Fig. 5.1
Tamoxifen-induced cystic hyperplasia of the endometrium
Hence, in asymptomatic women, there is a poor correlation between ultrasonographically measured endometrial thickness and abnormal pathology, and screening them has not shown to be beneficial. Thus, evaluation of the endometrium should be performed only in postmenopausal women with abnormal uterine bleeding. However, the risk of developing endometrial carcinoma is estimated to be only 1.26 for 1000 patient-years after 5 years of tamoxifen intake. Further, based on the findings of the ATLAS study [7], ACOG recommends that tamoxifen use may be extended to 10 years rather than 5 years [8]. ACOG does not recommend screening in premenopausal women and asymptomatic postmenopausal women taking tamoxifen [8].
Family history of malignancies among other members should not be overlooked, especially endometrial, breast, and colon cancers. Lynch syndrome or HNPCC (hereditary nonpolyposis colon cancer) is known to be associated with 40–60 % increased risk of endometrial malignancy, and 5 % of all endometrial cancers may be attributed to it. Germline mutation in one of four genes in the DNA mismatch repair family MLH1, MSH2, MSH6, or PMS2 is known to be associated with Lynch syndrome. Endometrial cancer occurs at an earlier age in these women, 47 years when compared to 60 years in general population [9]. Although BRCA1 and BRCA2 are known to be significantly associated with breast and ovarian cancers, lifetime risk of endometrial carcinoma is not increased in these women [10].
General examination should focus on detecting anemia, icterus, edema, and supraclavicular and inguinal lymph node enlargement. Clinical examination should aim at ruling out obvious causes of postmenopausal bleeding like those caused by lesions of the vulva, vagina, and cervix. This can be effectively done by visual inspection of the external genitalia in good light followed by a speculum examination. This should be followed by a bimanual examination to look for uterine size, tenderness, and irregularity, to rule out benign lesions, more so in premenopausal women. A rectovaginal examination aids in assessing the pouch of Douglas, the parametrium, and the adnexal pathology.
Pap Smear
If clinical examination does not reveal any obvious cause of postmenopausal bleeding, a Pap smear should be taken before doing the bimanual examination. Atypical glandular cells (AGC) reported on Pap smear are known to be associated with endocervical, endometrial, ovarian, or fallopian tube cancers 3–17 % of the time. These women should undergo a fractional curettage and pelvic imaging to rule out these cancers [11].
Office Endometrial Biopsy
The first step in the evaluation of the endometrium is invariably an office endometrial biopsy. Different devices which are available for performing the same are Novak curette, Pipelle endometrial suction curette, and Vabra aspirator (Fig. 5.2). Multiple studies have been done to determine the better device among these three, but it has been found that the accuracy for diagnosis of endometrial cancer is almost similar among these three (Novak curette, 67–97 %; Pipelle endometrial suction curette, 79–94 %; Vabra aspirator, 80–98 %) [12].
Fig. 5.2
Endometrial biopsy curettes
The success of the procedure is affected by many factors like cervical stenosis, alteration of the endometrial cavity by the submucous fibroids, and the size of the lesion itself. The yield of office endometrial biopsy can be increased by combining it with office hysteroscopy especially in small lesions [12]. False-negative rate of office endometrial biopsy is around 10 %, so further evaluation is recommended if the results come back as normal with persistent symptoms or abnormal pelvic imaging [13].
Transvaginal Ultrasound
Transvaginal ultrasound (TVUS) examination is a useful adjunct to office endometrial biopsy in the initial evaluation of endometrial pathology. The endometrium is usually evaluated by examining the thickness and morphology. Endometrial thickness of more than 5 mm is abnormal in postmenopausal women [14] (Fig. 5.3).


Fig. 5.3
Thickened endometrium by ultrasonogram
A normal TVUS decreases the pretest probability of endometrial cancer from 10 to 1 % posttest among postmenopausal women with vaginal bleeding [15]. Endometrial thickness is dynamic in premenopausal women; nevertheless, transvaginal ultrasound examination can be helpful in diagnosing benign conditions like fibroids and adenomyosis which can also present with abnormal uterine bleeding. At this juncture, it is prudent to mention that 17 % of type II endometrial cancers will have a thin endometrium as these cancers develop in a background of atrophy [16]. TVUS has good negative predictive value (99 %) but a poor positive predictive value (57 %) in the diagnosis of endometrial cancer which further decreases to 37 % in women taking hormone replacement therapy [15].
Endometrial thickness can be morphologically classified as diffuse or focal. Diffuse endometrial thickness may be due to endometrial hyperplasia or carcinoma, and a non-focal blind biopsy is sufficient for diagnosis, whereas focal endometrial biopsy can be due to lesions like polyps, either benign or malignant, and requires hysteroscopic-guided biopsy. Other morphological features described by researchers to indicate malignancy are heterogeneous and hyperechoic with irregular borders. It is recommended that combined assessment of endometrial thickness and morphology should be done to improve detection of endometrial pathology [17].
Color Doppler
Color Doppler used along with TVUS aids in the diagnosis of endometrial malignancy. The pattern of vascularity in the thickened endometrium or a focal lesion helps in distinguishing between malignant and benign conditions. Broad-based lesions with diffuse high level of vascularity indicate malignant lesions, and single feeding vessel in the stalk of a focal lesion with low vascularity indicates a benign condition like polyps [18]. When Doppler analysis was compared to conventional gray-scale TVUS, researchers found that abnormal endometrial thickness alone is a better predictor of endometrial pathology than Doppler analysis [19].
Sonohysterography
Transvaginal ultrasound examination is performed after installing sterile normal saline into the endometrial cavity to enable better visualization of lesions like endometrial polyps, submucous fibroids, adhesions, and others. This is especially recommended in women who are on tamoxifen as they tend to have endometrial polyps [14]. Sonohysterography accurately identifies endometrial pathology with reported sensitivities of 89–98 % and specificities of 46–88 % with a good negative predictive value for detecting malignancy. But the positive predictive value for cancer prediction is very poor (16 %) which implies that it is very good at detecting benign conditions [20].
Hysteroscopy and Guided Biopsy
Hysteroscopy enables visualization and guided biopsy especially in small early lesions which can be easily missed on routine office endometrial biopsy (Fig. 5.4).
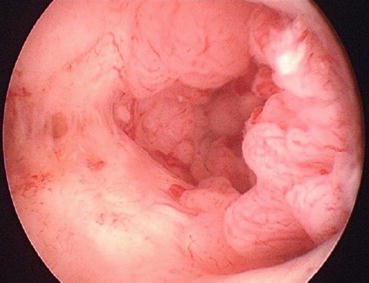
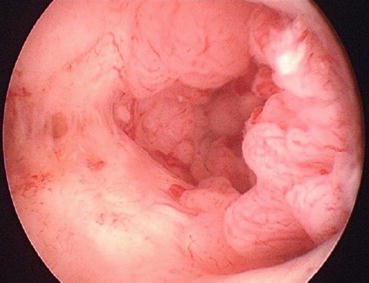
Fig. 5.4
Hysteroscopic image of endometrial malignancy
It is also useful in evaluating falsely thickened endometrium of women on tamoxifen which is due to subendometrial edema [14]. Hysteroscopy has good sensitivity and specificity at 86 % and 99 %, respectively. Like other modalities described above, the negative predictive value of hysteroscopy for detecting malignancy is up to 99 % with positive predictive value of 72 % [21].
Dilatation and Curettage
Dilatation and curettage was the recommended diagnostic test for evaluation of abnormal bleeding before office endometrial biopsy took over. Currently the indications for dilatation and curettage are inability to perform office endometrial biopsy due to patient distress, cervical stenosis, and anatomical factors like submucous fibroids. It is a day care procedure done under anesthesia, either local (paracervical block) or general. Hysteroscopic visualization during the procedures enables sampling of smaller lesions.
CECT, MRI, and PET-CT of the Abdomen and Pelvis
None of these imaging tests are indicated in screening or diagnosis of endometrial cancer. They are useful in pre-management workup of the patients as discussed in the next section.
Pre-management Workup
In a patient who is diagnosed with endometrial cancer, pre-management workup is essentially directed toward assessing the clinical stage of disease to decide the mode of initial treatment. In patients for surgery, pre-op workup also aims at determining medical fitness for surgery and deciding the extent of surgery. NCCN (2016) and ESMO 2015 [22] recommend following investigations in the initial evaluation of endometrial cancer (Table 5.1).
Recommended | Optional |
|---|---|
Clinical and gynecological examination | Genetic counseling in women <50 years and in those with family history of endometrial cancer and colon cancer |
Histopathology of endometrial biopsy | Cervix biopsy or MRI in suspected cases of cervical involvement |
CBC including platelets | CA-125 (optional), MRI, CECT in suspected extrauterine disease |
Chest X-ray | FDG PET-CT ([18F] 2-fluoro-2-deoxy-D-glucose positron emission tomography) in suspected distant metastases |
Liver function and renal function tests | Immunohistochemistry (IHC) and microsatellite instability (MSI) screening to identify individuals at risk for Lynch syndrome |
Staging of Endometrial Cancer
Endometrial cancer is generally staged according to the International Federation of Gynecology and Obstetrics (FIGO) system [23]. In May 2009, a new staging system was published, replacing the previous staging of 1988 (Table 5.2).
Stage I | Tumor confined to the corpus uteri | ||
IA | NO or less than half myometrial invasion | ||
IB | Invasion equal to or more than half of the myometrium
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

| ||