Systems
Symptoms of hyperthyroidism
Skin
Heat intolerance, hair loss, hyperhidrosis, urticaria, pruritis, eczema
Cardiopulmonary
Palpitation, exercise intolerance, dyspnoea on exertion, angina pectoris, orthopnoea, obstructive symptoms from enlarged thyroid (dysphagia or breathing difficulty).
Gastrointestinal
Increased bowel frequency from rapid intestinal transit, weight loss from increased caloric requirement, nausea or vomiting (may suggest concurrent pregnancy)
Renal and electrolytes
Polydipsia and polyuria
Reproductive system
Amenorrhea, oligomenorrhea, hypomenorrhea and anovulation, infertility
Neuromuscular system
Tremor, muscle weakness, especially proximal muscle involvement. Less commonly, patients might have bulbar and oesophagolaryngeal muscle weakness presenting with dysphonia, dysphagia and dysarthria. Reversible diaphragmatic weakness has occasionally being reported and presented with dyspnoea [1]
Mental and cognition
Anxiety, irritability, emotional liability, apprehension and difficulty concentrating, shortened attention span, distractibility and impaired short-term memory. Apathetic symptoms are common in the older group such as depression and pseudodementia
It is important to elicit symptoms of thyroid eye disease in patients suffering from thyrotoxicosis as this condition is clinically apparent in 50 % of patients with Graves’ disease [2]. Indeed, this patient admitted that her father noticed her eyes appear to be more prominent but she denied having pain or grittiness in her eyes. Questions addressing the risk factors and potential causes of hyperthyroidism were also explored, as summarized in Box 1.1.
Box 1.1: Risk Factors for Hyperthyroidism
A.
Past medical history of autoimmune diseases (pernicious anaemia, vitiligo, etc.)
B.
Past history of postpartum thyroiditis
C.
Family history of thyroid disease or autoimmune conditions
D.
Medication: Amiodarone, lithium, radiology imaging with iodine contrast, excessive thyroxine replacement
E.
Diet: Excessive consumption of high-iodine content food such as kelp or seaweed
F.
Recent hepatitis B vaccination, recent treatment for chronic hepatitis C (interferon and ribavirin), HIV or with alemtuzumab. This group of patients is at risk of both self-limiting thyroiditis or autoimmune hyperthyroidism (Graves’ disease)
There was no relevant past medical history in this patient. She did not have any previous thyroid disorders or other associated autoimmune diseases. She is a non-smoker with two healthy children aged 6 and 11 years old. Smoking history is particularly important as Graves’ ophthalmopathy is more common among smokers and they seem to respond poorly to treatment compared to non-smokers [3, 4]. Her mother has hypothyroidism and her great grandmother suffered from hyperthyroidism and pernicious anaemia. Her current medication includes Dianette for contraception and oxytetracycline as required for acne treatment.
What signs to look for?
The clinical manifestations of hyperthyroidism are multi-system, mainly caused by the acceleration of various physiological processes in all organs. Nevertheless, most of these signs are non-specific. The frequency and severity of these features vary widely among affected patients, and in rare cases the first presentation may be with life-threatening thyroid storm. The signs to look out for in hyperthyroidism are summarized in Table 1.2.
Table 1.2
Signs of thyrotoxicosis
Systems | Signs of hyperthyroidism |
|---|---|
Cardiovascular | Sinus tachycardia or atrial fibrillation, systolic hypertension with widened pulse pressure, cardiac flow murmur and third heart sounds from high-output congestive heart failure |
Respiratory | Stridor or facial plethora as a result of compression of trachea or vena cava from enlarged thyroid |
Bone | Osteoporosis, osteopenia, occasionally hypercalcaemia |
Skin | Warm, smooth and moist hands, fine hair, alopecia, shiny, soft and friable nails (onycholysis), thyroid acropachy, facial or palmar erythema, hyperpigmentation, telangiectasia, pretibial myxoedema |
Renal and electrolyte metabolism | Hypertension, pedal oedema, nephrocalcinosis, thyrotoxic periodic paralysis (associated with hypokalaemia), distal renal tubular acidosis, proteinuria in patients with autoimmune thyroid disease [6] |
Haematology | Microcytosis, pernicious anaemia, lymphoid enlargement and splenomegaly, and rarely thymic enlargement; thrombocytopenia [7] |
Mental/central nervous system | Tremor, agitation, fidgetiness or hyperactivity, muscle weakness and wasting, hyperactive deep tendon reflex with shortening of relaxation phase |
Eyes | Lid retraction, proptosis, chemosis, plica and conjunctival redness |
Gastrointestinal | Elevated transaminase enzymes, protein-calorie malnutrition and hypoalbuminaemia from severe thyrotoxicosis |
Summarise Key Symptoms and Provide a List of Differential Diagnoses
This case illustrates a 31-year-old lady presented with a 6-month history of significant weight loss, palpitation, hyperhidrosis, agitation and short attention span. Physical examination revealed a diffusely enlarged goitre with bruit, palmar erythema and tremors in both hands. Her pulse was regular at 88 beats per minute and her reflexes were normal. Her eyes appeared to be proptotic, without any dysmotility or redness. All these features are in keeping with thyrotoxicosis and the differential diagnosis include:
Graves’ hyperthyroidism (most likely diagnosis as patient has a diffuse goitre with eye symptoms)
Silent or subacute thyroiditis
Toxic nodular thyroid disease
Factitious thyrotoxicosis
What biochemical and radiological tests are needed to reach a diagnosis?
A comprehensive clinical history and physical examination should be sufficient to confirm thyrotoxicosis in most cases. Nevertheless, it is necessary to make an aetiological diagnosis in all cases in order to plan treatment and assess prognosis.
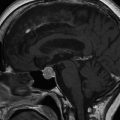
Thyroid status is determined biochemically by the measurement of serum free thyroxine (FT4), free triiodothyronine (FT3) and thyroid stimulating hormone (TSH) concentration. Serum TSH secretion is very sensitive to inhibition by excess circulating thyroid hormones and hence is a remarkably sensitive test for thyrotoxicosis. Importantly, in all cases of true primary hyperthyroidism, the TSH is fully suppressed (i.e., <0.05 mU/l), as non-thyroidal illness and several drugs may commonly lead to low but not suppressed TSH concentrations (0.1–0.4 mU/l) [8]. However, one also has to bear in mind that normal or raised serum TSH levels are found in the rare instances of thyrotoxicosis caused by a TSH-secreting pituitary adenoma or resistance to thyroid hormone. Serum FT3 is the next most sensitive test for hyperthyroidism, and a state of “T3 thyrotoxicosis” is defined by a suppressed TSH with an elevation of serum FT3 but with normal FT4. In evolving hyperthyroidism, serum FT4 is the last to become elevated. Use of modern free thyroid hormone assays has virtually eliminated interpretation problems caused by changes in serum binding protein levels that bedevilled total thyroid hormones assay.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree