Colorectal tumors exhibiting defective DNA mismatch repair (MMR-D)/microsatellite instability (MSI-H) form a distinct subgroup of CRCs associated with important clinical and pathologic features. The identification of MMR-D/MSI-H may impact CRC prognosis, prediction of response to chemotherapeutic agents, and may necessitate the need for genetic assessment for Lynch syndrome. Oncologists remain at the forefront of diagnosing, treating, and managing patients with MMR-D/MSI-H CRC and ensuring that the clinical care of these patients reflect our evolving understanding of this unique CRC subtype.
Key points
- •
Defective DNA mismatch repair (MMR-D), also referred to as microsatellite instability (MSI-H), is present in approximately 15% of colorectal cancers (CRCs).
- •
In most cases, MMR-D/MSI-H in colorectal tumors is caused by a noninherited epigenetic event; however, in about one-third of cases, it is caused by Lynch syndrome.
- •
Identification of MMR-D/MSI-H in patients with CRC may lead to a diagnosis of Lynch syndrome, with important clinical implications for future cancer surveillance and risk-reduction options for the patient as well as for at-risk family members.
- •
MMR-D/MSI-H is associated with distinct clinical and pathologic features, including right-sided colon predominance, early stage at diagnosis, prominent lymphocytic infiltrate, and a poorly differentiated mucinous adenocarcinoma, often showing a medullary component.
- •
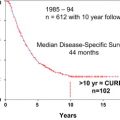
Although MMR-D/MSI-H in CRC is associated with a favorable prognosis, it also seems to predict for a lack of benefit from 5-fluorouracil chemotherapy.
Introduction
Colorectal cancers (CRCs) may be divided via molecular phenotyping into tumors with normal DNA mismatch repair (MMR) function and those with DNA MMR deficiency (MMR-D), representing ∼15% of CRCs. The hallmark of MMR-D CRC is a distinct type of genomic instability, referred to as high-frequency microsatellite instability (MSI-H). MMR-D/MSI-H is associated with specific clinical and pathologic features, and in some cases, may provide the initial clinical indication suggesting the presence of Lynch syndrome, an inherited form of CRC, characterized by germline genetic defects in one of the DNA MMR genes ( MLH1, MSH2, MSH6, PMS2, EPCAM ). Lynch syndrome remains significantly underdiagnosed, and recent measures to expand screening of patients with Lynch-associated cancers, including those with CRC and endometrial cancer, provides one of the most effective ways to identify at-risk families. The MMR-D/MSI-H phenotype also serves as an important prognostic and predictive marker in CRC. Although MMR-D/MSI-H CRCs tend to be early stage at diagnosis and are associated with a good prognosis, the value of 5-fluorouracil (5-FU) as an effective chemotherapeutic treatment of this type of CRC has been debated. As our understanding of MMR-D/MSI-H CRCs continues to evolve, oncologists remain at the forefront of diagnosing, treating, and managing patients with this unique subtype of CRC and ensuring that, for appropriate patients, referral to clinical cancer genetics for Lynch syndrome evaluation is implemented.
Introduction
Colorectal cancers (CRCs) may be divided via molecular phenotyping into tumors with normal DNA mismatch repair (MMR) function and those with DNA MMR deficiency (MMR-D), representing ∼15% of CRCs. The hallmark of MMR-D CRC is a distinct type of genomic instability, referred to as high-frequency microsatellite instability (MSI-H). MMR-D/MSI-H is associated with specific clinical and pathologic features, and in some cases, may provide the initial clinical indication suggesting the presence of Lynch syndrome, an inherited form of CRC, characterized by germline genetic defects in one of the DNA MMR genes ( MLH1, MSH2, MSH6, PMS2, EPCAM ). Lynch syndrome remains significantly underdiagnosed, and recent measures to expand screening of patients with Lynch-associated cancers, including those with CRC and endometrial cancer, provides one of the most effective ways to identify at-risk families. The MMR-D/MSI-H phenotype also serves as an important prognostic and predictive marker in CRC. Although MMR-D/MSI-H CRCs tend to be early stage at diagnosis and are associated with a good prognosis, the value of 5-fluorouracil (5-FU) as an effective chemotherapeutic treatment of this type of CRC has been debated. As our understanding of MMR-D/MSI-H CRCs continues to evolve, oncologists remain at the forefront of diagnosing, treating, and managing patients with this unique subtype of CRC and ensuring that, for appropriate patients, referral to clinical cancer genetics for Lynch syndrome evaluation is implemented.
The adenoma-carcinoma model of colorectal cancer
The development of CRCs via the adenoma-carcinoma sequence, initially described by Fearon and Vogelstein in 1990, proposed a multistep genetic model of CRC carcinogenesis. Most CRCs arise along the chromosomal instability pathway, characterized by widespread imbalances in chromosome number (aneuploidy) and loss of heterozygosity, as well as the accumulation of characteristic mutations in tumor suppressor genes and oncogenes critical for CRC initiation and progression. The second pathway, accounting for 15% to 20% of CRCs, results from defective DNA MMR, which leads to the molecular phenomenon of MSI-H shown within the tumor. Microsatellites are short, tandemly repeated DNA sequences that are distributed throughout the human genome and consist of mononucleotide, dinucleotide, or higher-order DNA base repeats. Such repetitive sequences are prone to the accumulation of mutations mostly because of base-base mismatches and insertion-deletion loops. The correction of errors in microsatellites is performed by the MMR proteins, the most notable of which are MLH1, MSH2, MSH6, and PMS2. In tumors with MMR-D, either because of germline, somatic, or epigenetic inactivation, the correction of such mutations is impaired, leading to the accumulation of DNA errors, resulting in the MSI-H phenotype.
In most cases, MMR-D is a result of an epigenetic phenomenon in the tumor, most commonly hypermethylation of the MLH1 promoter, which leads to the development of a sporadic (noninherited) CRC. However, in about 30% of cases, MMR-D is secondary to a germline mutation in one of the MMR genes, leading to a diagnosis of Lynch syndrome, an inherited form of CRC. Deciphering the cause of the MMR-D is of upmost importance, because it helps to differentiate sporadic from inherited forms of colon cancer.
Screening for defective DNA mismatch repair/high-frequency microsatellite instability in patients with colorectal cancer: should a universal approach be applied?
The identification of the MMR-D/MSI-H phenotype in a colorectal tumor may be the first indication that a patient may have a diagnosis of Lynch syndrome. Patients identified to have Lynch syndrome benefit from life-saving cancer surveillance measures. In addition, their at-risk family members would benefit from predictive genetic testing and, if needed, implementation of high-risk cancer surveillance. Although measures aimed at increasing awareness about hereditary CRC, both among individuals as well as among physicians, may be undertaken, one of the most effective ways to identify potential at-risk Lynch families is by evaluating patients who are diagnosed with either CRC or endometrial cancer, the 2 most common Lynch-associated malignancies.
Originally, the Amsterdam criteria and subsequently, the Revised Bethesda guidelines, have served as criteria to select patients with CRC or endometrial cancer in whom further evaluation for MMR-D/MSI-H was indicated. However, in the clinical setting these criteria have proved to be cumbersome to implement and lack specificity and sensitivity. Some groups have recommended expansion of the criteria for MMR/MSI testing to either universal testing, with testing of all patients with CRC, or to include all individuals with CRC diagnosed younger than 70 years. Using universal testing, Lynch syndrome was diagnosed in 2.4% to 3.7% of all unselected patients with CRC. Implementing universal screening for endometrial cancer yielded similar results, with about 1.8% to 3.9% of patients being diagnosed with Lynch syndrome. In the CRC cases, a Lynch syndrome diagnosis would have been missed in ∼12% to 28% of patients if the Revised Bethesda guidelines were used for selection criteria. More expansive testing of CRC and endometrial cases has also proved to be cost effective.
Based on these data, the Mallorca group, consisting of European experts in Lynch syndrome, the Evaluation of Genomic Applications in Practice and Prevention Working Group, and the National Comprehensive Cancer Network have recently updated their recommendations to suggest that either all patients with CRC or all patients with CRC younger than 70 years at diagnosis, and those 70 years or older who meet Bethesda guidelines, should undergo testing by either immunohistochemistry (IHC) or MSI for Lynch syndrome. Implementation of such reflex testing is already occurring across large medical centers, with a recent study suggesting that the specific implementation procedures influenced patient follow-through with genetic testing after an initial positive screening test. For example, institutions with a high level of involvement of genetic counselors in the tracking and communicating of screening results improved patient follow-through and reduced barriers to patient contact.
Identification of defective DNA mismatch repair/high-frequency microsatellite instability tumors
Two accepted methods for the detection of MMR-D are available. MSI testing relies on polymerase chain reaction for amplification of specific microsatellites repeats. The original accepted panel of 5 microsatellite markers, referred to as the Bethesda panel, includes 2 mononucleotides (BAT-25, BAT-26) and 3 dinucleotides (D5S346, D2S123, D17S250). The presence of instability is determined based on comparison of the length of a specific microsatellite marker in the tumor versus the normal DNA, such as adjacent colonic mucosa or a blood sample. Instability in 2 or more markers is defined as an MSI-high tumor, whereas those with 1 unstable marker are designated MSI low. For a sample to be microsatellite stable (MSS), no instability in any of the markers should be present. Given concerns over limited sensitivity of dinucleotide repeats, the 2002 National Cancer Institute workshop made further revisions, with recommendations to include a secondary panel of mononucleotide markers, such as BAT-40, to exclude MSI-low cases in which only a dinucleotide repeat is mutated.
In 1996, monoclonal antibodies against MMR proteins became available, rendering IHC detection of MMR proteins possible. A lack of expression of 1 or more of these proteins is diagnostic of MMR-D, with the specific pattern of expression also helping to pinpoint which gene is most likely to harbor a mutation or may be inactivated by another mechanism ( Table 1 ). Initial concerns over lower sensitivity of IHC as opposed to MSI screening have largely been overcome with the introduction of the 4-antibody panel (MLH1, MSH2, MSH6, PMS2). In the clinical setting, both IHC and MSI testing are used broadly and are essentially interchangeable techniques with greater than 90% concordance and similar sensitivity of around 85% to 92%. At our institution, the preference to use IHC as opposed to MSI testing for initial screening was largely based on the ability of IHC to pinpoint which genes should be targeted for subsequent germline analysis in MMR-D cases, thereby simplifying the genetic testing process.
| Protein Expression by IHC Staining | MMR Status | Most Likely Inactivated Gene | |||
|---|---|---|---|---|---|
| MLH1 | MSH2 | MSH6 | PMS2 | ||
| Present | Present | Present | Present | Proficient | None |
| Absent | Present | Present | Absent | Deficient | MLH1 (epigenetic or germline) |
| Present | Present | Present | Absent | Deficient | PMS2 |
| Present | Absent | Absent | Present | Deficient | MSH2 , possibly EPCAM |
| Present | Present | Absent | Present | Deficient | MSH6 |
Defective DNA mismatch repair/high-frequency microsatellite instability colorectal cancer: making the diagnosis of Lynch syndrome
An MSI-H or an abnormal IHC result does not distinguish between a somatic (sporadic) versus a germline (inherited) defect in the MMR system. Without further analysis, the cause of the defect remains elusive. In approximately two-thirds of cases, MSI-H indicates a sporadic CRC, with the molecular phenomenon being caused by an epigenetic event, most commonly MLH1 promoter hypermethylation, leading to MLH1 gene inactivation. In about 70% of such promoter hypermethylated MSI-H cases, the presence of a BRAF V600E mutation can be identified. The presence of a BRAF V600E mutation in a colorectal tumor would make the diagnosis of Lynch syndrome less likely, and together with an absence of suggestive family history, may reassure clinicians of the sporadic cause of the MSI-H CRC. Cases of BRAF mutated tumors in Lynch syndrome–associated CRCs have been reported, and therefore a careful review of the clinical and family history should be undertaken to determine whether further genetic counseling/testing is indicated. In many centers, an MSI-H CRC or a CRC showing loss of MLH1/PMS2 protein expression is immediately tested via direct MLH1 hypermethylation analysis or BRAF V600E mutation analysis. These are generally not considered genetic tests but are used for risk stratification to determine which patients may benefit from subsequent genetic testing.
In one-third of MSI-H tumors, the molecular defect is secondary to a germline mutation in one of the MMR genes, diagnostic of Lynch syndrome. In patients with CRC in whom Lynch syndrome is suspected based on early age at diagnosis or family history of Lynch-associated malignancies, an abnormal IHC or MSI-H result should prompt referral for genetic counseling and genetic testing. If IHC was performed, then the specific protein expression loss helps guide genetic testing (see Table 1 ). For example, in a tumor with absence of MSH2 and MSH6 expression, genetic testing for mutations in the MSH2 gene should be undertaken initially. Identification of a genetic mutation confirms the diagnosis of Lynch syndrome. In such patients, appropriate cancer surveillance and options for cancer risk reduction need to be reviewed and implemented. Moreover, expansion of genetic counseling and testing for family members should be undertaken.
A difficult clinical situation that arises not infrequently is that workup of a patient with an MSI-H or MMR-D CRC results in ambiguous or uninformative results with respect to the origin of the MMR defect. For example, in a young patient with CRC with absence of MLH1/PMS2 protein expression, genetic testing of the MLH1 and PMS2 genes may be unrevealing, with no mutation identified. Coupled with the absence of MLH1 promoter hypermethylation and absence of a BRAF mutation, in such a clinical circumstance, Lynch syndrome cannot be ruled out. In such situations, a careful evaluation of the family history may help to identify other cancer-affected family members whose tumors could be evaluated for the MMR-D/MSI-H molecular signature and, if positive, would confirm the presence of an occult mutation. These cases require the careful input of genetic counselors and cancer geneticists for recommendations for appropriate cancer surveillance for both the patient and at-risk family members.
Clinical and pathologic features of defective DNA mismatch repair/high-frequency microsatellite instability colorectal cancers
Regardless of the cause of the MMR deficiency, MMR-D/MSI-H CRCs seem to be associated with distinct clinical and pathologic features, which often serve as the initial clue that a particular tumor may harbor an MMR defect ( Table 2 ). As opposed to the 25% of MSS colorectal tumors, 85% of MMR-D/MSI-H tumors are proximal to the splenic flexure. Moreover, the age distribution of MMR-D/MSI-H tumors seems to be bimodal, with about 24% of patients with CRC younger than 40 years and 19% older than 70 years having MSI-H tumors, as opposed to only 8% of patients with CRC aged between 50 and 59 years. This U-shaped age distribution reflects the higher prevalence of Lynch-associated MMR-D/MSI-H CRCs in young patients and the similarly higher prevalence of sporadic MMR-D/MSI-H phenotype observed in older patients.