Discovery and Control of the HIV/AIDS Epidemic among Plasma Donors in China
Outline
Late 1994 into early 1996 was the beginning of an HIV/AIDS epidemic in some regions of central and eastern China among plasma donors. The height of the prevalence and the extent to which certain areas suffered from the epidemic was extraordinary in the history of the global HIV/AIDS epidemic. The epidemic became a very sensitive issue for China because it was contamination of the plasma collected at plasma donation sites that caused the disturbingly high rate of HIV infection in these areas. While early reports indicated that the epidemic was a serious one, they did not provide an estimate of the actual number of the infected cases. A large-scale epidemiological and serum testing survey was carried out among plasma donors in 1996, and the prevalence of HIV infection was found to be approximately 12.5%. The survey showed that the rate of infection was related to the frequency of plasma donation. Eight years later, HIV antibody testing was conducted among some 260,000 former paid blood/plasma donors in Henan Province between June and August 2004 and the average HIV prevalence was found to be 8.9%. Following this, the Ministry of Health launched a full-scale, nationwide HIV screening campaign among former paid blood/plasma donors in October 2004. At present, a fairly clear picture has been established of the prevalence of HIV/AIDS among the former paid blood/plasma donors, and treatment and other health care services are being implemented.
In the mid-1990’s, China’s HIV/AIDS epidemic exploded after contamination of the plasma donation supply in central China, especially in the provinces of Anhui, Hebei, Henan and Shanxi etc. Some villages reported such a high prevalence of HIV that they came to be known as “AIDS villages”. This article reviews the process of the discovery of this epidemic, the ensuing survey and prevention and control measures that were taken to mitigate the epidemic among the plasma donors.
1. Plasma Collection and the Emergence of the Blood/Plasma Economy
Plasma collection is a process in which blood is drawn from a donor and the plasma is separated by centrifugation to make biological products. This collection method began abroad in the 1940s and was popular until the 1970s.[1] In 1979, Professor Juanxiang Liu advocated the plasma collection method in China and the Ministry of Health officially approved its use. In 1982, the First National Workshop on Plasma Donation Experience Exchange was held by the Ministry of Health, and the use of plasma collection was promoted all over the country. People were worried, however, that the hurried promotion of this collection method would cause some safety issues. In 1984, the Ministry of Health arranged for Professor Juanxiang Liu and other experts to visit 22 plasma collection centers in 8 provinces, and a handbook, the Manual of Plasma Collection, was developed to standardize the process of the plasma collection. This was all done in order to ensure the well-being of the plasma donors,
the plasma recipients, and the staff working at plasma collection centers.[2]
the plasma recipients, and the staff working at plasma collection centers.[2]
Around the same time as plasma donation was introduced to China, the country ended its paid blood donation system and opted for an unpaid system. This was after nearly 30 years of instituting a paid system and the new system did not meet with much success because people had a difficult time understanding the point of the new system and did not readily accept it. As a result, paid blood donation persisted throughout the country. However, local supply could not meet demand. Almost all clinical blood products used at that time were imported because there were very few blood product enterprises in China. Then, in the early 1980s, the Ministry of Health, the Ministry of Foreign Trade and the China Quarantine and Customs Bureau jointly issued several notices banning the importations of blood and blood products, including plasma, albumin prepared from human plasma, and globulin.[3,4 and 5] This was in an effort to prevent HIV transmission through blood products. Given the existing reluctance to donate blood or plasma, the new regulations resulted in a shortage in the domestic supply of blood products. Thus, a blood/plasma economy emerged in the early 1990s. This was helped by increased importation of foreign capital, technology and equipment needed to establish blood product enterprises. Plasma collection centers sprang up all over the country as raw material providers, and this so-called blood/plasma economy came to be regarded as a kind of tertiary-industry which could help peasants make money, particularly in some poor areas. For example, at the peak of the industry, there were more than 200 registered plasma collection centers in Henan Province, and among which more than 30 were located in Zhumadian District.
2. Contamination of the Blood Supply and the Discovery of HIV among Donors
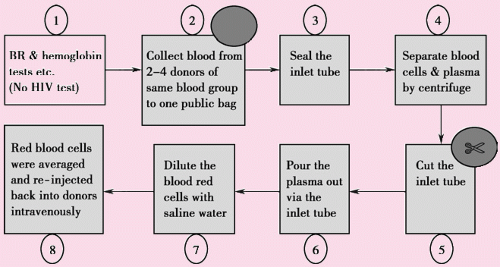
Plasma collection comes with strict regulations, some of which are geared towards the donors themselves, such as how much plasma can be donated each time and how frequently an individual can donate.[1] In practice, however, many issues arose such as poor monitoring of adherence to the regulations by the collection centers and the donors. In order to promote the local economy, the local governments approved as many blood collection centers as possible and did not give due attention to the proper management of each site. Many collection centers focused on increasing profit margins and operated without respect to regulations and without regard for the safety of the donors. The process of blood collection in some of the illegal blood centers was done in very poor conditions, and the blood collection was often done in the donor’s home or even at the edge of the field where he/she worked. The donors did not undergo any testing before the blood collection. One blood bag had only one inlet tube, sealed using a hemostat. Ten shares of blood, collected from ten different donors, were injected into one blood bag. These ten shares of blood were then centrifuged to separate the plasma, the inlet tube was cut and the plasma was poured into a public plasma bag and sent to a biological products company as raw material. To prevent anemia in the donors, the rest of the red blood cells would be diluted with saline water and re-injected back into the donors intravenously- a process known
as plasmapheresis. Some blood collection center owners collected 450ml or 500ml of whole blood in one 400ml blood bag. Then the blood bags of same blood type were pooled into one big public blood bag for centrifugation. None of the equipment was disinfected during the procedure. One blood bag had only one pipe acting as both an inlet and an outlet, and many different donors used one public blood bag. All these factors easily facilitated contamination of the equipment with blood-borne diseases, including HIV.
as plasmapheresis. Some blood collection center owners collected 450ml or 500ml of whole blood in one 400ml blood bag. Then the blood bags of same blood type were pooled into one big public blood bag for centrifugation. None of the equipment was disinfected during the procedure. One blood bag had only one pipe acting as both an inlet and an outlet, and many different donors used one public blood bag. All these factors easily facilitated contamination of the equipment with blood-borne diseases, including HIV.
2.1 Identification of the first case and investigation
In September 1994, a feedback report from a random quality assurance survey by the Shanghai RAAS Blood Product Company Ltd showed that a plasma donor called Mrs. Cui Li, from Lixin County, Fuyang Prefecture, Anhui Province (now Bozhou Profecture) was HIV positive. The staff of local blood collection center, however, did not pay attention to this report because they did not know what HIV was at that time. In November, the company again informed the Lixin County Blood Collection Center that Mrs. Li’s donation was HIV-positive.
This was the first report of an HIV-positive individual in all of Fuyang Prefecture. In an area with no previous cases of HIV and which had little traffic, how did Mrs. Li become infected?
A research team came to Li’s home to conduct an investigation. All five of the family members were screened for HIV and the results indicated that the two men in the family (father and son) were HIV-negative, while the three women (mother and two daughters) were HIV-positive. Later testing confirmed HIV-seropositivity. These three women were sent to the county hospital for a physical health examination. Both daughters, who were aged 16 and 19 years, respectively, had intact hymens, ruling out the possibility of sexual transmission. Each of the women denied a history of blood transfusion or any physical or dental surgery. Drug use was not popular in the area, and they all denied ever having used drugs. Finally, it was revealed that the three women often sold blood at the Lixin County Blood Collection Center as well as at other nearby blood collection centers. In contrast, the two men had never sold their blood at a collection center. Further investigation revealed that selling blood actually meant selling plasma. So, while none of the women had a history of transfusion, they did have a history of plasmapheresis. Thus, the most likely route of HIV infection was through contamination during the donation process at one or some of the collection centers.
A careful site observation was conducted by the research team, focusing on each step of the plasma collection process and the Lixin center’s facilities. There were many opportunities for contamination to have occurred. For example, equipment, such as scissors, was not sterilized between donations, the blood cells that were contaminated were reinfused into the donors, and many of the staff working at the center had never received any related on-the-job training. Two types of potential contamination in plasma collection procedure are outlined in Figure 13.1 and 13.2.
HIV testing of the plasma stored in the refrigerator at the center revealed that more than 40% was HIV-infected.
In light of all these findings, it was concluded that an HIV epidemic was occurring among the local plasma donors
because of contamination during the plasma collection process. [6]
because of contamination during the plasma collection process. [6]
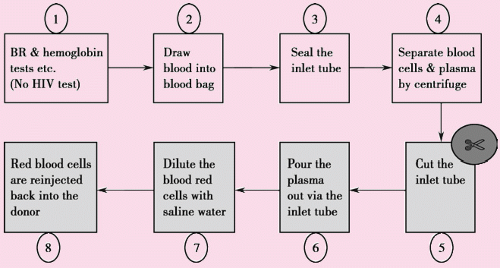 Figure 13.1 Contamination steps of one blood bag for each donor (Step 5, the main contamination step happens when the same pair of scissors is used. Step 7 & 8, another two contamination steps.) |
2.2 Emergency Response
On March 9, 1995, the Fuyang Prefecture Health Bureau issued an urgent notice (Health & Medical No. 35 [1995]) requiring all the blood collection/supply centers, including the blood/plasma collection centers and blood banks, to immediately stop plasma collection.
Almost at the same time, HIV positive individuals were found among the plasma donors in Hebei Province and Henan Province. In February 1995, Mrs. Zhao, a farmer from Yongqing county of Langfang Prefecture, Hebei Province, was found infected with HIV in the First Center Hospital of Tianjin. The local Health Bureau responded by banning all blood/plasma collection/supply activities. In March 1995, Mr. Guo, a donor from Henan Province, was reported HIV positive by the Ministry of Health.
The potential rapid spread of HIV, coupled with such high infection rates in some areas urged immediate action,
as even one day’s delay in closing the donation centers could allow for the probable infection of more than a thousand more people. Thus, it was crucial that all collection centers close immediately and HIV testing be carried out on all blood products to prevent further infections among donors and transfusion recipients.
as even one day’s delay in closing the donation centers could allow for the probable infection of more than a thousand more people. Thus, it was crucial that all collection centers close immediately and HIV testing be carried out on all blood products to prevent further infections among donors and transfusion recipients.
Anhui Province:
On March 13, 1995, an internal telegram ordering the reorganization of the blood supply and collection industry was issued by the Anhui Provincial Health Department. It stipulated that only one blood bank be kept in operation and that all the other blood collection centers should be closed. (No.3 [1995] the Telegram of Health Department).
On March 28, 1995, the Provincial Health Department issued another notice of warning to Shanghai City, Zhejiang Province and Henan Province not to accept blood/plasma collected by some blood/plasma collection centers in Anhui Province. This attracted the attention of Henan government to HIV epidemic among plasma donors. (No.63 [1995] Medical Notice).
On April 6, 1995, a notice suspending plasma collection and supply was issued by the Provincial Health Department to all local governments in the province and to local health bureaus. (No.7 [1995] the Telegram of Health Department).
Hebei Province:
On February 21, 1995, the Hebei Provincial Health Department issued a statement mandating the use of blood tests at all blood collection centers and blood banks before collection from donors. (No.8 [1995] Medical and Health Notice of Hebei Province).
On April 13 1995, the Provincial Health Department issued a notice suspending plasma collection and provision.
Henan Province:
On March 31, 1995, the Henan Province Health Department issued a statement ordering the reorganization and improved management of plasma collection and supply. It mandated that all plasma collection centers be closed.
On May 4, 1995, a meeting was held to discuss the prevention and control of HIV transmission among the former paid blood and plasma donors in Henan, and an urgent report on HIV/AIDS control issued by the Provincial Health Department was sent to local governments requiring all the plasma collection centers in the province be closed (No.37 [1995] Government of Henan Province).
The Ministry of Health:
On March 20, 1995, Regulations for the Management of Blood and Plasma Collection and Supply were issued by the Ministry of Health.
On March 25, 1995, the Ministry of Health ordered all blood/plasma collection and supply centers to close.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree