Overview
Osteosarcopenia is an age-related syndrome characterized by a low mass of the musculoskeletal unit composed of muscles and bones . Osteosarcopenia was first described in 2009 as the coexistence of osteoporosis/osteopenia (characterized by low bone mass and microarchitectural deterioration of bone tissue ) and sarcopenia (age-related loss of muscle mass, strength, and physical performance ). During the past decade, the negative impact of osteosarcopenia was proven to be more than only the cumulative effect of osteoporosis and sarcopenia (known as a hazardous duet) due to the interaction of their risk factors (including hormonal, nutritional, genetic, and lifestyle factors) . The general consensus on the interaction between sarcopenia and osteoporosis/osteopenia is that it is first the loss of muscle that reduces bone mineral density (BMD) via a reduction in mechanical loading by gravitational forces, which usually stimulate bone formation .
The prevalence of osteosarcopenia
Epidemiological studies examining the prevalence of osteosarcopenia are fairly limited due to the recent origin of this syndrome . The prevalence of osteosarcopenia was estimated to be between 5% and 40% . The varied prevalence is likely due to a non‐unified diagnostic criterion for this syndrome, with various screening tools being utilized for low muscle mass and function (sarcopenia), a key component of osteosarcopenia . A recent study compared the performance of five screening tools for identifying older adults at risk of sarcopenia against five diagnostic definitions . They found the prevalence of sarcopenia varied from 5.7% to 16.7%, depending on the definition. This study suggested using one of these clinical criteria to identify individuals with sarcopenia . The prevalence of osteosarcopenia varies in epidemiological studies due to including heterogeneous populations. For example, the prevalence of osteosarcopenia in people with hip fracture was 27.2% ; however, the prevalence in community-dwelling older adults ranged from 4% to 15.1% . Also, the prevalence of osteosarcopenia appear to vary in different countries; community‐dwelling older adults range from 4.7% in Japan to 13% in China , and 28% in Germany , with the highest rates observed in Australia (40%) and Iran (34%) . Despite the differences in reported prevalence of osteosarcopenia in previous studies, osteosarcopenia is a global health concern and a serious problem in the elderly due to its increasing incidence and the associated unfavorable outcomes .
Impact of osteosarcopenia
With aging of the global population, the impact of osteosarcopenia is increasing . One-year mortality of older adults with osteosarcopenia (15.1%) was higher than people with osteoporosis (4.9%) or sarcopenia only (9.1%) . After adjusting for covariates, osteosarcopenia had a 1.8 times higher mortality rate than nonosteosarcopenia (hazard ratio, 1.84; 95% confidence interval, 0.69–4.92) . People with osteosarcopenia are at a higher risk of falls and fractures . In addition, fracture risk in older men with osteosarcopenia is 3.5-fold higher than having only sarcopenia or osteopenia alone . Compared with the nonosteosarcopenic group, those with osteosarcopenia had greater impairment in physical performance and balance (measured by short physical performance battery and timed-up and go) . With physical performance impairment, osteosarcopenia is associated with a significant physical disability, representing a substantial threat to loss of independence later in life . Indeed, the osteosarcopenic population is at higher risk not only for fractures but also for institutionalization, depression, and impaired mobility and quality of life .
Osteosarcopenia complications are associated with substantially increased morbidity and mortality, placing a significant economic burden on healthcare services . An American study estimated the lifetime attributable cost of hip fracture in an 80 years old community dweller person to be $81,300, and the total yearly cost of all hip fractures in the United States of more than $20 billion . Also, in the United States, another study calculated the direct cost of sarcopenia to be $18.5 billion in 2000, represented by hospitalization, nursing home admissions, and home healthcare expenditure . In Europe, an estimate in 2010 calculated the direct cost of all osteoporotic fractures at €29 billion in the five largest EU countries (France, Germany, Italy, Spain, and the United Kingdom) and €38.7 billion in 27 EU countries . Given the clinical outcomes associated with osteosarcopenia, the diagnosis of osteosarcopenia is imperative to enable clinical care . The diagnosis and screening for osteosarcopenia and hence implementing different prevention and treatment strategies will improve health outcomes and quality of life of older adults.
Osteosarcopenia diagnostic algorithm
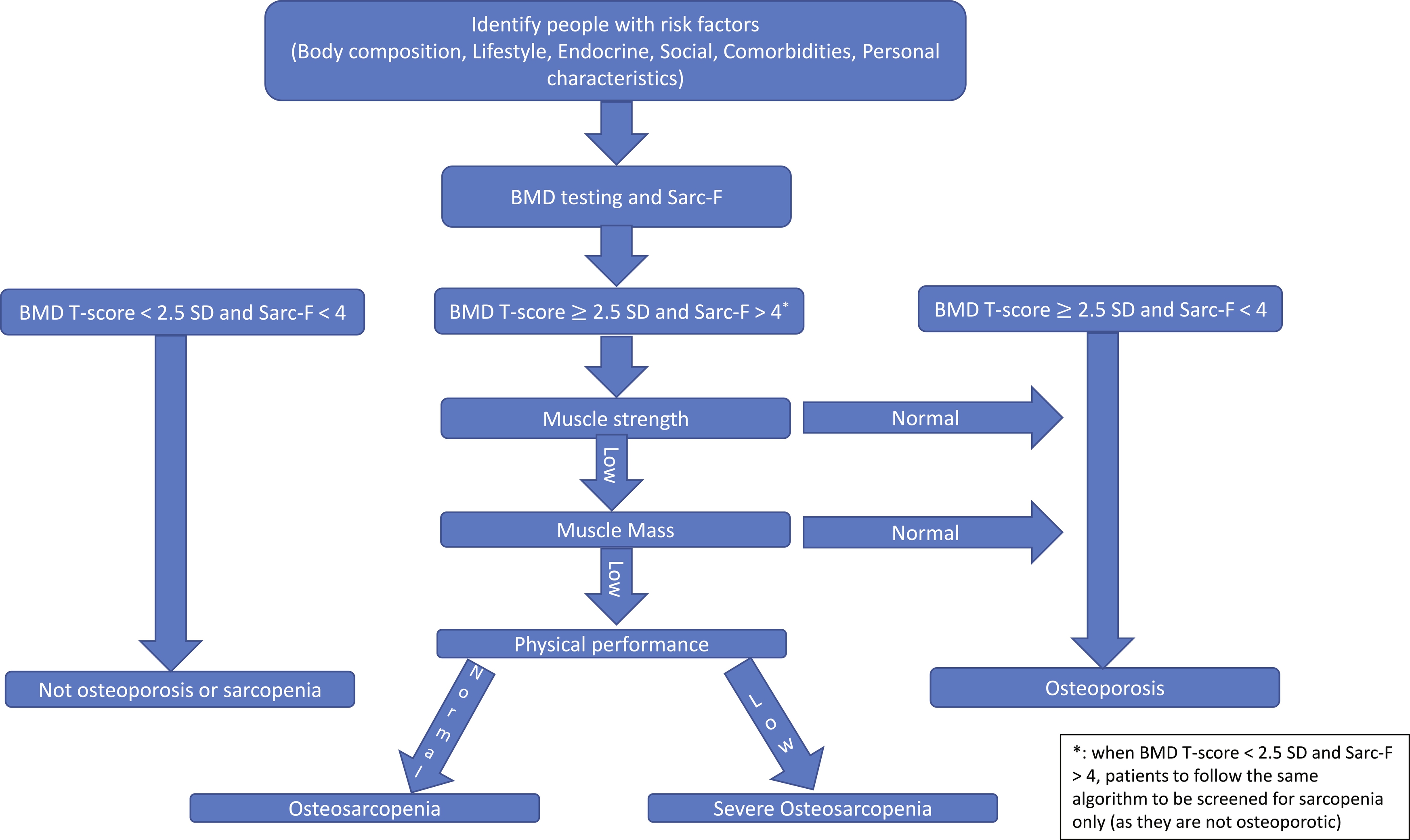
There are several diagnostic and screening tools to identify people with osteosarcopenia; specifically, the sarcopenia component of osteosarcopenia. In this chapter, we are presenting an algorithm to screen and diagnose people at risk of osteosarcopenia. The algorithm is shown in Fig. 1 . We are also describing a number of validated tools to be used in each stage of the algorithm.
Case finding
Early identification of older adults with osteosarcopenia will allow clinicians to implement preventative or intervention strategies and avoid complications. Patients with one or more of the following osteosarcopenia risk factors need to be further screened and tested.
Clinical risk factors
Personal
Age
Sarcopenia and osteoporosis are age-related diseases by definition . The mean age of the subjects with osteosarcopenia is close to 80 years (79–82 years), as observed in most studies. People in this age group have a significant increase in the incidence of fractures. This significant increase is caused by the greater physical functional loss resulting from sarcopenia, and the lower BMD observed in osteosarcopenic patients as compared to older persons with sarcopenia or osteoporosis only .
Sex
Osteosarcopenia occurs more frequently in women than in men. Studies have shown variation between 55% and 65% of prevalence in women . The association with the female is mainly due to the estrogenic deprivation of menopause, which causes a marked decrease in muscle strength in women . The lower muscle strength promotes less mechanostatic action, decreasing the stimulus on bone growth and, consequently, more significant loss of BMD, contributing to the incidence of osteosarcopenia.
Body composition
Obesity
Obesity, i.e., excess body fat, usually defined as body mass index (BMI)⩾ 30 kg/m 2 , is a major public health problem and is well recognized as a risk factor for morbidity and mortality in older adults . Aging is associated with significant changes in body composition with a substantial reduction in fat-free mass and muscle mass and an increase in visceral fat . Given the age-related changes in body composition, sarcopenia often coexists with an increase in fat mass. Visceral fat and muscle mass are known to be interrelated from a pathogenic point of view and are reported to share common inflammatory pathways . In addition, sarcopenia reduces physical activity, resulting in decreased energy expenditure, leading to an increased risk of obesity . Alternatively, visceral fat induces inflammation, contributing to osteoporosis and sarcopenia . The interplay between sarcopenia and rising trends in obesity in an aging population is emerging as a paramount public health concern in the older population. The term sarcopenic obesity was first introduced by Baumgartner and is defined by the combination of sarcopenia and obesity. Obesity and sarcopenia may act synergistically; sarcopenic obesity may have a greater effect on metabolic disorders and mortality, disability, or physical function as outcomes than either obesity or sarcopenia alone . Therefore, screening people with obesity for osteosarcopenia is indicated to prevent unfavorable outcomes of older adults.
Fat infiltration
Since BMI does not distinguish between fat mass and fat-free mass, which have opposing effects on the risk of morbidity and mortality, the use of BMI in older persons may have limitations . Therefore, to fully understand the impact of obesity on older persons, it is essential also to take both fat mass and lean mass into account. Several studies have observed that osteosarcopenic individuals present a high percentage of fat independent of BMI . There is still no consensus as to the percentage of better specificity and sensitivity for these patients. At present, high fat is present when it is above 30% or 40% or the percentage body fat percentage by the squared height is equal to or above the upper quintile of the sample.
Low body weight
Low body weight, defined by low BMI, is associated with sarcopenia . The few studies that evaluated the BMI of older subjects with osteosarcopenia showed that the mean BMI of these individuals is lower when compared to individuals with sarcopenia and osteoporosis only. However, due to the ethnic and gender variety of study populations, there is some discrepancy as to the mean that can best characterize osteosarcopenia, since they ranged from 20.7 (3.5) kg/m 2 in Asian elderly with hip fracture to 27.2 (6.2) kg/m 2 in a population of community-dwelling older persons with a high prevalence of obesity .
Lifestyle
Sedentary lifestyle/poor mobility
Both bone and muscle are adaptive, modifying their mass and strength in response to mechanical loading. Therefore, mechanical stimulus is essential for the health of both tissues, and thus, decreased levels of physical activity may shift the delicate balance in favor of muscle degradation and bone resorption . Physical activity diminishes with aging, with up to 80% of waking hours spent sedentary in older adults , leading to a loss of mechanical loading and associated bone and muscle loss . Low mobility is a prevalent and specific clinical feature among the osteosarcopenic population. The risk of loss of mobility was about three times higher among osteosarcopenic patients than the control group, whereas people with sarcopenia had no significant association with loss of mobility .
Malnutrition
Caloric intake diminishes by around 25% between the ages of 40 and 70 , with reduced vitamin D levels and protein intake correlated with declining muscle strength . Vitamin D deficiency also increases the risk of falls and fractures through its multiple effects on muscle and bone . Malnutrition was described in a study with the Mini-Nutritional Assessment (MNA) tool. In this study, osteosarcopenic individuals present a twofold higher risk for malnutrition (MNA < 12) than individuals in the control group .
Smoking
Smoking may have detrimental effects on the skeletal system. Recent evidence demonstrates tobacco smoking causes an imbalance in the mechanisms of bone turnover, leading to lower bone BMD making bone vulnerable to osteoporosis and fracture . Similarly, components of cigarette smoke enter the bloodstream and reach the skeletal muscles of smokers and accelerate muscle wasting . A metaanalysis of 12 studies (22,515 participants) indicated that cigarette smoking as an isolated factor might contribute to the development of sarcopenia. Therefore, cigarette smoking should be counted among the risk factors of osteosarcopenia .
Alcohol consumption
Alcohol is a significant risk factor for osteoporosis, with an intake of ≥ 3 units of alcohol/day increasing fracture risk in a dose-dependent fashion .
Endocrine
Glucocorticoids
The increased incidence of various diseased states during aging is associated with the hypersecretion of glucocorticoids . Glucocorticoid-associated atrophy appears to be specific to type II or phasic muscle fibers. In a study of controlled hypercortisolemia in healthy men , experimental inactivity increased the catabolic effect of glucocorticoids, suggesting that an absence of mechanical signals potentiates the impact. The mechanism of glucocorticoid-induced atrophy may involve an upregulated expression of myostatin and glutamine synthetase, the latter via the glucocorticoid receptor’s interaction with the glutamine synthetase promoter . Glucocorticoids inhibit the physiological secretion of growth hormone and appear to induce IGF-I activity in target organs . Also, prolonged use of systemic glucocorticoids (i.e., at least three months cumulative use during the preceding year at a prednisone-equivalent dose ≥ 7.5 mg daily) increases the risk of fracture independent of BMD .
Low vitamin D
Vitamin D has been considered a key regulator of bone metabolism and calcium and phosphorus homeostasis through negative feedback with the parathyroid hormone . It is also well established that vitamin D deficiency is a risk factor for osteoporosis in older adults. A large and growing body of evidence suggests that vitamin D is necessary for bone tissue and calcium metabolism . Approximately 1 billion, mostly older persons, worldwide have vitamin D deficiency . The prevalence of low vitamin D concentrations in subjects older than 65 years of age has been estimated at approximately 50% . Similarly, there is an age-dependent reduction in vitamin D receptor expression in skeletal muscle . Prolonged vitamin D deficiency has been associated with severe muscle weakness, which improves with vitamin D supplementation . Interestingly, muscle biopsies performed before and after vitamin D supplementation have documented an increased number and sectional area of type II (or fast) muscle fibers . More comprehensive knowledge of vitamin D-related mechanisms may provide a helpful tool for preventing muscle atrophy in older persons (sarcopenia).
Hypogonadism (male)
In males, levels of testosterone decrease by 1% per year, and those of bioavailable testosterone by 2% per year from age 30 . In women, testosterone levels drop rapidly from 20 to 45 years of age . Testosterone increases muscle protein synthesis , and its effects on muscle are modulated by several factors, including genetic background, nutrition, and exercise . Numerous studies of treatment with testosterone in older persons have been performed over the past few years . In 1999, Snyder et al. suggested that increasing the level of testosterone in older men to that seen in young men increased muscle mass but did not result in functional gains in strength. Systemic reviews of the literature have concluded that testosterone supplementation attenuates several sarcopenic symptoms, including decreases in muscle mass and grip strength . For instance, a recent study of 6 months of supraphysiological dosage of testosterone in a randomized placebo-controlled trial reported increased leg lean body mass and leg and arm strength . Although there are significant increases in strength among older males given high doses of testosterone, the potential risks may outweigh the benefits. Risks associated with testosterone therapy in older men include sleep apnea, thrombotic complications, and the increased risk of prostate cancer .
Menopause (female)
Menopause is a natural part of aging, and it encompasses the loss of ovarian reproductive function. Osteoporosis is a common, asymptomatic postmenopausal disease that substantially impacts the quality of life of older women. Osteoporosis-related fractures are one of the causes of disability among the older population . One in two postmenopausal women will have an osteoporotic fracture in their lifetime .
It has been hypothesized that menopause transition and the subsequent decline in estrogen may play a role in muscle mass loss . Van Geel et al. reported a positive relationship between lean body mass and estrogen levels. Similarly, Iannuzzi-Sucich et al. observed that muscle mass is correlated significantly with plasma estrone and estradiol levels in women. The mechanisms by which a decrease in estrogen levels may have a negative effect on muscle mass are not well understood but may be associated with an increase in proinflammatory cytokines, such as TNF-α and IL-6, which might be implicated in the apparition of sarcopenia . Furthermore, estrogen could directly affect muscle mass since it has been shown that skeletal muscle has estrogen beta-receptors on the cell membrane . Therefore, a direct potential mechanistic link could exist between low estrogen levels and a decrease in protein synthesis.
Low growth hormone
Growth hormone (GH) is a single-chain peptide of 191 amino acids produced and secreted mainly by the somatotrophs of the anterior pituitary gland. GH coordinates the postnatal growth of multiple target tissues, including skeletal muscle . Indeed, circulating GH levels decline progressively after 30 years of age at a rate of ∼ 1% per year . In aged men, daily GH secretion is 5- to 20-fold lower than in young adults . The age-dependent decline in GH secretion is secondary to a decrease in GHRH and an increase in somatostatin secretion . There is evidence that the age-associated decline in GH levels in combination with lower IGF-I levels contributes to the development of sarcopenia . The effects of GH administration on muscle mass, strength, and physical performance are still under debate . In animal models, GH treatment effectively inhibits sarcopenic symptoms such as muscle atrophy and decreases in protein synthesis, particularly in combination with exercise training . The effect of GH treatment on older subjects is controversial. Some groups demonstrated an improvement in strength after long-term administration (3–11 months) of GH . In contrast, many researchers have found that muscle strength or muscle mass did not improve on supplementation with GH .
Hyperparathyroidism
Hyperparathyroidism is due to increased parathyroid gland activity, which leads to osteoporosis with related fractures . Proximal muscle weakness due to type II muscle fiber atrophy can be seen in association with severe bone disease (such as osteoporosis) . High serum levels of parathyroid hormone have been recently associated with osteosarcopenia independently of serum vitamin D or renal function (summarized in Chapter 8 ).
Social
Living in a residential care facility
Dependent older adults pose a particular challenge for researchers because advanced functional and cognitive impairment may limit their capacity to perform tests, especially for speed and strength. As the population ages, a greater number of older adults will need residential support such as residential care facility (RACF). RACF residents are often frail since their multiple physical and cognitive deficits place them at high risk of falls, disability, and death . The fracture rate for adults living in RACF is two to four times that of adults of a similar age living in the community, and one-third of older adults who experience hip fracture are residents in RACF .
A systematic review and metaanalysis published in 2017 by Shafiee et al. addressed the worldwide prevalence of sarcopenia but excluded studies carried out in hospitals or nursing homes for older adults. The prevalence of sarcopenia was shown to be higher in RACF residents. A review followed the consensus of the European Working Group on Sarcopenia in Older People (EWGSOP) , described prevalence values of 1%–29% among older adults living at home, 14%–68% among those in RACF, and 10% among people hospitalized in acute care . Another review included studies that evaluated the prevalence of sarcopenia among older adults (aged ≥ 60 years) living in RACF. Forty-four studies were identified, of which 21 studies were included after applying eligibility criteria. The reported prevalence of sarcopenia ranged widely between 17.7% and 73.3% in RACF and between 22% and 87% in assisted-living facilities . Therefore, it is critical to identify RACF residents with osteosarcopenia.
Comorbidities
A large proportion is of older adults are suffering from chronic comorbidities such as cardiovascular failure, renal failure, or cancer . These comorbidities are associated with a decline of skeletal muscle and bone mass, potentially leading to osteosarcopenia .
Previous fragility fracture
History of fragility fracture is associated with osteoporosis and sarcopenia. In a recent study, 70 out of 139 hip fracture patients (50.36%) were diagnosed with sarcopenia. Hip fracture patients with sarcopenia also have insufficient activity of daily living and a lower quality of life than patients without sarcopenia before the injury and 6 months after the operation . Clinicians should examine people with a history of fragility fracture for sarcopenia and osteoporosis (if not diagnosed already).
Frailty
The odds of frailty are significantly higher in osteosarcopenic patients than those with osteoporosis or sarcopenia alone . Bone and muscle loss also may be tightly linked to the risk of frailty as shown in a 2015 study conducted in China in which osteosarcopenia was found in 26.3% of men and 38.5% of women with frailty and only in 1.6% and 1.9% of nonfrail men and women, respectively .
Sarc-F and BMD
People with one or more osteosarcopenia risk factors need to be screened using the Sarc-F questionnaires, as well as BMD measurement to determine whether a patient is at risk of osteosarcopenia, sarcopenia, or osteoporosis alone.
Sarc-F
To identify candidates for sarcopenia assessment, the Sarc-F questionnaire will be used. Sarc-F comprises five components: strength, assistance with walking, rise from a chair, stair climbing, and falls. The scores range from 0 to 10, with 0 to 2 points for each component. A score equal to or greater than four is predictive of sarcopenia . SARC-F was valid and consistent for identifying people at risk of sarcopenia-associated adverse outcomes. SARC-F has a low-to-moderate sensitivity and a very high specificity to predict low muscle strength . As such, SARC-F primarily detects severe cases. As an inexpensive and convenient method for sarcopenia risk screening, SARC-F is recommended as a way to introduce assessment and treatment of sarcopenia into clinical practice.
BMD
The World Health Organization (WHO) established diagnostic criteria for osteoporosis based on BMD T scores . The T score describes the patient’s BMD in terms of the number of SDs by which it differs from the mean peak value in young, healthy persons of the same sex . The WHO uses a threshold of 2.5 SDs below the mean of young adult women as the criterion for a diagnosis of osteoporosis . The criterion for diagnosing osteopenia (low bone mass) is more than 1.0 SD, but less than 2.5 SDs below the reference mean . However, T scores were developed to estimate the prevalence of osteoporosis across populations, not for the assessment of osteoporosis in specific patients . Moreover, although T scores originally were based on the BMD of the hip measured by dual-energy X-ray absorptiometry (DXA), the scores are now applied to BMD at other skeletal sites and/or measured by different methods . Currently, the National Osteoporosis Foundation and the International Society for Clinical Densitometry consider central DXA of the hip and/or spine as the preferred measurement for a diagnosis of osteoporosis . In this chapter, radiologic diagnostic measures of osteoporosis will be discussed in more detail.
Muscle strength
In patients with osteosarcopenia risk factors who scored 4 or more on Sarc-F, muscle strength needs to be measured. There are several clinical measures of muscle strength.
Grip strength
Grip strength is a simple method to measure muscle strength. Low grip strength is associated with poor patient outcomes such as disability, longer hospital stays, increased functional limitations, poor health-related quality of life, morbidity, and mortality . Measurements of grip strength taken with the Jamar dynamometer have evidence for good to excellent ( r > 0.80) test-retest reliability and excellent ( r = 0.98) interrater reliability . High test-retest reliability has been shown among older American community-dwelling volunteers (mean age 75 years) repeatedly tested over 12 weeks . Grip strength correlates moderately with strength in other body compartments, so it serves as a reliable surrogate for more complicated measures of arm and leg strength . Because of its ease of use, grip strength is advised for routine use in hospital practice, specialty clinical settings, and community healthcare .
Accurate measurement of grip strength requires using a calibrated handheld dynamometer under well-defined test conditions with measurement protocol to improve the validity of assessment . It was demonstrated that the choice of equipment and measurement protocol for assessing grip strength varies widely between studies. The Jamar hand dynamometer is the most widely cited instrument in the literature and appears to be a generally accepted gold standard with the most normative data .
Measurement protocol
The American Society of Hand Therapists (ASHT) recommends standardized positioning: patient seated, shoulders adducted and neutrally rotated, elbow flexed at 90°, forearm in neutral, and wrist between 0° and 30° of dorsiflexion . Different methods of instruction and/or verbal encouragement can affect the patients’ performance and thus introduce measurement error . Mathiowetz et al. have a set of standardized instructions: “I want you to hold the handle like this and squeeze as hard as you can.” The examiner demonstrates and then gives the dynamometer to the subject. After the subject is positioned appropriately, the examiner says, “Are you ready? Squeeze as hard as you can.” As the subject begins to squeeze, the examiner says, “Harder!… Harder!… Relax” .
Sarcopenia cut-off points for grip strength vary according to the sarcopenia definition used. Table 1 summarizes the cut-off points for EWGSOP2, Asian Working Group for Sarcopenia, and The Foundation for the National Institutes of Health (FNIH) .
| Sarcopenia definition | Measurement modality (cut-off points) |
|---|---|
| EWGSOP2 | (Men < 27 kg; women < 16 kg) |
| SDOC | Handgrip strength (men < 35.5 kg; women < 20 kg) |
| Handgrip strength:BMI (men ≪ 1.05 kg/kg/m 2 ; women < 0.79 kg/kg/m 2 ) | |
| Asian Working Group for Sarcopenia | Handgrip strength (men < 26 kg; women < 18 kg) |
Chair stand
The chair stand test can be used as a proxy for the strength of leg muscles (quadriceps muscle group). The chair stand test measures the amount of time needed for a patient to rise five times from a seated position without using their arms; the timed chair stand test is a variation that counts how many times a patient can rise and sit in the chair over a 30-s interval . Since the chair stand test requires both strength and endurance, this test is a qualified but convenient measure of strength.
In the chair stand test, participants are asked to stand up five times in a row as quickly as possible from a chair without stopping, keeping arms folded across the chest. Participants have to come to a full standing position each time they stood up and to sit all the way down each time. Timing starts when the examiner says “Go!” and stops when the participant sits down for the fifth time. Time (in seconds) or inability to perform the test is used as a result of the test . According to EWGSOP2, older adults who complete 5 rises in more than 15 s are considered sarcopenic .
Lower limb strength
When measurement of grip is not possible due to hand disability (e.g., with advanced arthritis or stroke), isometric torque methods can be used to measure lower limb strength (most frequently of the quadriceps) . Commercial dynamometers can enable isometric and/or isokinetic measurements of strength . Even if these measurements are feasible in frail people , they are often limited in clinical practice by their relative expense, the need to purchase dedicated equipment, the lack of trained staff, and limited data in older populations. Harbo et al. described a lower limb strength measurement protocol for research purposes .
Muscle mass
If a participant has low muscle strength, muscle mass needs to be measured to confirm the diagnosis of sarcopenia. Muscle mass can be estimated using different techniques, and there are multiple methods of adjusting the result for height or BMI . Muscle (lean)mass can be reported as total body Skeletal Muscle Mass (SMM), as Appendicular Skeletal Muscle Mass (ASM), or as cross-sectional muscle area of specific muscle groups or body locations. The diagnostic measures of muscle mass include DXA (the most commonly used diagnostic measure ), Computed Tomography (CT)/Magnetic Resonance Imaging (MRI) (considered the gold standard), ultrasound, or bioimpedance analysis (BIA). In this chapter, the radiological and nonradiological diagnostic measures of muscle mass will be discussed in detail.
Physical performance
Physical performance is a multidimensional concept that involves not only muscles but also central and peripheral nervous functions, including balance . Measuring physical performance aims to determine the severity of osteosarcopenia. Physical performance can be measured by gait speed, Short Physical Performance Battery (SPPB), Timed-Up and Go test (TUG), or 400-m walk test, among other tests.
Gait speed
The most widely used tool in clinical practice for assessing physical performance is the gait speed measurement. The test is highly acceptable for participants and health professionals in clinical settings . No special equipment is required as it only needs a flat floor devoid of obstacles with a straight, clearly marked course. A trained operator with a stopwatch is also needed as an evaluator . Patients are instructed to walk at their usual pace from a still-standing position behind the starting line. Timing starts at the first foot movement and ends when a foot completely crossed the finish line. Canes and walkers are allowed if a patient normally used this equipment in their daily life. In the 4-m gait speed test, which the EWGSOP2 recommends for assessing sarcopenia, men and women with a gait speed < 0.8 m/s are described as having poor physical performance .
400-m walk test
The 400-m walk test assesses walking ability and endurance. For this test, patients are asked to complete 20 laps of 20 m, each lap as fast as possible, and are allowed up to two rest stops during the test. Measurement protocol and equipment are similar to the gait speed test .
Short physical performance battery
The Short Performance Physical Battery (SPPB) is an objective physical performance measure focused on lower extremity physical function and measures balance, strength, and coordination , which are important contributors to mobility and independence . In older adults with a high degree of frailty and impairment, age- and gender-adjusted SPPB is associated with increased emergency room visits and hospitalizations . The SPPB is a composite test that includes an assessment of gait speed, a balance test, and a chair stand test, and each component is scored between 0 and 4 . This performance-based tool is a continuous measure with total scores ranging from 0 to 12. From previous validation , scores of 0–4, 5–8, and 9–12 indicate poor, intermediate, and good lower extremity function, respectively. For the assessment of sarcopenia, a score of ≤ 8 points indicates poor physical performance .
Timed-up and go test
The Timed-Up and Go test (TU & Go) is the most used test worldwide . This test measures the dynamic balance and functional mobility in older adults, as well as in the neurological population . The TU & Go is a simple test that can be performed anywhere and consists of a patient getting up from a chair from the sitting to the bipedal position, walking three meters, turning, returning, and sitting on the chair again. The variable measured is the total time taken by the test, and then the score assigned in seconds is observed, which is correlated with the risk of falls . Some of the advantages of the TU & Go test are the simplicity in its application and its short duration. In addition, it requires little equipment and allows the possibility that people with a functional impairment can perform the test . The EWGSOP2 suggested that patients with a TU & Go of 20 s or more are described as having poor physical performance .
Table 2 summarizes the sarcopenia cut points of sarcopenia cut-off points of physical performance measures for EWGSOP2, Asian Working Group for Sarcopenia, and the FNIH .