Fig. 3.1
A colloid goiter showing a colloid droplet and clusters of typical follicular cells (LBC, Pap, 300×)
The cytological findings of a nodular lesion in Graves’s disease is not specific similar to a benign goiter sometimes with the presence of lymphocytes and oncocytes in the background. The keystone feature is the presence of flame cells characterized by marginal cytoplasm vacuoles with red frayed edges.
Chronic lymphocytic (Hashimoto’s) thyroiditis is characterized by a variable amount of lympho-monocytic cells in the background admixed with oxyphilic cells. When a thyroiditis is suspected, the detection of lympho-epithelial clusters in an inflammatory background is the pivotal clue for the diagnosis on LBC slides [15, 22–25]. Oxyphilic hyperplastic nodules in a thyroiditis should not be surgically removed because they represent the functional replacement of the parenchyma infiltrated by the inflammatory cells. Thus, the identification of oxyphilic cells in a background of inflammatory cells virtually does rule out an oxyphilic neoplasm and warrants a simple follow-up for the patient [15, 17].
Granulomatous De Quervain’s and Riedel’s thyroiditis are less common variants of inflammatory diseases of the thyroid which can be encountered in the routine practice [26, 27].
Clinical and US follow-up are suggested for non-neoplastic nodules. Repeat FNA is recommended in case of nodule growth or structural changes, and in patients who are undergoing ablative treatments [17].
3.3 Indeterminate Lesions
Numerous studies demonstrated that indeterminate lesions (IL) may account for up to 20 % of cytological diagnoses and they represent a “gray zone” in which both benign and malignant entities are included, especially PTC and its variants [28, 29]. The surgical treatment of IL results in a high number of unnecessary thyroidectomies which may cause additional morbidity and increase of health care costs [28–30]. The impossibility to evaluate any capsular or vascular invasion, which is the cornerstone of the diagnosis of differentiated carcinoma, represents a major limit of morphology and decreases the overall diagnostic accuracy of FNAC.
An articulate debate on this IL category has emerged in a number of new classification systems for reporting thyroid cytopathology leading to a division in subcategories with different risks of malignancy [28–31]. The Bethesda Reporting System for Thyroid Cytology (TBRSTC) subclassified IL in three categories: (1) atypia of undetermined significance and follicular lesions of undetermined significance (AUS/FLUS); (2) follicular neoplasms or suspicious for follicular neoplasm (FN/SFN); and (3) suspicious for malignancy (SM). The two published European classifications, with different definitions, have kept the distinction of IL in three categories [17, 30, 31].
The diagnosis of IL is based upon the identification of microfollicles made up of medium-sized thyrocytes in a background with scant colloid (Fig. 3.2).
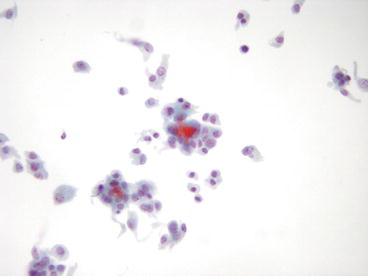
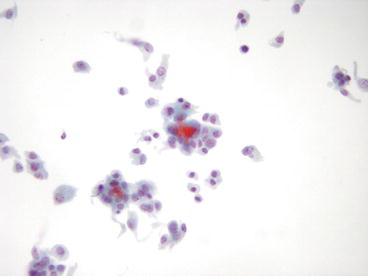
Fig. 3.2
Microfollicular aggregates of thyroid cells from a follicular neoplasm (LBC, Pap, 300×)
In this category there is an almost complete agreement in the different classification systems in terms of malignancy risk (between 15 and 30 %). A general consensus was evident in the therapeutic action of the surgical removal of the lesion, preferably after a collegial discussion. At histology an indeterminate lesion may correspond to both a follicular adenoma or an adenomatous nodule in a goiter (70–80 % of cases) although on a morphological basis a follicular carcinoma or a follicular variant of a papillary carcinoma cannot be ruled out.
An advantage of the LBC technique in IL is the possibility to apply additional investigations (immunocytochemistry, flow cytometry, molecular biology) to the cells left in the vial and these procedures are particularly helpful in defining the malignant risk of the lesion (see below) [11, 32–34]. Our recent experience involving an immunocytochemical panel made up of HBME-1 and Galectin-3 pointed to an 81 % overall diagnostic accuracy in discriminating between low and high risk of malignancy in follicular proliferations, which increased to 92 % when a concordant positive panel was applied [11, 33, 34].
TBRSTC includes, in the IL category, the “follicular lesion with undetermined significance (FLUS)” or “atypical cells of undetermined significance (ACUS or AUS).” The morphological criteria for diagnosing AUS/FLUS of TBRSTC was based on smears with cells showing architectural and/or nuclear atypia that are not sufficient to be classified as suspicious for follicular neoplasm [28, 29, 35–37]. The reasons for enclosing a case in this category are briefly three: (1) technical problems including poor preservation or drying, artifact; (2) some atypical features but the amount of material is scant for a diagnosis; (3) atypia may be architectural or cytologic [28]. The low malignant risk indeterminate category has been only recently included in the European classifications although some papers concerning the efficacy of the AUS/FLUS category of the Bethesda system underline some difficulties in a correct definition of this category and that some studies have reported malignancy rates similar to the follicular neoplasm category [22].
The same diagnostic criteria and therapeutic actions are applied to indeterminate lesions composed mostly by oxyphilic (or Hurthle) cells (see Sect. 3.3). Smears of an oxyphilic lesion are categorized as “Oxyphilic or Hurthle cell neoplasm” when more than 90 % of the component are oxyphilic cells. These cells may feature nuclear enlargement and pleomorphism which are clinically irrelevant since they can be found in benign neoplasms or even in hyperplastic lesions [15, 38–40].
Recent studies support the idea that the majority of oxyphilic neoplasms histologically represent oxyphilic adenomas thus these nodules might be only followed-up instead of being surgically removed [40].
The clinical recommendation for IL of low malignant risk (FLUS/AUS, Thy 3f, TIR 3A) is follow-up in most cases. During the follow-up repeat FNA is recommended (after 6 months in the Bethesda classification) [17, 28, 31, 41]. Surgery is the recommended option for IL of high malignant risk and oxyphilic neoplasms (FN/SFN, HCN/SHCN, Thy 3a, TIR 3B). Frozen section examination is generally not recommended [17, 28, 31, 41].
3.4 Suspicious for Malignancy
This category is one of the three subgroups of IL [17, 28, 31, 41]. These cases exhibit some features consistent for a diagnosis of papillary carcinoma but lack the presence of the major criterion (nuclear pseudoinclusions or “Orphan Annie’s eye”). These cases bear a risk of malignancy ranging between 60 and 80 %. With a diagnosis of SM the surgical consultation is strongly recommended. The intraoperative frozen section examination may be considered. Repeat FNA may be performed either in cases with poor cellularity or in those needing additional techniques for a better characterization.
3.5 Malignant Neoplasms
Thyroid malignancy represents 4–8 % of all FNAC and the majority of them (90 %) are papillary thyroid carcinoma. The diagnostic accuracy of FNAC is at about 96–100 % [28, 42–45]. This tumor type and its variants (follicular variant of PTC, Tall cell PTC, macrofollicular PTC) show evidence of follicular differentiation with the typical distinctive nuclear features.
The most important and common malignant tumor which should be appropriately identified is papillary thyroid carcinoma (PTC). This entity accounts for 80 % of all cancers. The LBC diagnosis of PTC is straightforward when the nuclear pseudo-inclusions (major criterion) are detected even within tridimensional clusters of cells with nuclear elongation and clearing (Fig. 3.3) [28, 29]. Papillary structures, multinuclear giant cells, typical “chewing-gum” colloid, and psammoma bodies are seldom identified.
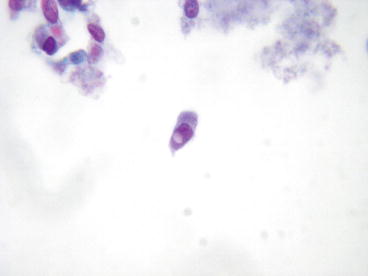
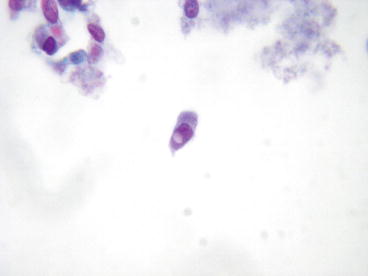
Fig. 3.3
In the center a PTC cell with the distinctive nuclear inclusion (Orphan Annie’s eye) (LBC, Pap, 500×)
In this group we can include also the cystic variant of PTC in which the cytological smear includes also histiocytes, watery fluid, and macrophages. The diagnosis is based on the evidence of convincing nuclear features of PTC [28].
Major difficulties might be encountered in the diagnosis of a follicular variant of PTC (FVPC) because of the lack of the typical parameters. The major misleading parameter is the absence of papillary structures and the bland nuclear features which may fall short of a correct diagnosis. All the morphological parameters are subtler than on classical PTC smear.
The variants of PTC include either tumor types which share the same prognosis and therapeutical options of the two most important variants presented above (macrofollicular, oncocytic, and cystic variants) and a few histotypes which pursue a more aggressive course (tall cell, columnar cell, and diffuse sclerosing variants). Regardless of the prognostic outlook, all these tumors show the same nuclear features of PTC so that the diagnosis is virtually always possible in the preoperative phase [42–45].
The poorly differentiated category of malignant neoplasm was proposed by Carcangiu as an intermediate malignancy between differentiated follicular neoplasms and anaplastic carcinomas [46, 47]. This category shows a variety of different degree of pleomorphic features.
Anaplastic thyroid carcinoma (ATC) is a rare and extremely aggressive thyroid carcinoma. It accounts for less than 5 % of all thyroid carcinoma with a very poor outcome and most of the patients succumb in a period of 1 year. This entity is an uncommon finding in thyroid cytology as this tumor presents a rapid growth which frustrates the attempts to plan a surgical strategy [48]. Cytological smears are composed of variable cellularity made up of large undifferentiated polygonal or spindle cells mixed with necrotic debris. The aggregation of these cells and their large cytoplasms help in distinguishing ATC from large-cell non-Hodgkin malignant lymphoma, which represents, from a clinical and morphologic viewpoint, the most important differential diagnosis.
Medullary thyroid carcinoma (MTC) represents 7 % of all thyroid carcinomas and can appear as a sporadic (75 %) or familiar disease (25 %) with a dominant autosomal mode of inheritance [49, 50]. The cytological diagnosis of MTC relies on the identification of a population of both plasmacytoid and spindle cells with variable nuclear pleomorphism. The typical amyloid substance with dense, amorphous texture may be present. Although the diagnosis of MTC can be suggested by morphology alone, it is advisable to confirm it by the immunocytochemical evaluation which offers the opportunity to identify calcitonin and CEA in the neoplastic cells [49–51].
A miscellaneous group may include both benign and malignant conditions. One of the most controversial is hyalinizing trabecular tumor (HTA) which is a rare follicular derived neoplasm which shows trabecular pattern, intratrabecular hyalinization, and some nuclear features of PTC. For this reason, some authors consider it as a variant of PTC with a benign course [51].
Primary thyroid lymphomas account for 5 % of all thyroid tumors and 2.5–7 % of all extrathyroid lymphomas [52].. Both Hodgkin’s disease and non-Hodgkin lymphoma may affect the thyroid gland although the latter outnumbers the first entity. Several papers report that diffuse large-cell lymphomas, extranodal marginal zone B-cell lymphoma or mixed patterns are the most frequent types. Other types have also been reported including follicular and Burkitt’s lymphoma.
The smear is cellular with prevalence of round non-cohesive lymphocytes. Their nuclei show coarse chromatin with prominent nucleoli and in some types, large basophilic cytoplasms may be detected (diffuse large B-cell lymphoma). The use of immunocytochemical markers for lymphoid lineage (LCA, CD20, bcl-6, and others) reveals a monoclonal phenotype and is helpful in the correct diagnosis. The main difficult differential diagnosis is with Hashimoto’s thyroiditis and anaplastic carcinoma. The combining evaluation of morphology and application of ancillary techniques represent the keystone for the correct diagnosis.
3.6 Reporting Systems for Thyroid Cytology
The need of a clarity of communication led to some classification systems in order to obtain a succinct, unambiguous, and clinically useful interpretation of the FNAC [17, 22, 28–31, 56].
An articulate debate was delivered for the follicular neoplasm category as emerged in a number of new classification systems for reporting thyroid cytopathology which led to a division in subcategories with different risks of malignancy [17, 19, 21, 28–31, 41].
In this regard several classifications with different tiered schemes were discussed including the proposals of the Papanicolaou Society, the American Thyroid Association, the American Association of Clinical Endocrinologists and the British Thyroid Association [28–31]. As discussed in the FN section, a conclusion was reached by the National Cancer Institute (NCI) State of the Science conference in which the Bethesda System of Reporting Thyroid Cytopathology proposed three subcategories of the follicular/indeterminate neoplasms including (1) follicular lesions of indeterminate significance or atypia of undetermined significance (AUS); (2) follicular neoplasms and hurtle cell neoplasms (FN); (3) suspicious for malignancy (SM). The stratification of cancer risk for each of these categories ranged from 5 to 75 % [23, 24, 32]. However, as emerged by several papers, one of the limit of this subclassification of FN is the difficult reproducibility of the criteria even among expert cytopathologists [17, 19, 21, 28–31, 41].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree