Multiple myeloma (MM) is a tumor of monoclonal plasma cells, which produce a monoclonal antibody and expand predominantly in the bone marrow. Patients present with hypercalcemia, renal impairment, anemia, and/or bone disease. Only patients with symptomatic MM require therapy, whereas asymptomatic patients receive regular follow-up. Survival of patients with MM is very heterogeneous. The variety in outcome is explained by host factors as well as tumor-related characteristics reflecting biology of the MM clone and tumor burden. The identification of cytogenetic abnormalities by fluorescence in situ hybridization is currently the most important and widely available prognostic factor in MM.
Key points
- •
Multiple myeloma (MM) is a tumor of monoclonal plasma cells, which produce a monoclonal antibody and expand predominantly in the bone marrow.
- •
Patients present with hypercalcemia, renal impairment, anemia, and/or bone disease (CRAB criteria). Only patients with symptomatic MM require therapy, whereas asymptomatic patients receive regular follow-up. Survival of patients with MM is very heterogeneous.
- •
Gene expression profiling is emerging as a prognostic tool to further improve risk stratification.
- •
Incorporation of imaging techniques, such as positron emission tomography/computed tomography and magnetic resonance imaging, will add valuable information to the standard response assessment.
- •
New therapeutic strategies for high- and low-risk MM should be explored in the setting of clinical trials.
Clinical presentation
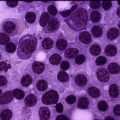
Multiple myeloma (MM) is a tumor of terminally differentiated monoclonal B cells (plasma cells) that produce a monoclonal protein and .expand predominantly in the bone marrow (BM). Hypercalcemia, renal impairment, anemia, and bone disease represent the CRAB criteria for symptomatic MM requiring therapy.
Symptoms of anemia develop as a result of displacement of normal hematopoiesis. Thrombocytopenia occurs rarely with only 5% of patients with newly diagnosed MM presenting with platelets less than 100 × 10 9 /L. Alterations in the BM microenvironment result in reduced bone formation by osteoblasts and increased bone destruction by osteoclasts, which lead to diffuse osteoporosis, osteolytic lesions, and painful pathologic fractures. There is also a higher incidence of infections because of immune dysfunction, especially during active disease. Approximately 20% of the patients with newly diagnosed MM present with renal impairment (creatinine ≥2 mg/dL); it is most frequently caused by light-chain cast nephropathy, which results in extensive destruction of tubular cells. Several other factors, such as dehydration, hypercalcemia, infections, nephrotoxic drugs, and contrast media, may also contribute to renal impairment. Also amyloidosis and monoclonal immunoglobulin deposition disease are causes of renal impairment in MM, leading to usually nonselective proteinuria.
Clinical presentation
Multiple myeloma (MM) is a tumor of terminally differentiated monoclonal B cells (plasma cells) that produce a monoclonal protein and .expand predominantly in the bone marrow (BM). Hypercalcemia, renal impairment, anemia, and bone disease represent the CRAB criteria for symptomatic MM requiring therapy.
Symptoms of anemia develop as a result of displacement of normal hematopoiesis. Thrombocytopenia occurs rarely with only 5% of patients with newly diagnosed MM presenting with platelets less than 100 × 10 9 /L. Alterations in the BM microenvironment result in reduced bone formation by osteoblasts and increased bone destruction by osteoclasts, which lead to diffuse osteoporosis, osteolytic lesions, and painful pathologic fractures. There is also a higher incidence of infections because of immune dysfunction, especially during active disease. Approximately 20% of the patients with newly diagnosed MM present with renal impairment (creatinine ≥2 mg/dL); it is most frequently caused by light-chain cast nephropathy, which results in extensive destruction of tubular cells. Several other factors, such as dehydration, hypercalcemia, infections, nephrotoxic drugs, and contrast media, may also contribute to renal impairment. Also amyloidosis and monoclonal immunoglobulin deposition disease are causes of renal impairment in MM, leading to usually nonselective proteinuria.
Differential diagnosis
Sixty-three percent of the patients with MM present at more than 65 years of age, and 37% of the patients newly diagnosed with MM are older than 75 years. Therefore, patients may present with renal impairment that is not related to MM but a result of other underlying medical conditions that are prevalent in elderly patients, such as hypertension and diabetes. Similarly, primary hyperparathyroidism should be considered for hypercalcemia; deficiencies of iron, vitamin B 12 , and folic acid for anemia; and metastatic carcinoma for lytic bone lesions. Other symptomatic plasma cell diseases that have to be excluded include solitary plasmacytoma and primary plasma cell leukemia (pPCL) ( Table 1 ). Symptomatic MM is virtually always preceded by monoclonal gammopathy of uncertain significance (MGUS) that progresses to smoldering myeloma (SMM) (see Table 1 ). MGUS and SMM do not require therapy but only clinical observation, except in the setting of clinical trials.
| International Myeloma Working Group Consensus Diagnostic Criteria Combined with the Mayo Clinic Criteria | |
|---|---|
| Non-IgM MGUS | |
| IgM MGUS | |
| Light-chain MGUS | |
| SMM (or asymptomatic MM) | |
| Idiopathic Bence Jones proteinuria | |
| Symptomatic MM | |
| Solitary plasmacytoma | |
| pPCL |
|
a End-organ damage includes hypercalcemia (serum calcium >11.5 mg/dL [>2.65 mM]), renal insufficiency (serum creatinine >2 mg/dL [>177 μM]), anemia (hemoglobin <10 g/dL [<6.2 mM] or >2.0 g/dL [>1.25 mM] less than the lower limit of the normal range), and bone disease (lytic bone lesions, severe osteopenia, or pathologic fractures) (CRAB) that can be attributed to the plasma cell proliferative disorder.
b Especially in elderly persons other causes should be considered, such as deficiencies of vitamin B 12 , folic acid, or iron for anemia; primary hyperparathyroidism for hypercalcemia; diabetes and hypertension for renal insufficiency; and metastatic carcinoma for lytic bone lesions.
c End-organ damage includes anemia, constitutional symptoms, hyperviscosity, lymphadenopathy, or hepatosplenomegaly that can be attributed to the underlying lymphoproliferative disorder.
Diagnostic workup of MM
At the time of MM diagnosis, the authors obtain a detailed medical history and physical examination and perform laboratory studies, such as full blood count and differential, peripheral blood smear, blood chemistry including tumor lysis parameters, beta-2 microglobulin, serum protein electrophoresis, and free light chains ( Box 1 ). Staging procedures should also include the evaluation of urine M protein in 24-hour urine and a skeletal survey. Whole-body radiographs still remain the standard tool for the evaluation of MM bone disease. However, it is well recognized that this imaging technique underevaluates the extent of skeletal lesions. Low-dose whole-body computed tomography (CT), which is faster and has greater sensitivity compared with standard radiography, is a valuable alternative. Magnetic resonance imaging (MRI) is useful for the evaluation of cord compression or a painful area of the skeleton. Furthermore, MRI is recommended in patients with radiographs suggesting a solitary plasmacytoma of the bone.
Medical history and physical examination
With emphasis on the presence of comorbidities, frailty, and disability (Charlson index, ADL, and IADL)
Blood
Complete blood count with differential
BUN, creatinine, liver enzymes, bilirubin, alkaline phosphatase, total protein, CRP
LDH, calcium, phosphate
Beta-2 microglobulin and albumin
Serum protein electrophoresis, immunofixation, serum-free light-chain analysis
Urine
24-hour urine collection for electrophoresis and immunofixation
24-hour urine for total protein
Bone marrow
Biopsy for histology
Aspirate for
Morphology
Immunophenotyping
Cytogenetic analysis by FISH a at least focused on del(17p13), t(4;14), ampl(1q21), and t(14;16); an extended panel may focus on del(13q), del(1p21), t(11;14), t(14;20), and ploidy status
Radiographic skeletal survey including skull, pelvis, vertebral column, and long bones b
Additional investigations, which may be useful under certain circumstances
Lumbar puncture (cell counts, chemistry, cytology, immunophenotyping): suspicion of leptomeningeal involvement
MRI: evaluation of cord compression or painful area of the skeleton (suspicion of soft tissue plasmacytomas arising from bone) as well as in the evaluation of patients with radiographs suggesting a solitary plasmacytoma of the bone
CT or 18 F-FDG-PET/CT: suspicion of extramedullary plasmacytomas
Survey for evaluation of AL amyloidosis
Bleeding time, APTT, PT
Cryoglobulins, cold agglutinins
Serum viscosity, fundoscopy: symptoms of hyperviscosity
HLA typing: in case allo-SCT is considered
Abbreviations: ADL, activities of daily living; allo-SCT, allogeneic stem cell transplantation; APTT, activated partial thromboplastin time; BUN, blood urea nitrogen; CRP, C-reactive protein; CT, computed tomography; 18 F-FDG-PET, 18 F-fluorodeoxyglucose positron emission tomography; FISH, fluorescence in situ hybridization; IADL, instrumental activities of daily living; LDH, lactate dehydrogenase; MRI, magnetic resonance imaging; PT, prothrombin time.
a FISH is preferably performed on purified tumor cells or with simultaneous staining of cytoplasmic immunoglobulins.
b As alternative to conventional radiography, low-dose whole-body CT can be considered.
In addition, the authors perform a BM biopsy and BM aspiration for morphology, immunophenotyping by flow cytometry, and cytogenetic analysis by fluorescence in situ hybridization (FISH), which should include at least t(4;14)(p16;q32), t(14;16)(q32;q23), ampl(1q21), and del(17p13) (see Box 1 ). Lumbar puncture, MRI, or CT is performed when extramedullary (EM) involvement is suspected.
Prognostic factors
Response to treatment and survival of patients with MM is very heterogeneous, with some patients dying of refractory MM within a few weeks, whereas others live for more than 10 years. This variety in outcome is related to intrinsic tumor cell characteristics, including sensitivity to active MM drugs, tumor burden, and several host factors. Risk stratification of patients with MM is important in order to define which patients will have a long-term survival and which patients have high-risk MM, so that the best therapeutic strategy can be defined.
In the next section, the authors describe prognostic factors that reflect myeloma biology and represent MM tumor burden and discuss patient characteristics that have an impact on survival. Because outcome is also associated with quality of response, the authors also discuss several therapy-related factors.
Disease characteristics
Conventional Cytogenetics
Conventional cytogenetics reveal karyotypic abnormalities in only 20% to 30% of the patients, whereas more sensitive techniques that are not based on metaphase availability, such as FISH, array comparative genomic hybridization, and single-nucleotide polymorphism (SNP)–based mapping arrays, reveal that virtually all MM tumors have chromosomal abnormalities. This discrepancy is related to the low proliferation index of the tumor cells observed in most patients with MM. The normal karyotype in patients with a low proliferation index probably corresponds with normal BM myeloid cells.
FISH
FISH can detect specific changes in interphase cells, thereby overcoming the problem of the lack of proliferating cells, which are required for conventional cytogenetic analysis. Because of the frequent low percentage of tumor cells in the BM aspirate, plasma cell purification or sorting is required before FISH.
In MM chromosome translocations involving the immunoglobulin heavy chain (IgH) locus and hyperdiploidy, with multiple trisomies of chromosomes 3, 5, 7, 9, 11, 15, 19, and 21, are primary events, whereas other events, such as del(17p) and amp(1q21), are acquired during disease progression ( Table 2 ).
| Genomic Aberration | Incidence (%) |
|---|---|
| del(13q) | ∼50 |
| 14q32 Translocations | ∼50–60 |
| Hyperdiploidy | ∼50 |
| t(4;14) | ∼15 |
| t(11;14) | ∼15 |
| t(14;16) | ∼5 |
| t(14;20) | ∼1 |
| del(17p) | ∼10 |
| amp(1q21) | ∼30–43 |
| del(1p21) | ∼20 |
Hyperdiploidy occurs in approximately 50% of patients with newly diagnosed MM and is associated with an improved progression-free survival (PFS) and overall survival (OS). However, patients with hyperdiploidy represent a heterogeneous group, which is partly explained by the presence of other cytogenetic abnormalities (see later discussion).
Translocation t(4;14) leads to deregulation of fibroblast growth factor receptor 3 ( FGFR3) and multiple myeloma SET domain ( MMSET) . However, because FGFR3 is not expressed in about one-third of the patients with t(4;14), the target gene is most likely MMSET . The t(4;14) is associated with impaired PFS and OS in several studies. Importantly, bortezomib seems to overcome part of the negative prognostic impact of t(4;14).
The translocation t(14;16) results in deregulation of the c-MAF proto-oncogene and is predictive of a poor outcome. However, an intergroupe francophone du myelome (IFM) analysis showed no adverse impact of t(14;16), which may be related to treatment differences, with 60% of patients in this study receiving double auto-stem cell transplantation (SCT). The rare translocation t(14;20) results in deregulation of MAFB and confers a poor prognosis.
The translocation t(11;14) results in upregulation of cyclinD1 and was identified as a favorable prognostic factor in some studies, whereas it has no impact on outcome in others. This translocation is also associated with CD20 expression on the cell surface and lymphoplasmacytic morphology of the tumor cells.
Del(13q) predicts for impaired PFS and OS; however, the negative prognostic impact of del(13) is mainly related to its frequent association with del(17p) and t(4;14). In patients with del(13q) detected by FISH without t(4;14) or del(17p), del(13q) is no longer predictive of survival. However, deletion of chromosome 13 retains its prognostic value when it is detected by conventional cytogenetics.
Del(17p) is an important prognostic factor with a negative impact on PFS and OS. The molecular target of del(17) may be TP53 , which is important in both clonal immortalization and survival of tumor cells after treatment. Several studies show that bortezomib or lenalidomide do not overcome the poor prognosis conferred by del(17p). However, in the randomized Hovon-65/GMMG-HD4 study, long-term bortezomib administration during induction and maintenance overcomes part of the adverse impact of del(17p). Also incorporation of bortezomib in the Total Therapy 3 (TT3) protocol abrogated the negative prognostic impact of del(17p) in patients with gene-expression profiling (GEP)–defined low-risk disease. These conflicting results may be explained by differences in the cumulative dose of bortezomib administered in the different protocols.
Gain of 1q21 has also been linked to an adverse prognsosis. Patients with greater than 3 copies of 1q21 have a worse outcome when compared with patients with 3 copies of 1q21, possibly reflecting a dosage effect of genes located at this chromosomal region. Also del(1p) confers poor prognosis in MM.
Multiple Adverse Cytogenetic Abnormalities
Boyd and colleagues showed that ampl(1q) is very common in patients with adverse IgH translocations. Seventy-two percent of the patients with an adverse IgH translocation also had amp(1q21), whereas this was 32.4% in the group without adverse IgH translocations. The frequency of del(17p) was similar in patients with or without adverse IgH translocations. Importantly, there is an association between the accumulation of adverse lesions and progressive impairment of survival. The median PFS and OS of patients treated in the Medical Research Council (MRC) Myeloma IX trial without adverse genetic lesions (no adverse IgH translocation, no del[17p], and no amp[1q21]), one adverse lesion, and greater than 1 adverse genetic lesion was 23.5, 17.8, and 11.7 months and 60.6, 41.9, 21.7 months, respectively. The median OS was only 9.1 months for the 16 patients with 3 adverse genetic abnormalities.
Good Combined with Adverse Cytogenetic Abnormalities
Within the group of patients with hyperdiploidy, there is a great heterogeneity in survival. Avet-Loiseau and colleagues showed that gain of 5q31 resulted in a better outcome in hyperdiploid MM compared with hyperdiploid cases without this feature. Another study demonstrated that among patients with hyperdiploidy trisomy 11 confers a favorable prognosis, whereas gain of 1q and loss of chromosome 13 drive poor outcomes. Also GEP identifies subclasses of hyperdiploid MM with different clinical outcomes.
Another study showed that coexistent hyperdiploidy does not abrogate the poor prognosis associated with adverse cytogenetics in MM. In the Myeloma IX study, 58% of the patients had hyperdiploidy. Of these hyperdiploid patients, 61% had one or more adverse lesions (t[14;14], t[14;16], t[14;20], amp[1q], or del[17p]). The OS and PFS were significantly worse in patients with hyperdiploidy with an adverse lesion when compared with those patients with hyperdiploidy alone (median PFS 23.0 vs 15.4 months; median OS 60.9 vs 35.7 months). Alternatively, the outcome of patients with an adverse lesion was independent of the presence or absence of hyperdiploidy.
However, a recent study showed that patients with high-risk chromosomal abnormalities (t[4;14], t[14;16], t[14;20], or del[17p]) have different outcomes depending on the presence (median OS: not reached) or absence of trisomy (median OS: 3 years).
Gene Expression Profiling
Several studies have evaluated myeloma at the transcriptional level by using GEP, which has led to molecular classification systems for MM based on differential gene expression but also to improved risk stratification. So far none of these signatures has been introduced into general clinical practice.
Shaughnessy and colleagues evaluated the gene expression profile of newly diagnosed MM patients and identified a 70-gene subset as an independent predictor of outcome. The presence of a high-risk signature (13.1% of the patients) resulted in inferior event-free survival (EFS) (5-year EFS: 18% vs 60%) and OS (5-year OS: 28% vs 78%) compared with a low-risk signature. In this 70-gene high-risk signature, elevated expression levels of genes mapped to chromosome 1q and reduced expression levels of genes mapped to chromosome 1p, which reflects the importance of amp(1q21) and del(1p) in conferring a poor prognosis. However, epigenetic modifications in chromosome 1 cannot be excluded. The same group performed GEP analysis before and 48 hours after a bortezomib test dose in patients treated in bortezomib-based TT3 protocols. Based on changes in expression following the test dose, the University of Arkansas Medical School (UAMS)-80 signature was constructed, which has strong prognostic impact on both PFS and OS. The selected genes in this model were enriched in genes of the protein ubiquitination pathway.
The Erasmus MC-92 signature is derived from patients treated in the Hovon-65/GMMG-HD4 trial, and predicts for impaired PFS and OS in several independent data sets. The survival of high-risk patients in the bortezomib arm of the Hovon-65/GMMG-HD4 study was 30 months, whereas it was 19 months in the vincristine, adriamycin, dexamethasone (VAD) arm. Other GEP-based risk models that predict survival in patients newly diagnosed with MM include the IFM-15 and MRC-IX-6 gene expression signatures. These different models have to be validated in the context of other treatment approaches because it is to be expected that prognostic factors change with different treatment schedules.
Plasma Cell Proliferation
Several studies using different techniques have demonstrated that proliferation of tumor cells is an important independent adverse prognostic factor in MM. The plasma cell labeling index (PCLI) is a measure of the fraction of cells in S phase and is evaluated by using fluorescence microscopy. The PCLI predicts for impaired PFS and OS. Furthermore, reduction of the PCLI after initial therapy is predictive of improved survival.
Use of the PCLI has not gained widespread acceptance because of its labor-intensive slide-based method. However, the fraction of plasma cells in S phase can also be determined by flow cytometry. With this technique, a subgroup of patients with inferior PFS and OS can be identified. A recent study showed that novel agents may overcome the poor prognosis of patients with a high plasma cell proliferation index as determined by flow cytometry.
In another technique, Ki-67 staining identifies proliferating cells in G1, G2, S, and M phases of the cell cycle (but not G0). In MM, it is associated with impaired survival. Also gene-expression–based proliferation assessment identifies patients with significantly inferior EFS and OS.
Lactate Dehydrogenase
Elevated lactate dehydrogenase (LDH) levels are present in 10% to 15% of newly diagnosed patients. Several studies have shown that high LDH serum levels are associated with advanced disease and shorter survival. LDH retains its prognostic significance in patients treated with novel agents (JCO Moreau, unpublished, 2014).
M Protein Isotype
The isotype of the M protein that is produced by the plasma cell clone may have prognostic value. However, this is frequently related to presence of other poor prognostic factors. For example, patients with IgA MM have an inferior outcome when compared with IgG MM, which is related to its association with t(4;14).
IgD MM accounts for approximately 1% to 2% of all MM cases and is associated with a high frequency of undetectable or small M-protein levels. IgD MM is characterized by an increased frequency of EM involvement, anemia, renal failure, osteolytic bone lesions, hypercalcemia, and International Staging System (ISS) stage III disease. The clustering of these adverse prognostic factors may explain the poor prognosis of IgD MM when compared with IgG or IgA MM.
Similar to IgD MM, IgE M-protein levels are very low in IgE MM. IgE MM is a very rare subgroup and has a poor prognosis.
EM Myeloma and Primary Plasma Cell Leukemia
EM disease is more common in patients with high-risk cytogenetics or high-risk GEP profiles and carries a poor outcome. EM disease occurs more frequently at the time of relapse than at diagnosis.
EM disease (positron emission tomography [PET]–positive lesions not contiguous to bone and arising in soft tissues) was detected by using PET/CT in 6% of patients with newly diagnosed MM who were treated with double auto-SCT. In this study, EM disease was predictive of shorter PFS (4-year PFS: 22% vs 63% for patients with and without EM disease, respectively) and OS (4-year OS: 64% vs 90%). EM disease defined by PET/CT (present in 6% of cases) also had a prognostic impact in patients enrolled in TT3.
The most aggressive plasma cell dyscrasia is pPCL. Compared with MM, pPCL presents more often with anemia, thrombocytopenia, hypercalcemia, EM involvement, impaired renal function, elevated beta-2 microglobulin, high plasma cell labeling index, increased LDH levels, and GEP-defined high-risk disease. Furthermore, the presence of high-risk cytogenetic abnormalities, such as t(4;14), t(14;16), del(17p), del(1p), and amp(1q), is markedly higher in pPCL compared with newly diagnosed MM. Conversely, the incidence of hyperdiploidy is rare (0%–8.8%). Altogether, this explains the poor prognosis of patients with pPCL.
Imaging Characteristics
Both MRI and PET/CT findings at the time of diagnosis have prognostic value. The number of focal lesions as detected by MRI is a prognostic marker for PFS and OS. In addition, diffuse BM involvement is associated with more advanced disease and inferior survival.
An Italian study, with patients enrolled in a trial that included double auto-SCT, showed that several characteristics of PET/CT have prognostic value, including the presence of EM disease, degree of fluorodeoxyglucose (FDG) uptake at the time of diagnosis, and type of BM involvement (>3 focal lesions or diffuse BM uptake). The number of focal lesions and degree of uptake before therapy as defined by PET/CT was also predictive of outcome for patients treated in TT3.
Higher numbers of focal lesions on MRI and PET, as well as the degree of uptake on PET, are linked to GEP-defined high-risk disease.
Other Factors
Several studies have shown that several variables that reflect tumor burden, including M-protein level, extent of bone lesions, BM plasma cell infiltration, beta-2 microglobulin, low platelet count, and anemia, have prognostic value in patients with newly diagnosed MM. Other factors that are associated with reduced survival include albumin, serum calcium, and presence of plasmablastic morphology.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree