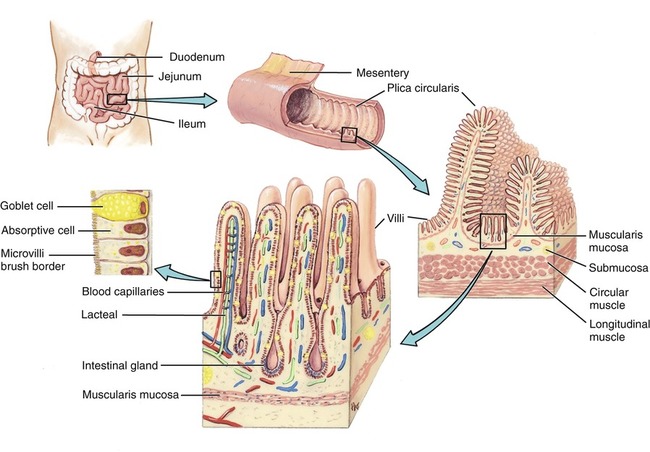
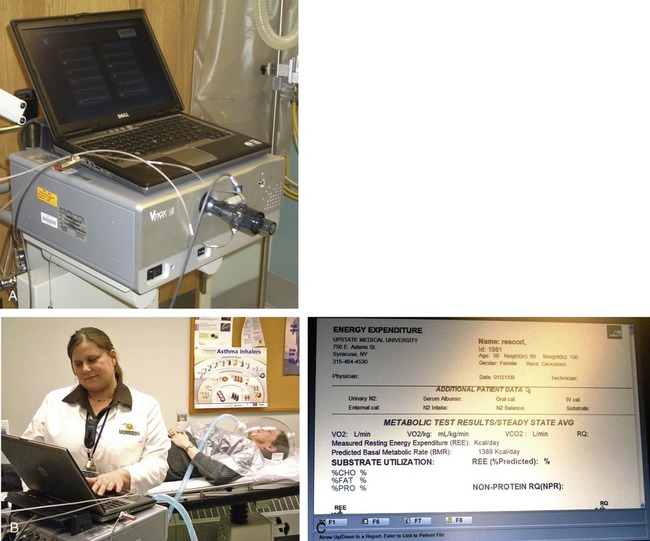
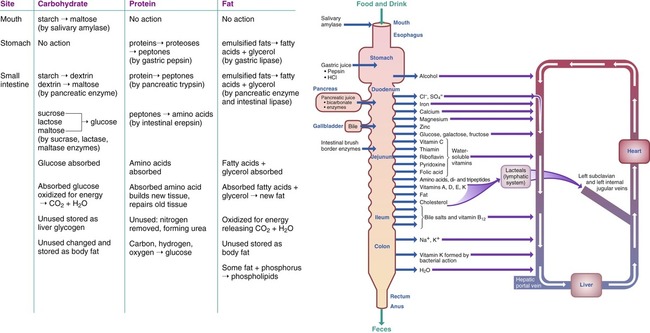
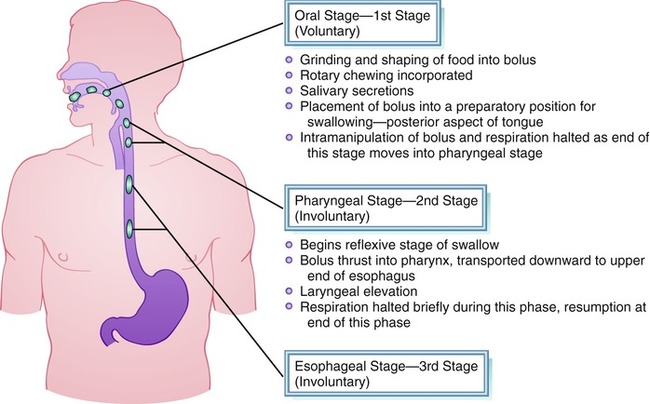
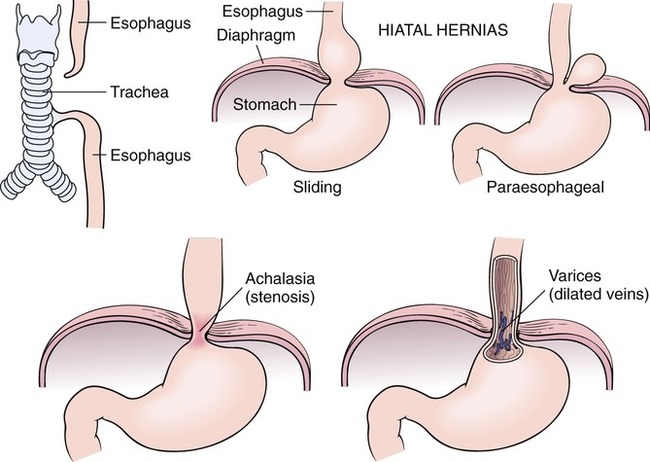
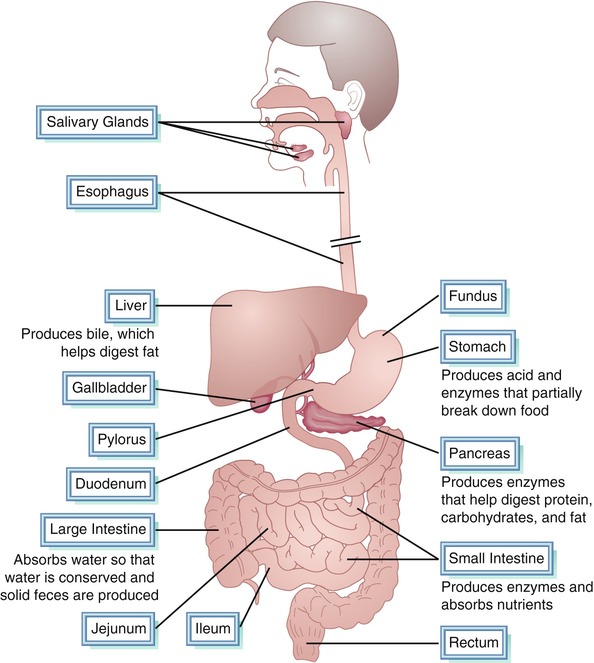
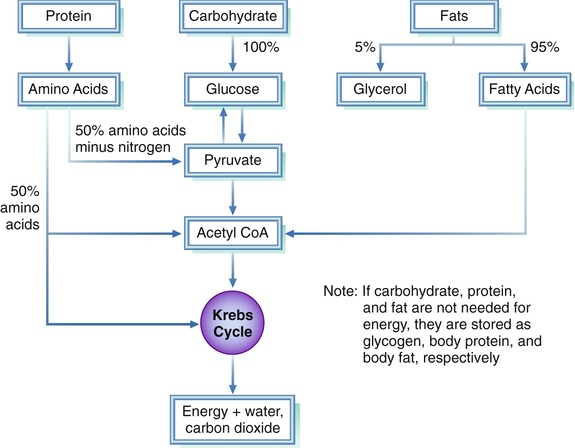
After completing this chapter, you should be able to: • Describe the mechanical and chemical processes of digestion, absorption, and metabolism of foods. • Describe the digestion and metabolism of carbohydrates, proteins, and fats. • Summarize the role of the mouth, stomach, and intestines in the digestive process in health and disease states. • Describe the role of enzymes and the endocrine system in digestion, absorption, and cell metabolism. • Discuss the difference between digestive intolerances and systemic inflammatory allergic reactions. • Describe the metabolism and effect of alcohol on digestion, absorption, and metabolism of food nutrients. • Describe the role of the nurse or other health care professional in aiding the digestive and metabolic processes. Digestion is the change of food from a complex to a simpler form and from an insoluble to a soluble state in the digestive tract. These changes facilitate absorption through the intestinal walls into circulation for eventual use by the body cells (Figure 4-1). The processes of digestion occur simultaneously: 1. Physical (mechanical): During the physical, or mechanical, process, food is broken into small particles in the mouth, then mixed with digestive juices by a churning action in the stomach, then propelled through the digestive tract in rhythmic movements known as peristalsis. 2. Chemical: During the chemical process, digestive enzymes change food nutrients into simple soluble forms that can be absorbed: carbohydrates to simple sugars, proteins to amino acids, and fats to fatty acids and glycerol. This chemical breakdown, called hydrolysis, involves adding water to molecules. Water, simple sugars, salts, vitamins, and minerals require no digestion. 3. Metabolic: During the metabolic process, nutrients are used at the cellular level for basic life processes. The liver plays a key role in the metabolic process, with the reassembly of digested nutrients back into complex molecules and structures. Metabolic enzymes are necessary in this process. Vitamins and minerals are required for metabolic enzymes and hormones to function effectively at the cellular level. A strong correlation between liking sweet foods and cravings for sweets has been linked to genetic factors (Keskitalo and colleagues, 2007). There are genetic differences with bitter taste perception. This difference has been known for decades, and an individual can be described as being a supertaster, taster, or nontaster (El-Sohemy and colleagues, 2007). A study at the Monell Chemical Senses Center in Philadelphia grouped children and their mothers based on their DNA, aimed at studying the effects of a newly discovered taste gene. As a group, it was found the African American children preferred higher-sugar cereals and were more likely to add sugar to their cereals than white children. However, the genetic differences did not bear out with adults, suggesting an environmental override of the need for sweet cereal (Mennella, Pepino, and Reed, 2005). Smell is critical to recognizing the flavors in foods, well known by anyone who has had a head cold and could not breathe through his or her nose. There is also evidence that perception of flavor, based on word descriptors, can influence flavor ratings and appears to correlate with specific regions in the brain (Grabenhorst, Rolls, and Bilderbeck, 2008). Different neurons and regions of the brain respond to different sensory properties of food, including flavor, temperature, and mouth feel (Rolls, 2006). There can also be a physiologic basis for taste preference. Rats, for example, have been found to increase their intake of potassium-based fluids when they are deficient in this mineral (Guenthner and colleagues, 2008). In a study of lambs, their intake of phosphorus-containing foods and water increased or decreased based on their body needs (Villalba and colleagues, 2006). This was later further demonstrated with lambs who were able to discriminate among different-flavored feeds, displaying preferences for calcium and phosphorus ones based on their specific needs (Villalba, Provena, and Hall, 2008). Absorption is the passage of soluble digested food materials through the intestinal walls into the blood, either directly or through osmosis by way of the lymphatic system. The primary site of absorption is in the small intestine. Tiny fingerlike projections called villi, which contain small capillaries (tiny blood vessels), line the intestinal wall. The villi are in constant motion and trap the tiny nutrients, which are then taken in by the adjacent cells and transported through the circulatory and lymphatic system to every body cell. Microvilli are even smaller projections on the surface of the villi (Figure 4-2). All metabolism happens at the cellular level, with the mitochondria acting like small furnaces to burn food energy (catabolism) and allow for anabolism. Food nutrients must enter the body cells in order for the body to metabolize or use these nutrients. It is at the intracellular (inside the cell) level that extremely complex biochemical reactions take place. In fact, through the science of molecular biology it is now recognized that the biochemical processes at the cellular level are so complex, because of multiple pathways of metabolism, that it is highly unlikely they will be totally understood in our lifetime. Good digestion and absorption of food nutrients is, however, essential for proper metabolism at the cellular level. Further, diet quality has an impact. Cellular metabolism is altered in response to the main types of fat: polyunsaturated, saturated, and monounsaturated fatty acids (Khodadadi, Griffen, and Thumser, 2008). A diet high in the fat palmitic acid has been found to lower energy expenditure and fat oxidation compared with a diet high in oleic acid (Børsheim, Kien, and Pearl, 2006). Thus the type of fat may have an effect on weight management (see Chapter 6). Genetic differences also affect the process of metabolism. The basal metabolic rate is influenced by body composition, body size, and age. The more muscle tissue a person has, the more calories are needed. The basal metabolic rate varies from person to person, but on the average it amounts to approximately 1200 to 1400 kcal daily for women and 1600 to 1800 kcal daily for men. Total energy requirements and weight management are discussed in Chapter 6. A simple and relatively accurate method of estimating daily basal metabolism is to multiply weight in kilograms by 0.9 for women and 1.0 for men, then by 24 (the number of hours in a day). This estimate is generally accurate enough, except during times of physiologic stress (see Chapter 15). In large institutions, metabolic carts are used to measure a person’s oxygen intake and carbon dioxide output. This technique can precisely measure the basal metabolic kcalorie needs. Various measurements of oxygen intake and carbon dioxide output have been used over the years to determine basal metabolic rate (Figure 4-3). Carbohydrates (except for fiber) are easily digested, and the degree of absorption is high. Digestion of starch starts in the mouth with the enzyme amylase, also called ptyalin, and is completed in the small intestine. Glucose, which is normally formed from carbohydrates eaten in food, is absorbed into the bloodstream through the walls of the small intestine and is metabolized as shown in Figure 4-4. The monosaccharides glucose and fructose are ready for absorption in the digestive tract because they are single sugar molecules. Double sugars, such as sucrose and lactose, must be changed to simple sugars for absorption, which is a quick process when there is adequate digestive enzyme production. Absorption occurs in the small intestine (Figure 4-5). There is debate on how to precisely define and therefore quantify carbohydrate content on food labels. Around the world there are three different food energy systems used in food tables and on food labels. One suggested descriptive approach suggests noting the difference between metabolizable energy (ME) and net metabolizable energy (NME). This would take into account the amount of carbohydrate able to be digested and absorbed, versus nondigested but fermentable (Elia and Cummings, 2007). The American Diabetes Association advocates subtracting fiber from the total carbohydrate listed on food labels if it is more than 5 g. This is due to an individual basing insulin injections on carbohydrate consumed to avoid developing hypoglycemia (see Chapter 8). The American Dietetic Association promotes subtracting half of the fiber from the total carbohydrates if it is over 5 g, which is more related to kcalorie utilization and not blood glucose outcomes per se. The proteins in the daily diet must be broken down by digestion into the component parts: peptides and amino acids. The mechanical digestive process begins in the mouth through mastication. The chemical digestive process of proteins begins in the stomach and is completed in the small intestines (see Figure 4-5). Hydrochloric acid prepares protein for enzymatic breakdown. The mechanical and chemical processes of protein digestion in particular require the function of an intact neurologic and hormonal response. These responses allow release of digestive enzymes and other substances that allow full digestion and help propel food through the digestive tract. Protease is the enzyme that aids protein digestion. Pepsin curdles milk in the process of milk digestion. In fact, cheese was first accidentally made when milk was stored in the stomachs of animals, before the days of glass, metal, or plastic containers. Trypsin is an enzyme released in the small intestine to help complete protein digestion. It specifically hydrolyzes peptides of arginine or lysine (amino acids; see Chapter 2). Once proteins are digested, absorption into the bloodstream from the small intestine can occur. Amino acids are less well absorbed than peptides. Peptides that are not absorbed are fermented by bacteria in the colon. Fats, because they are insoluble in water, require special treatment in the GI tract before absorption can take place. No digestion of fats takes place in the mouth, and only finely emulsified fats (such as those found in butter, cream, and egg yolk) can start to be digested in the stomach. For the most part, fats must be emulsified by bile (produced in the liver and stored in the gallbladder for use in fat digestion) and bile salts before they are digested in the small intestine by enzymes from the pancreatic juice. Fats are changed to glycerol and fatty acids during digestion (see Figure 4-4). When the body cells need energy, a series of complex metabolic reactions occur: the Krebs cycle (see Figure 4-4, which shows the central pathways of energy metabolism). Oxygen is necessary for the release of energy by the cells in the body. The process of combining oxygen with a molecule is called oxidation. A person needs hemoglobin to supply oxygen to the cells, and a low level of hemoglobin means oxygen is not available for energy production, which results in a tired feeling. An increased intake of air into the body, such as that achieved with aerobic exercise, tends to raise the body’s rate of metabolism through the process of oxidation (see Chapter 6). Physical disorders can begin where digestion starts—in the mouth, or oral cavity. One type of birth defect of the oral cavity is cleft palate (an opening or hole in the roof of the mouth sometimes extending to the lip, which may be referred to as have lip). Babies born with cleft palate have difficulty creating a suction seal around the mother’s nipple or a bottle nipple, which leads to inadequate ingestion of breast milk or formula. Severe cases may require surgical correction. Babies with less severe forms of cleft palate, however, may benefit from special bottle nipples that do not require suction or from a slightly larger hole in the bottle nipple. Mothers who are motivated to continue nursing until the problem is resolved should be encouraged to do so with supplemental bottle feedings as needed (see Chapter 11 for more ideas). Missing teeth, severe dental caries, or ill-fitting dentures can adversely affect food choices. Without adequate nutritional knowledge, omitting food groups may not seem important to a person with dental problems. Alternatives should be discussed, such as eating applesauce in place of fresh apples or eating cooked or soft vegetables in place of raw or hard-to-chew vegetables. Prevention of dental caries is addressed in Chapter 12. Swallowing problems, referred to as dysphagia, are often related to stroke, head injury, cerebral palsy, and other conditions (Figure 4-6). Inability to swallow correctly may result in aspiration of food into the lungs. Aspiration pneumonia is a frequent complication of dysphagia. Dysphagia requires a review of the swallowing process to determine the best means of feeding. A speech pathologist is trained to help assess swallowing problems. An x-ray examination called videofluoroscopy is used in conjunction with a barium swallow to objectively diagnose dysphagia. The swallowing problem is generally at the pharyngeal area. Liquids are usually the most difficult food to swallow for persons with dysphagia. Liquids that are of a nectar consistency can be used for mild swallowing problems, progressing to the thickness of honey, and as needed the thickness of pudding. Liquids can be thickened with a commercial product or with baby rice cereal. Feeding positions can also help (see Figure 15-4 and Table 15-5). Table 4-1 lists a variety of food consistency considerations. See Chapter 15 for institutional issues and guidelines for provision of altered meal consistencies. Table 4-1 Food Consistency Considerations Courtesy of the Occupational Therapy Department of the J.N. Adam Developmental Center, Perrysburg, NY. In achalasia the lower part of the esophagus fails to relax, and swallowing difficulty occurs. The individual senses fullness in the sternal region and may vomit; then there is danger that the contents of the esophagus may be aspirated into the respiratory passages. Weight loss may become a problem that requires nutritional intervention. Dilation of the esophagus or surgical intervention can improve the condition. Including semisolid foods can help a person manage this condition. One case of achalasia was attributed to Wernicke’s encephalopathy (Kennedy and colleagues, 2007). A hiatal hernia is a protrusion of a part of the stomach through the esophageal hiatus (opening) of the diaphragm (Figure 4-7). Persons with this disorder sometimes complain of heartburn because of the reflux of gastric contents into the esophagus. Medical treatment includes ingestion of antacids to neutralize or inhibit gastric secretions and possibly surgery. Small, frequent meals are recommended to reduce symptoms, although dietary modifications cannot eliminate the cause. No food is advised for approximately 3 hours before bedtime, and the person should remain in the upright position after eating. For the obese person, weight loss is indicated to help relieve pressure on the diaphragm. Any source of pressure on the abdomen, such as bandages or clothes that fit too tightly, should be eliminated. A peptic ulcer is an eroded lesion in the lining (mucosa) of the stomach (gastric ulcer) or duodenum (duodenal ulcer). Excess use of nonsteroidal antiinflammatory drugs (NSAIDs) can contribute to the erosion of the mucosal lining. In recent years Helicobacter pylori infection has been increasingly recognized as being involved in the development of peptic ulcers. Symptoms include burning or gnawing pain in the pit of the stomach. While an ulcer is bleeding, no food is allowed; instead the patient may be given intravenous feedings of dextrose and amino acids. As the condition improves, the patient usually progresses from a full liquid diet to a regular diet with the omission of irritants based on individual tolerances. Common intolerances include caffeine, alcohol, and spicy foods, but some individuals have no adversity with these substances (Table 4-2). Table 4-2 Possible Dietary Treatment of Peptic Ulcers* The dumping syndrome is a condition related to stomach surgery. Surgery for ulcers is not uncommon. Obesity surgery may also result in the dumping syndrome (see Chapter 6). In the dumping syndrome the food “dumps” into the small intestine rapidly, causing severe cramping and pain. It has been found that the dumping syndrome may occur even years after gastrectomy (removal of the stomach or portions of it). Hypoglycemia can be a consequence. Individuals presenting with hypoglycemia and a history of stomach surgery may have the dumping syndrome. Seizures resulting from hypoglycemia may occur (Harder and colleagues, 2005). Treatment is aimed at drinking beverages separate from solid foods and consuming low-glycemic-load meals. The condition of gastroesophageal reflux disease (GERD) is the opposite of achalasia, although it may be the cause of the strictures found with achalasia. Esophageal cancer is also related to uncontrolled GERD. In this condition the lower esophageal sphincter is incompetent and allows stomach matter to regurgitate into the esophagus. GERD is considered common in the elderly, but also does occur with young children. It may present various symptoms, such as heartburn, regurgitation, and obstructive sleep apnea (Friedman and colleagues, 2007). Central obesity along with medications and fluctuation of hormonal level may play a causal role. Lowered esophageal sphincter competency has been associated with use of tobacco and intake of alcohol, chocolate, and high-fat meals. Some individuals have appeared to benefit with avoidance of alcohol, fatty foods, chocolate, coffee, mint, and carbonated beverages (Csendes and Burdiles, 2007). However, successful treatment of GERD, as evidenced by reduced acidity level of the esophagus, has only been shown in the research literature with weight loss, remaining upright after meals, and head elevation during sleep (Kaltenbach, Crockett, and Gerson, 2006
Digestion, Absorption, and Metabolism in Health and Disease
WHAT IS MEANT BY THE DIGESTION, ABSORPTION, AND METABOLISM OF FOODS?
WHAT IS BASAL METABOLISM?
HOW ARE THE MACRONUTRIENTS DIGESTED AND ABSORBED?
CARBOHYDRATES
PROTEIN
FAT
HOW ARE MACRONUTRIENTS CONVERTED TO ENERGY?
WHAT ROLE DOES EACH PART OF THE DIGESTIVE TRACT PLAY AND WHAT ARE COMMON ASSOCIATED PROBLEMS?
THE MOUTH
TYPE OF DIET
EXAMPLE
POTENTIAL EFFECT ON ORAL FUNCTION
Thin foods and liquids
Soup broth, juice
More difficult to control within mouth, especially with limited tongue control (i.e., quickly runs to all areas of mouth); often promotes excessive food loss
Thick foods
Pudding, yogurt, applesauce
Improved control within oral cavity because of reduced flow and increased sensory input (i.e., weight and texture)
Pastelike or sticky foods
Peanut butter, thick cheese sauce
May be more difficult to move in oral cavity with limited tongue movement; may stick to the roof of the mouth, especially with a high, narrow palate
Slippery foods
Pasta, Jell-O
Often difficult to control and either triggers reflexive swallow too quickly or runs out of oral cavity before the swallow
Smooth textures
Pudding, pureed foods
Relatively easy to swallow; promotes minimal tongue and jaw movement, especially over time
Coarse textures
Creamed corn, ground foods, Sloppy Joe filling
Increases sensory input to stimulate more jaw and tongue movement; coarseness of food should be carefully graded
Varied textures
Soups with noodles or chunks of vegetables
Difficult to manage in oral cavity, especially with limited tongue movement or decreased oral sensitivity (i.e., liquid is swallowed and solid pieces remain in the mouth)
Scattering textures
Grated carrots, rice, coleslaw, corn bread
Very difficult to manage with limited tongue movement and decreased oral sensitivity
Crisp solids
Carrot sticks, celery sticks
Requires sophisticated biting and chewing to grind pieces into consistency that is safe to swallow
Milk-based substances
Milk, ice cream
Appears to coat mucous membranes in oropharyngeal cavity to interfere with swallowing
Broth
Meat broth, chicken broth
Appears to cut mucus in oropharyngeal cavity and facilitates swallowing
Dry foods
Bread, cake, cookie
May be difficult to chew or swallow with insufficient saliva
Whole, soft foods
Slice of bread
Requires the ability to bite off appropriately sized pieces
THE ESOPHAGUS
THE STOMACH
GUIDELINE
RATIONALE
Eat three regular meals or six small meals
Inhibits stomach distention
Avoid caffeine-containing beverages, decaffeinated coffee
Decreases gastric secretions
Avoid alcohol
Reduces damage to stomach lining
Avoid black pepper, chili powder, cloves, nutmeg, curry powder, mustard seed
Reduces irritation to stomach lining
Avoid aspirin
Reduces irritation of stomach lining
Avoid cigarette smoking
Promotes healing of ulcer
Eat in a relaxed atmosphere
Reduces stress
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Digestion, Absorption, and Metabolism in Health and Disease