Fig. 7.1
Pathway of choline metabolism in normal and cancer cell (Cho choline, ChAT choline acetyltransferase, ACho acetylcholine, ChoK choline kinase, CMP cytidylate, DAG diacylglycerol, PCho phosphocholine, CDP diphosphocholine, PPi Inorganic pyrophosphate, PC phosphocholine, PA phosphatic acid, PLD phospholipase D)
Choline radiopharmaceuticals can be labelled by both 11C (11C-CHO) and 18F (18F-CHO). The most striking difference between the two tracers is the urinary elimination that is high for 18F-CHO, being an important disadvantage for imaging prostate region. Conversely, 18F-CHO imaging has the advantage of a longer half-life (approximately 110 min versus 20 min of 11C-CHO) allowing transportation from one single cyclotron centre to several PET centres [3, 4]. 18F-CHO provides more flexibility concerning imaging protocols and availability and presents a very similar behaviour to 11C-CHO in prostate cancer patients. Both 11C- and 18F-CHO PET/CT are actually an established imaging modality in the evaluation of patients with prostate cancer [5, 6].
7.2 Diagnostic Accuracy of Radiolabelled Choline in Skeletal Metastases
Although most studies of choline in prostate cancer evaluated localised or lymph node disease [7, 8], their results provided additional evidence to support the use of choline also for the detection of early osseous metastatic disease in newly diagnosed and recurrent prostate cancer patients [9]. In a retrospective analysis, 11C-CHO PET/CT was valuable in the assessment of metastatic bone disease in terms of detection, localisation and characterisation [10]. It remains unclear whether 11C-CHO PET/CT is more sensitive than conventional BS, but it has higher specificity, with fewer indeterminate lesions [6, 11, 12]. 11C-CHO PET/CT may detect multiple bone metastases in patients showing a single metastases on bone scan and may be positive for bone metastases in up to 15 % of patients with biochemical failure after radical prostatectomy and negative bone scan [13]. The specificity of 11C-CHO PET/CT is also higher than bone scan with less false-positive and indeterminate findings [14, 15]. An important advantage of CHO PET/CT is the opportunity to discover the presence of medullary bone involvement, before that the cortical part is taken. Fig. 7.2 is reported in example of a patient with bone medullary involvement at 18F-CHO PET/CT that was later confirmed by MRI.
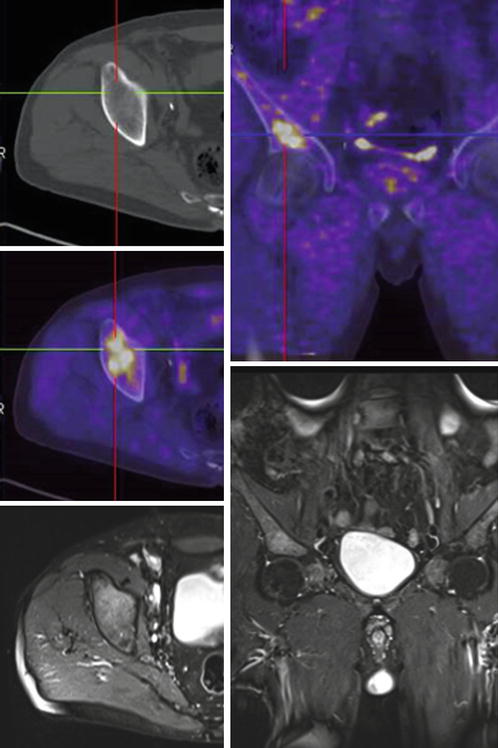
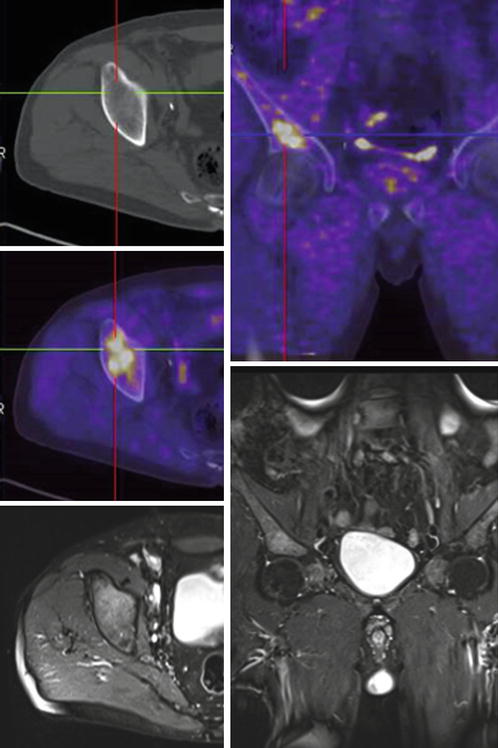
Fig. 7.2
A 78-year-old man underwent 18F-CHO PET/CT for a biochemical recurrence of prostate cancer. A significant uptake of CHO was shown in the right ischium (up; left and right), without any morphological changes at co-registrated CT images (up, left). An MRI scan confirmed the presence of medullary involvement in the same site (down, left and right) (Courtesy Dr. Laura Evangelista, Nuclear Medicine and Molecular Imaging Unit, Veneto Institute of Oncology IOV – IRCCS, Padua, Italy)
Beheshti et al. have investigated whether 18F-CHO PET/CT is of value for the detection of bone metastases and found that 18F-CHO PET/CT showed a sensitivity, specificity and accuracy of 79 %, 97 % and 84 % [16]. Onyeuku et al. observed similar radiographic results to Beheshti et al. when compared to conventional methods in two of the four patients with positive findings on imaging [17]. In a recent study by Kjolhede et al., 90 high-risk prostate cancer patients presenting a negative or inconclusive bone scan underwent 18F-CHO PET/CT [18]. Authors concluded that choline PET/CT imaging could detect metastases in high-risk prostate cancer patients with negative or inconclusive bone scan, with a change in the planned treatment (from curative to palliative) in 20 % of them. Poulsen et al. [19] evaluated the value of 18F-CHO PET/CT in the initial staging of 210 patients. Even if the goal of the study was to assess the value of PET/CT in lymph node staging, authors underlined that a high focal bone uptake, consistent with bone metastases, was seen in 18 patients, 12 of which presented histologically proven benign lymph nodes. However, 18F-CHO presented limitations in detecting densely sclerotic malignant lesions [14]. In particular, in restaging prostate cancer, both 11C- and 18F-CHO PET/CT have been demonstrated to be superior to 18F-FDG PET/CT in detecting recurrences, including bone metastatic lesions (Figs. 7.3, 7.4 and 7.5) [20].
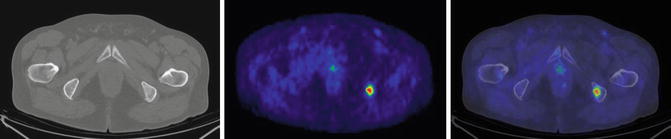
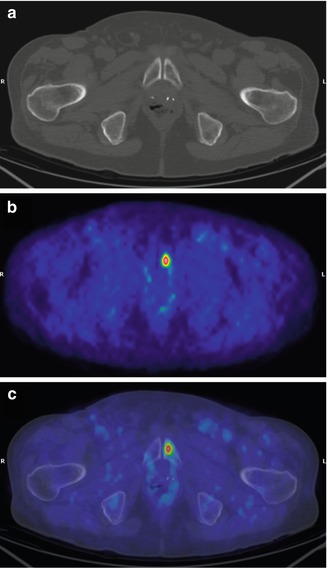
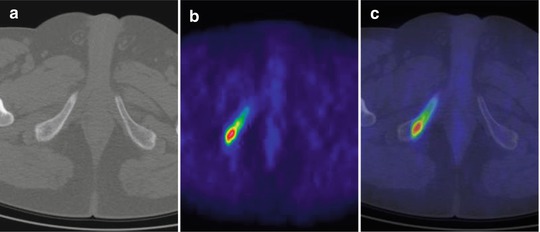
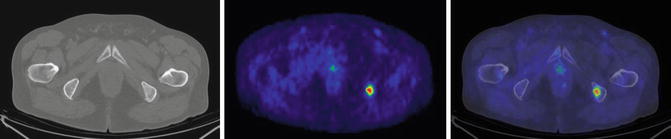
Fig. 7.3
A 61-year-old man treated with radical prostatectomy for prostate cancer (GS 7 (4 + 3), pT2cR1N0), who performed 11C-CHO PET/CT for biochemical recurrence (PSA: 14.62 ng/mL). 11C-CHO PET/CT showed a pathological uptake in the left ischial tuberosity as documented on CT (a), PET (b) and PET/CT-fused (c) transaxial images. After androgen deprivation therapy (PSA: 0.07 ng/mL), helical tomotherapy (HTT) was performed on the positive 11C-CHO PET/CT lesion. One year after HTT, patient showed a complete response with a PSA value of 0.03 ng/mL
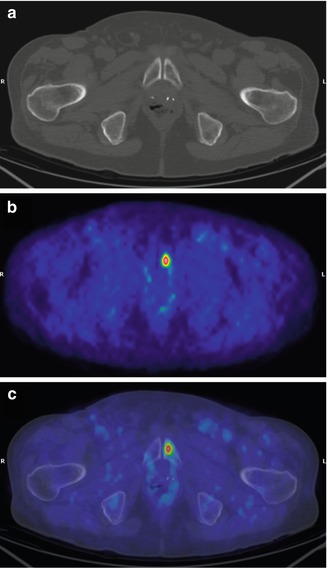
Fig. 7.4
A 75-year-old man treated with radical prostatectomy for prostate cancer (GS 7 (3 + 4), pT2cN0), who performed 11C-CHO PET/CT for biochemical recurrence (PSA: 4.00 ng/mL). 11C-CHO PET/CT showed a pathological uptake in the left groyne as documented on CT (a), PET (b) and fused PET/CT (c) transaxial images. After androgen deprivation therapy (PSA: 0.60 ng/mL), helical tomotherapy (HTT) was performed on the positive 11C-CHO PET/CT lesion. Nine months after HTT, patient showed a complete response with an undetectable PSA serum value
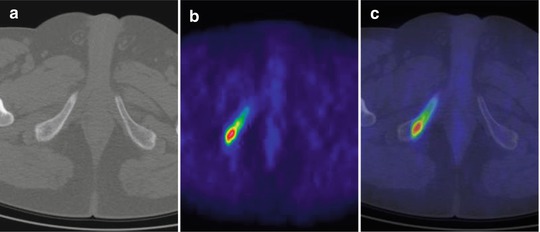
Fig. 7.5
A 57-year-old man treated with radical prostatectomy for prostate cancer (GS 7 (4 + 3), pT3aN0), who performed 11C-CHO PET/CT for biochemical recurrence (PSA: 15.14 ng/mL). 11C-CHO PET/CT showed a pathological uptake in the right ischio-pubic branch as documented on CT (a), PET (b) and fused PET/CT (c) transaxial images. After androgen deprivation therapy (PSA: 0.63 ng/mL), helical tomotherapy (HTT) was performed on the positive 11C-CHO PET/CT lesion. Two years after HTT, patient showed a complete response with a PSA value of 0.03 ng/mL
Picchio et al. showed that 11C-CHO PET/CT exhibits a lower sensitivity but a higher specificity than those of bone scan in the detection of bone metastases in prostate cancer patients with biochemical progression. Equivocal findings occurred in 1 of 78 (1 %) cases in 11C-CHO PET/CT and in 21 of 78 (27 %) cases in bone scan. Depending on their attribution as either positive or negative, the ranges of sensitivity, specificity, positive predictive value, negative predictive value and accuracy for 11C-CHO PET/CT were 89–89 %, 98–100 %, 96–100 %, 94–96 % and 95–96 %, respectively. For bone scan they were 100–70 %, 75–100 %, 68–100 %, 100–86 % and 83–90 %, respectively. Concordant findings between 11C-CHO PET/CT and bone scan occurred in 55 of 78 (71 %) cases [6]. Fig. 7.6 is reported with discordant images between 18F-CHO PET/CT and bone scan.
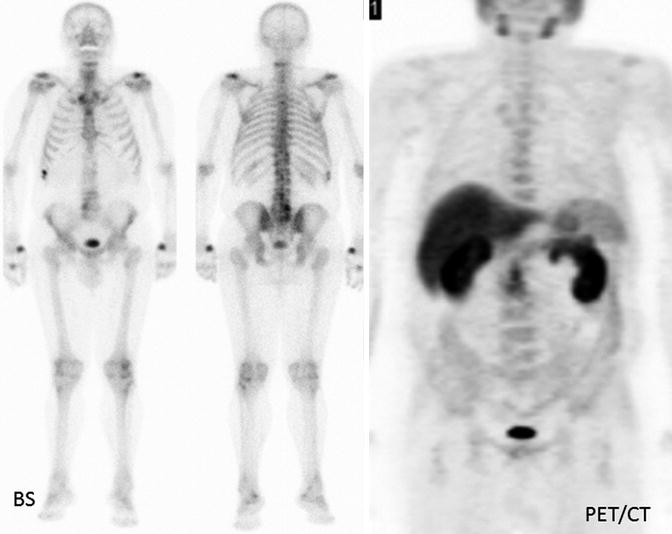
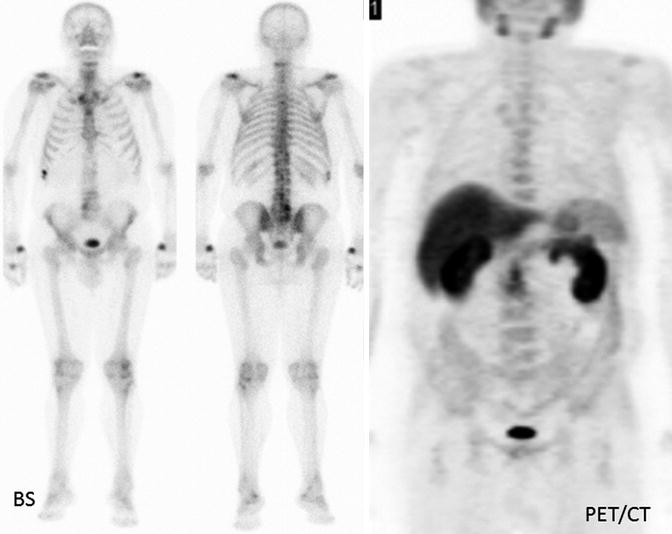
Fig. 7.6
A 65-year-old man with a suspicion for bone recurrence at bone scan was sent to 18F-CHO PET/CT. PSA level at the time of bone scan was 2.3 ng/mL. Bone scan resulted falsely negative, while PET/CT was truly negative (Courtesy Dr. Laura Evangelista, Nuclear Medicine and Molecular Imaging Unit, Veneto Institute of Oncology IOV – IRCCS, Padua, Italy)
Another PET tracer, 18F-fluoride, traditionally used in the evaluation of bone metastases, showed a better sensitivity compared with traditional bone scan. However, 18F-fluoride PET/CT scans suffer from the same lack of specificity of bone scan. Poulsen et al. [21] studied detection of spine metastases with 18F-fluoride, 18F-CHO and bone scan and found that 18F-fluoride is superior in sensitivity to 18F-CHO (93 vs 85 %). However, 18F-CHO is superior to 18F-fluoride in specificity (81 vs 91 %). Both tracers were better than bone scan in hormone-naïve patients. Thus, 18F-fluoride PET is most useful in high-risk patients to confidently detect or eliminate bone disease and potentially monitor the effects of therapy on bone metastases. In another review by Wondergem et al. [5], data on the performances of 11C- or 18F-CHO and 18F-fluoride PET/CT in bone metastases detection has been reported. On a lesion basis, authors reported sensitivity and specificity rates of 84 % and 98 % for 11C-CHO and 18F-CHO and 89 % and 91 % for 18 F-fluoride, respectively. On a patient basis, the reported sensitivity and specificity rates were 85 % and 96 % for 11C-CHO and 18F-CHO and 87 % and 80 % for 18F-fluoride, respectively. No significant differences were found between the sensitivity and specificity of 11C-CHO or 18F-CHO and 18F-fluoride reporting a general high sensitivity for PET/CT [14, 22–24]. In addition, Ceci et al. also evaluated the semi-quantitative data of 11C-CHO in 304 bone lesions (184 osteoblastic, 99 osteolytic and 21 bone marrow lesions) of 140 patients during biochemical recurrence. They could demonstrate differences in PSA kinetics and SUVmax between osteolytic (higher values) and osteoblastic (lower values) lesions. 11C-CHO PET/CT may identify patients that could benefit from early targeted therapies, depending on the type of bone lesions expressed [25]. The reported method could also help in delineating the extension and severity of skeletal involvement and classifying lesions as predominantly osteoblastic, lytic or mixed type, with crucial impact on treatment plan. In the management of prostate cancer patients, radiotherapy (RT) and diagnostic imaging have always enjoyed a close relationship: advances in diagnostic imaging and RT techniques have in fact resulted in a significant improvement of planning delineation [26, 27]. In general, PET may improve the target definition with a decrease in inter-observer variations, also in bone lesions, being potentially considered as a valuable tool in guiding tailored treatment on bone metastatic lesions [28–32]. Beheshti et al. comparing 18F-CHO and 18F-fluoride in 38 patients with biopsy-proven prostate cancer documented a sensitivity, specificity and accuracy in the detection of bone metastases of 81 %, 93 % and 86 % for 18F-fluoride and 74 % (p = 0.12), 99 % (p = 0.01) and 85 % for 18F-CHO, respectively. In addition, 18F-CHO could lead to a change in the management in two out of 38 patients due to the early detection of bone marrow metastases [14].
7.3 Response to Treatment with Radiolabelled Choline Agents
Oligometastatic subjects are a group of prostate cancer patients with a limited number of metastases (≤3 lesion). The number of metastases may reflect the biological aggressiveness of the tumour and may determine the possibility of curative potential interventions such as surgery or high-dose targeted RT [33]. However, there are very few data on the irradiation of oligometastases in recurrent disease, and they are mainly exclusively focused to lymph node lesions [34–36]. Interestingly, the extent of osseous metastatic disease is an independent prognostic factor in evaluating newly diagnosed advanced prostate cancer [37, 38]. A recent study showed that skeletal complications result in significant decreases in quality-of-life scores [39]. Therefore, therapies preventing skeletal complications could translate into improvements in quality of life and prolong physical activity. Besides analgesics, different treatment options are available for further palliation in case of symptomatic local and systemic progression. They include drug treatment, surgery, chemotherapy, hormonal therapy, RT and radionuclide treatment. It has been reported that androgen deprivation therapy (ADT) is strongly associated with bone metabolism modifications in prostate cancer, significantly decreasing bone mineral density [40]. In addition to conventional treatments, in patients with bone oligometastatic disease, a tailored approach on bone lesions by using either high-dose targeted RT or surgery could be proposed when an accurate imaging is available. Choline PET/CT can be a valuable imaging technique to monitor the disease in prostate cancer patients, as reported in a study in 40 patients with 64 bone metastases referred to after image-guided single fraction robotic stereotactic radiosurgery. The advantage of PET/CT in the evaluation of bone metastases is that this method combines the detection and the morphologic assessment of bone lesions with information concerning the metabolic activity of the metastases and can help to triage patients with metastatic prostate cancer and also in the evaluation of therapy response [41]. The potential influence of anti-androgenic treatment in patients who undergone 11C-CHO PET/CT study is still controversial. A significant reduction of 11C-CHO uptake following treatment with the nonsteroidal androgenic antagonist bicalutamide has been reported during the staging phase of prostate cancer patients [42]. In particular, in a series of 14 hormone-sensitive patients with recurrent prostate cancer, it was stated that ADT influences the uptake of 11C-CHO PET/CT [43]. Berkovic et al. [44] investigated whether repeated stereotactic body RT (SBRT) of oligometastatic disease is able to defer the initiation of ADT in patients with low-volume metastases. They enrolled 24 recurrent prostate cancer patients with biochemical recurrence after radical therapy and 1–3 synchronous metastases (bone and/or lymph nodes) assessed by 18F-CHO PET/CT.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree