The UK National Screening Committee (NSC) has produced grading criteria describing various levels of disease (Box 37.1).
Background retinopathy (R1)
The early changes in diabetic retinopathy include death of the retinal pericytes, thickening of the retinal basement membrane and impairment of its function. Pericytes are mesenchymal-like cells that support the walls of small blood vessels.
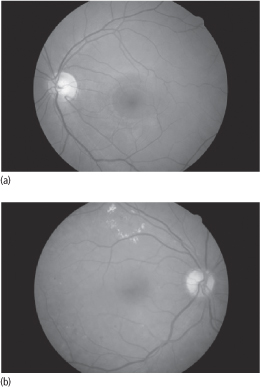
These changes are associated with the formation of retinal capillary microaneurysms (outpouchings of retinal capillaries with weakened walls partly due to pericyte loss) and increased vascular permeability, resulting in the leakage of lipid and proteinaceous material (hard exudates) (Fig. 37.1). Capillary leakage often spreads in a circinate pattern.
Figure 37.1 (a) Normal retina with no retinopathy (NSC grade R0). (b) Background retinopathy with microaneurysms, haemorrhages and hard exudates (NSC grade R1)
The initial stage of cell death may be followed by cycles of renewal and further cell death. The intraluminal proliferation of cells, as well as changes in platelet function, erythrocyte aggregation and high plasma fibrinogen levels, can cause vascular occlusion and rupture. This can result in small flame-shaped and blot haemorrhages proximal to the occlusion.
Preproliferative retinopathy (R2)
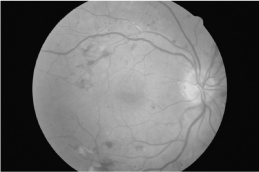
Intraretinal infarcts (cotton wool spots or soft exudates) may occur distal to microvascular occlusions (Fig. 37.2). Proliferation of the endothelial cells of retinal veins results in venous calibre abnormalities, such as venous beading, loops and dilation. Intraretinal microvascular abnormalities (IRMAs) are dilated capillaries that occur in response to retinal ischaemia.
Figure 37.2 Preproliferative retinopathy (NSC grade R2) with cotton wool spots, intraretinal microvascular abnormalities and multiple blot haemorrhages.
Proliferative retinopathy (R3)
Progressive microvascular occlusion and retinal ischaemia results in an increased release of vasoproliferative substances such as IGF-1 and VEGF, which promote the formation of new vessels (neovascularization). New vessels (Fig. 37.3) can arise from arteries or veins. The new vessels form a lace-like pattern with a fine mesh of fibrous tissue connecting them. There are two main risks associated with new vessel formation:
- Pre-retinal or vitreous haemorrhage: the new vessels are fragile and therefore prone to rupture.
- Retinal detachment: as new vessels mature, the fibrous component becomes more prominent, resulting in contraction.
New vessel proliferation can also occur on the surface of the iris and in the anterior chamber. The latter change can cause glaucoma by blocking the outflow of the aqueous humour.
Maculopathy (M1)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree