Fig. 9.1
A large 10cm IDC is occult on 2D mammography but well demonstrated on CEMRI imaging in this woman with dense breasts
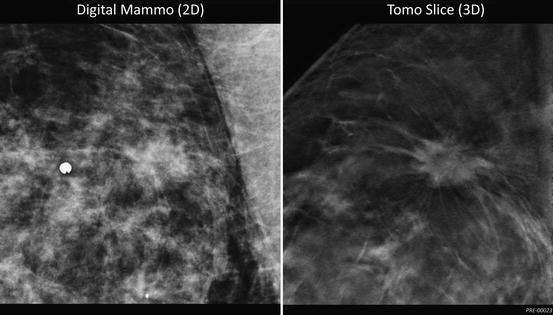
Fig. 9.2
A 2cm. spiculated IDC is partially obscured (by overlying parenchyma) on 2D mammography but is discretely seen on 3D Tomosynthesis
Evidence of Efficacy
DBT has the potential to improve both mammographic sensitivity and specificity in the detection of breast cancer. The current published literature on this emerging technology predominately includes smaller pilot and retrospective studies with enriched data sets. However, at least two large-scale prospective, population-based screening trials are currently underway in Sweden and Norway, with projected completion dates in 2014 and 2015, respectively.
The literature to date shows that the addition of DBT to standard FFDM significantly improves diagnostic accuracy compared to FFDM alone. A recent study by Rafferty et al. comparing FFDM alone to FFDM combined with DBT in 293 cases with dense breast tissue showed that the combined modalities performed significantly better for both calcification cases and non-calcification cases, increasing cancer detection rate and decreasing non-cancer recall rate (Area under the receiver operating conditions (ROC) curve (AUC) equaling 0.94 for 2D + 3D vs. 0.857 for 2D alone [p < 0.0001]) [6]. Similarly, Gur and colleagues found a 16 % improvement in performance for the detection, localization, and characterization of cancer with the addition of DBT to FFDM alone in a study of 125 cancer enriched cases [7]. Early data from a population-based screening study in Norway examining 3,356 cases demonstrated a 47 % increase in cancer detection with DBT in combination with either conventional or synthetic FFDM (created from DBT) compared to FFDM alone [8].
Studies comparing the efficacy of DBT head-to-head with FFDM also suggest superior diagnostic accuracy with two-view DBT. A recently published study by Wallis et al. comparing the two modalities in 130 women, both symptomatic and asymptomatic, found significantly greater accuracy with two-view DBT compared with FFDM, with AUC values of 0.851 and 0.772, respectively [p = 0.021] [9]. Preliminary data from a population-based screening trial in Sweden also suggests higher diagnostic precision of DBT compared with DM [10].
With regards to single-view DBT, prospective studies have shown it is comparable to standard two-view FFDM with regards to diagnostic accuracy [9, 11].
Calcifications
A potential concern with regards to the utilization of DBT in lieu of FFDM for screening purposes relates to both the detection and analysis of microcalcifications. There is limited data on the performance of DBT compared to DM specifically with regards to calcifications. An early investigation by Poplack et al. found that image quality of DBT was inferior to DM in the characterization of calcifications [12]. However, a recent study by Kopans and colleagues found that in 92 % of cases, the clarity of calcifications was felt to be equivalent or better (50.4 % and 41.6 %, respectively) with single-view DBT vs. standard CC and MLO FFDM [13]. Spangler et al. investigated the performance of DBT vs. FFDM with regards to detection and classification of calcifications and found that although FFDM was slightly more sensitive than two-view DBT in detecting calcifications (0.84 % vs. 0.75 %), the diagnostic performance as measured by the AUC was not statistically different (0.76 for DM vs. 0.72 for DBT [p = 0.1277]) [14].
Recall Rate Reduction
In addition to improved breast cancer detection, an additional potential benefit of DBT is a reduction in screening recall rate for non-cancer cases. Current studies indicate that the addition of DBT to FFDM results in a significant reduction in non-cancer recall rate ranging between 28 and 40 % [6, 12, 15], while DBT alone results in a 9.5–11 % reduction vs. DM alone [9, 15]. It should be noted that most of this recall data is derived from retrospective studies with enriched case sets and may not reflect the true performance of DBT in a screening population setting. However, promising preliminary data by Gur et al. from the first 120 patients of a prospective breast cancer screening trial shows a 28 % reduction in recall rate with the addition of DBT to FFDM [16].
DBT Compared to Additional Diagnostic Mammographic Views
Studies comparing DBT to additional diagnostic mammographic views indicate that DBT is comparable in accuracy [17, 18], and equivalent or superior in subjective image quality in 81–89 % of cases [12, 19]. These results suggest that the use of DBT in the diagnostic mammographic workup of patients will result in improved accuracy and workflow efficiency.
Radiation Risk
Modern mammography utilizes very low dose X-ray and even most critics of mammography have stopped using radiation exposure as a reason to avoid mammography. However, as previously described, the current practice in the USA is to utilize DBT in conjunction with 2D FFDM for optimal diagnostic accuracy, which does expose a patient to approximately twice the radiation dose of a 2D FFDM study alone and warrants some consideration.
The FDA mandated MQSA dose limit for mammography is based on the dose delivered to an ACR phantom and is presently 3 mGy. Modern 2D digital mammography units deliver a phantom dose of approximately 1.3 mGy. A combination 2D + 3D tomosynthesis exam delivers a phantom dose of approximately 2.7 mGy, less than the FDA MQSA regulatory limit of 3 mGy for a single 2D exposure but roughly double the dose of a FFDM alone.
The effective dose (measured in milliSieverts) is defined as the dose to the breast normalized to whole body exposure. The effective dose of 2D mammography is approximately 0.5 mSv. A 2D + 3D combination study delivers an effective dose of 1.0 mSv. To put this in perspective, the average annual background effective dose from solar and background radiation is 3 mSv or three times the effective dose from the combination 2D + 3D Tomosynthesis exam. Moving to Denver Colorado from sea level results in an additional 1 mSv of annual background radiation exposure, i.e., twice the dose from a DBT exam. According to the Health Physics Society, “estimation of health risk associated with radiation doses that are of similar magnitude as those received from natural sources should be strictly qualitative and encompass a range of hypothetical health outcomes, including the possibility of no adverse health effects at such low levels [20].”
The mortality risk estimates of the additional radiation exposure associated with DBT are based on worst case (linear no threshold) extrapolations from the known risk at the high doses associated with the nuclear Hiroshima blast. Over the course of their lives, about 375 women out of 3,000 will develop naturally occurring breast cancer. Of these, 125 will prove fatal. At worst, based on the BEIR VII data, annual breast screening from age 40–80 would hypothetically increase breast cancer mortality by about 1 % to 126 for 2D and 127 for 2D plus 3D. This risk is far outweighed by the apparent benefit of digital breast tomosynthesis in diagnosing additional early stage breast cancer and saving lives.
Despite this data on radiation risk, the increased dose associated with a combination 2D + 3D DBT exam has been a source of criticism of the technology. One vendor has now developed a synthetic 2D mammogram, which is created from the 3D projection images. This “synthetic view” obviates the need for the 2D portion of the present combination exam. The dose of the DBT exam is then similar to a present 2D FFDM exam. The synthetic view is presently being utilized on Digital Breast Tomosynthesis systems in Europe, Asia, and Australia and is awaiting FDA approval in the USA.
Challenges with DBT
Image Storage
Tomosynthesis exams are large data sets and require greater storage capacity than conventional full field digital mammograms. It is important to engage your IT department early during planning of tomosynthesis deployment in order to ensure adequate storage capacity and optimal imaging archiving and retrieval. A DBT study is a significantly larger file size when compared to a standard four view 2D mammogram. For example, the currently commercially available DBT system in the USA produces approximately 1GB of data for a 4-view DBT exam. This is stored at a 4:1 lossless compression, meaning the study requires 250 MB of storage space. Currently, the DBT images can be stored on PACS, but in order to be reviewed must be sent to a proprietary workstation. It is expected that this issue will be resolved shortly.
Interpretation Time
While a standard 2-view screening mammogram consists of four total images, a 2-view DBT exam with, for example, a breast that compresses to 4 cm consists of 160 images to review. The amount of time required to interpret a DBT exam as compared to a conventional 2D digital mammogram is therefore receiving significant attention.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree