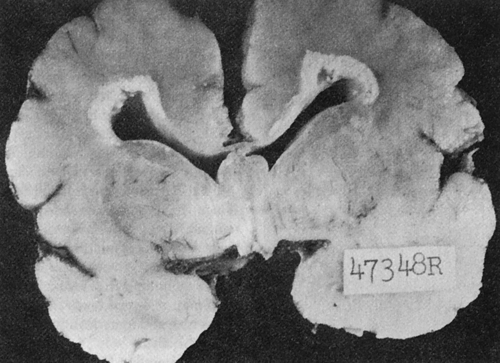
At the conclusion of this chapter, the reader should be able to: • Discuss the etiology and epidemiology of acquired, latent, and congenital cytomegalovirus (CMV) infection. • Explain the signs and symptoms of acquired and congenital CMV infections. • Describe the immunologic manifestations of CMV. • Identify and explain the serologic markers and diagnostic evaluation of CMV. • Discuss the principles and applications of passive latex agglutination and other quantitative determinations of IgM and IgG antibodies. • Correctly answer case study related multiple choice questions. • Be prepared to participate in a discussion of critical thinking questions. • Describe the principle, reference range, sources of error, limitations, and clinical applications of Latex Agglutination for Antibodies to CMV. • Describe the principle and clinical applications of antibody detection to CMV. 1. Primary infection occurs when a previously unexposed (seronegative) recipient is transfused with blood from an actively or latently infected donor. This type of infection is accompanied by the presence of virus in the blood and urine, an immediate antibody response, and eventual seroconversion. Patients with primary infections may be symptomatic, but the great majority are asymptomatic. 2. Reactivated infection can occur when a seropositive recipient is transfused with blood from a CMV antibody–positive or –negative donor. Donor leukocytes are thought to trigger an allograft reaction, which in turn reactivates the recipient’s latent infection. These infections may be accompanied by significant increases in CMV-specific antibody. Some reactivated infections exhibit viral shedding as their only manifestation. Reactivated infections are largely asymptomatic. 3. Reinfection can occur by a CMV strain in the donor’s blood that differs from the strain that originally infected the recipient. A significant antibody response is observed and viral shedding occurs. Although it is difficult to differentiate a reactivated infection if the patient and donor are CMV antibody–positive before transfusion, reinfections can be documented if isolates can be obtained from the donor and recipient. The classic congenital CMV syndrome is manifested by a high incidence of neurologic symptoms, as well as neuromuscular disorders, jaundice, hepatomegaly, and splenomegaly (Fig. 21-1). Petechia is the most common clinical sign, seen in about 50% of CMV-infected infants. Congenitally infected newborns, especially those who acquire CMV during a maternal primary infection, are more prone to develop severe cytomegalic inclusion disease (CID). The severe form of CID may be fatal or can cause permanent neurologic sequelae, such as intracranial calcifications (Fig. 21-2), mental retardation, deafness, vision defects, microcephaly, and motor dysfunction. Psychomotor impairment is seen in 51% to 75% of survivors. Hearing loss is observed in 21% to 50% and visual impairment in 20% of patients. Infants without symptoms at birth may develop hearing impairment and neurologic impairment later.
Cytomegalovirus
Signs and Symptoms
Acquired Infection
Congenital Infection
Oncohema Key
Fastest Oncology & Hematology Insight Engine