal cell adhesion molecule . In Kallmann syndrome , this migration does not occur and there is no development of regular functional GnRH neurons. Thus, GnRH release fails to occur, with the consequence of maldevelopment of the gonads (hypogonadotropic hypogonadism ). This developmental failure is often coupled to a subdeveloped or missing olfactory sense (anosmia ).
14.1.2 Craniopharyngioma
Craniopharyngioma is the most frequent tumor in children. Some remnants of Rathke’s pouch develop slowly into a tumor with preferred location at the optic chiasm and the sella turcica, thus before and under the hypothalamus. Although it is benign in origin, craniopharyngioma is listed among malignant diseases since it extends into the hypothalamic and pituitary areas and causes massive disturbances of the endocrine system.
Although there are disturbances of the endocrine system, these are mostly undetected and the tumor is recognized as such when optical malfunctions or behavioral abnormalities are apparent. Treatment involves surgical removal of the tumor, radiotherapy, long-lasting endocrine control, and hormone substitution (Grossman 1992; Gerok et al. 2000).
14.2 Pituitary Defects
14.2.1 Genetic Deficits
The anterior pituitary develops from Rathke’s pouch by time- and space-controlled expression of several pituitary specific transcription factors: Pit1, Pitx1, Pitx2, HESX1, PROP1, LHX3, LHX4, GATA2, SF1, and Egr1. Pitx2 and LHX3 seem to stimulate expansion of the pituitary anlage by activating HESX1 and PROP1, which in turn cooperate to stimulate Pit1. Defects of any of these transcription factors cause pituitary maldevelopment. In empty sella syndrome, cells from the adenohypophysis are found outside the sella turcica and vasopressin/oxytocin release occurs ectopically. This syndrome, in addition, might be caused by necrosis, infarct, or radiation.
In the healthy pituitary, gonadotropic cells develop under the influence of GATA2, SF1, and Egr1, all activated by Pitx2. For the development of somatotropic and thyrotropic cells, Pit1 is activated by Pitx2. Maturation of gonadotropic, thyrotropic, and somatotropic cells and their hormone biosynthesis are under the control of Pitx1.
In cases of combined pituitary hormone deficiency (CPHD), mutations in the following genes have been reported (Achermann et al. 2002):
HESX1. Mutations in this gene are causal for CNS defects and pituitary damage connected with faulty gonadotropin release and reduced GH secretion.
LHX3. If this transcription factor is mutated, patients present with cryptorchism, micropenis, and delayed puberty.
PROP1. CPHD in 50 different families has been linked to mutations of PROP1.
14.2.2 Pituitary Tumors
14.2.2.1 Prolactinoma
A prolactin-secreting tumor is the most frequent cause of prolactin overproduction (hyperprolactinemia ) and the most frequent pituitary tumor. Growth of lactotropic cells because of lack of dopamine control appears causal. This lack of dopamine control may arise by defects of dopamine secretion or by disrupted dopamine transport in the portal system. Patients with hyperprolactinemia present with fertility disturbances: Estradiol and progesterone levels are reduced, and pulsatile follicle-stimulating hormone (FSH) and luteinizing hormone (LH) secretion is affected, and therefore so are spermatogenesis, the menstrual cycle, and oocyte maturation. In addition to headache, galactorrhea is observed in women.
The standard therapy uses a dopamine agonist such as bromocriptine (an ergoline derivative). Surgical treatment is performed when there is resistance to the drug therapy. The tumor is reached through the nose (transsphenoidal surgery) and electively removed. This treatment is most often well tolerated without a prolonged postoperative hospital stay.
14.2.2.2 Corticotroph Adenoma (Cushing Syndrome )
Adrenocorticotropic hormone (ACTH ) biosynthesis and release are controlled by corticotropin-releasing hormone (CRH ). Excessive ACTH release causes Cushing syndrome (see Sect. 14.5). This might be caused by a hypothalamic tumor or hyperplasia of corticotropic pituitary cells. In 4–24 % of transsphenoidally treated patients, the hyperplasia is caused by defective hypothalamic CRH control; more frequent, however, is primary corticotropinoma. There are additional observations where nonendocrine tumors release CRH (paraneoplasia ), causing hyperplastic growth of corticotropic cells.
The surgical removal of ACTH-secreting pituitary tumors is the therapy of choice.
14.2.2.3 Somatotroph Adenoma (Acromegaly )
GH synthesis and release are stimulated by GH-releasing hormone (GHRH ) and are inhibited by somatostatin (see Sect. 4.4). Acromegaly is most often caused by a GH-secreting tumor, and thereby through enhanced secretion of insulin-like growth factor 1. Rarely, acromegaly is initiated by a GHRH-secreting hypothalamic tumor. Indications for acromegaly are changed modified facial features—for example, brow protrusion, lower jar protrusion, or teeth gapping.
Occurring before puberty , this tumor results in giantism . As a result of this and any other sufficiently large pituitary tumor, the optic nerve might be influenced, with impaired vision or a reduced field of vision. Excessive prolactin release (see Sect. 14.2.2.1) and infertility are often linked to acromegaly.
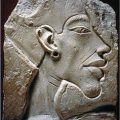
Therapy involves transsphenoidal surgery, radiotherapy, and treatment with somatostatin analogs or a GH receptor antagonist. The long-lasting somatostatin agonist octreotide (Fig. 14.1) has been shown to control GH secretion and thus the tumor in a large number of acromegaly patients.
Fig. 14.1
Long-lasting somatostatin agonist: octreotide
14.2.2.4 Gonadotroph Adenoma
Tumors of gonadotropic cells are rare, and were described first in 1974. Gonadotropic cells secrete LH and FSH controlled by periodic secretions of GnRH . The two subunits of the glycoprotein hormones (α chain and β chain) are normally found in equal numbers in serum. Patients with gonadotropinoma , however, have an increased proportion of the α chain. In male patients, the tumor presents with enlarged testes and an extension of the seminiferous tubules. In women, owing to persistent stimulation of the ovaries, the menstrual cycle is disturbed.
Surgical removal is the therapy of choice since expansion of this tumor might cause visual impairment.
14.2.2.5 Thyrotroph Adenoma
For this very rare tumor, two variants can be distinguished: primary adenoma and the so-called feedback adenoma . The former causes hyperthyroidism —excessive release of thyroid hormone (see below); the latter is caused by strongly reduced or missing levels of thyroid hormones. Feedback adenomas occur since suppression of thyrotropin-releasing hormone (TRH) or thyroid-stimulating hormone (TSH) release is not inhibited by circulating thyroxine. Thyrotropic cells thus are not blocked, synthesize TSH, and proliferate. Feedback adenomas react to thyroxine by stopping TSH synthesis, and thus are easy to treat. Primary adenomas, however, have to be treated by surgery, chemotherapy, or radiotherapy.
14.2.3 Disturbances of Water Homeostasis
Water homeostasis is controlled by a complex network of hormones: vasopressin , whose release is controlled by osmoreceptors via the osmolarity of blood, initiates by enhancing water renal resorption renin release, which in turn stimulates aldosterone synthesis and release. In the kidney, expression and localization of aquaporins and sodium transporters are tightly regulated. Central neuronal networks measuring and setting dilatation or constriction of arteries, and pressure sensors in carotids or in the aortic arch and atrial myocytes estimating the vessel volume or by release of atrial natriuretic peptide as a vasopressin antagonist contribute to this regulation. Centrally triggered is the thirst which makes us drink and which is triggered by changes of osmolarity.
Disturbances of water balance cause polyuria , which is identified by enhanced and salt-deprived urine excretion (insipidus in “diabetes insipidus” means tasteless, sallow urine).
The cause of central diabetes insipidus is insufficient or totally lacking vasopressin biosynthesis in the hypothalamic neurons. Genetic modifications might be inherited or acquired and might be linked to other diseases: diabetes mellitus (DM), visual impairment , or deafness (Wolfram syndrome) . Diabetes insipidus might also occur as a consequence of other illnesses such as trauma, tumors, or infections. In nephrogenic diabetes insipidus , vasopressin binds in the kidney to the vasopressin receptor, which in turn stimulates adenylate cyclase and thus increases intracellular levels of cyclic adenosine monophosphate (cAMP ). This increase of cAMP concentration is lacking in some patients; in other patients, cAMP levels increase, but the following events are inhibited. Apart from genetic defects, metabolic anomalies (increased or diminished calcium concentration), drug use (e.g., lithium salts), sickle cell anemia, and chronic nephropathies have been reported as causal.
Primary polydipsia is characterized by insatiable thirst—patients drink much more liquid than is physiologically required. As causal for this disease, psychotic conditions (e.g., schizophrenia) have been observed.
Apart from diabetes insipidus, there are patients where the serum sodium concentration is abnormally enhanced (above 140 mmol/l). Such hypernatremia might occur after taking an emetic or certain baby food, or after sodium bicarbonate infusion following cardiac arrest. Insufficient water uptake has been observed in cases of pituitary tumors, aneurysms, shock or hydrocephalus, or when movement is limited because of apoplexy or after vomiting, diarrhea, or severe burns, all combined with enhanced liquid loss.
14.3 Thyroid Diseases
14.3.1 Lack of Thyroxine Synthesis: Hypothyroidism
This disease manifests itself by slowing down all metabolism without any apparent involvement of the thyroid gland. A rapid diagnosis, however, is of utmost importance before other failures occur. This is particularly relevant in the diagnosis of inborn hypothyroidism, where genetic deficits block thyroxine synthesis. When the malfunction is diagnosed early, if thyroxine is administered, the imminent consequences such as cretinisms , growth retardation, and mental retardation can be blocked.
In adults, hypothyroidism manifests itself as dry skin, feeling cold more frequently, adding weight, or reduced activity. In the attempt to compensate for the thyroid hormone deficit, a goiter develops: Since thyroxine (and deiodothyronine) does not inhibit TRH and TSH release from the hypothalamus and the pituitary, respectively, the thyroid gland is persistently stimulated. Such stimulation leads to cellular proliferation. A similar phenomenon occurs in the case of iodine deficiency: all enzymes are functional, but cannot act since the iodine uptake does not suffice for the necessary thyroxine amounts.
Today, iodine deficits can be estimated from urine. By use of iodinated salt, iodine deficiency can be avoided.
Apart from iodine deficits, hypothyroidism might be caused by enzyme defects—of thyroid peroxidase or deiodinase—by mutations of TSH or the TSH receptor , and also by inherited errors of the nuclear thyroid hormone receptor.
Finally, the disease might be caused by an autoimmune reaction where antibodies against thyroid peroxidase block thyroxine synthesis and cause tissue destruction.
14.3.2 Thyroxine Excess: Thyrotoxicosis
If the serum thyroxine content is much enhanced compared with that of healthy individuals, the disease is called thyrotoxicosis (Basedow disease , Graves disease, Flajani disease). The cause is an enhanced stimulation of thyroid cells via the thyrotropin receptor. This stimulation may be due to pathologically increased levels of TSH, which in turn can be caused by a thyrotroph adenoma. Thyroiditis may also transiently cause thyrotoxicosis. Adenoma of thyroid cells is an additional potential cause, as are antibodies against the TSH receptor which trigger cells to enhance thyroxine synthesis and cellular proliferation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree