Gestational trophoblastic neoplasms are malignant lesions that arise from placental villous and extravillous trophoblast. Four clinicopathologic conditions make up this entity: invasive mole (IM), choriocarcinoma (CCA), placental-site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor (ETT). IM and CCA, which make up the majority of these tumors, are highly responsive to chemotherapy with an overall cure rate exceeding 90%, making it usually possible to achieve cure while preserving reproductive function. PSTT and ETT, which rarely occur, are relatively resistant to chemotherapy, making surgery the primary treatment modality, chemotherapy being used only when the disease has metastasized.
Gestational trophoblastic neoplasms (GTN) are malignant lesions that arise from placental villous and extravillous trophoblast. Four clinicopathologic conditions make up this entity: (1) invasive mole, which follows either complete hydatidiform mole (CHM) or partial hydatidiform mole (PHM), (2) choriocarcinoma (CCA), (3) placental-site trophoblastic tumor (PSTT), and (4) epithelioid trophoblastic tumor (ETT). Each of these conditions can perforate the uterine wall, metastasize, and lead to death if left untreated. Approximately 50% of cases of GTN arise from molar pregnancy, 25% from miscarriage or tubal pregnancy, and 25% from term or preterm pregnancy. Invasive mole and CCA, which make up the majority of these tumors, always produce easily detectable amounts of human chorionic gonadotropin (hCG) and are highly responsive to chemotherapy with an overall cure rate exceeding 90%, making it usually possible to achieve cure while preserving reproductive function. This success is attributable to several factors, the most important of which are the unique sensitivity of these two trophoblastic neoplasms to chemotherapeutic agents and the use of hCG as a tumor marker for diagnosis, monitoring treatment, and follow-up. By contrast, PSTT and ETT, which rarely occur, produce scant amounts of hCG and are relatively resistant to chemotherapy, making surgery the primary treatment modality. Chemotherapy is used for PSTT and ETT only when the disease has metastasized.
Epidemiology
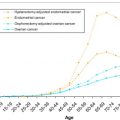
The incidence and etiologic risk factors that contribute to the development of GTN have been difficult to characterize because of problems in accumulating reliable epidemiologic data, bias, and interpretation and differing methods of expressing incidences in terms of hospital-based versus population-based data. Despite these problems, there are sufficient data to indicate that there are wide regional variations in the incidence of CHM. Estimates from North America, Australia, New Zealand, and Europe have shown the incidence of CHM to range from 0.57 to 1.1 per 1000 pregnancies, whereas studies from Southeast Asia and Japan report an incidence approaching 2.0 per 1000 pregnancies. Similarly there are data that show an increased incidence of CHM among American Indians, Eskimos, Hispanics, and African Americans as well as various Asian populations. There is no conclusive evidence that genetic traits, cultural factors, or differences in reporting account for this increase. The etiologic risk factors that have been linked to the development of CHM are advanced maternal age (>40 years) and prior molar pregnancy. Familial clusters of biparental CHM have been associated with NLRP7 gene mutations on chromosome 19q. In addition, well-documented nutritional studies have shown an inverse relationship between β-carotene and animal dietary fat intake and the incidence of CHM. In this regard, it is of interest that the documented decrease in the incidence of CHM in South Korea has been associated with a gradual Westernization of the Korean diet.
Determining the incidence rate of CCA is even more problematic because of the rarity of this condition and the difficulty in clinically distinguishing postmolar CCA from metastatic mole. In Europe and North America CCA affects approximately 1 in 40,000 pregnancies, whereas in Southeast Asia and Japan CCA rates are higher at 9.2 and 3.3 per 40,000 pregnancies, respectively. The incidence of both CHM and CCA has gradually declined over the past 30 years.
Risk factors for CCA include prior CHM, ethnicity, and advanced maternal age. CCA is 1000 times more likely to occur after CHM than after another type of pregnancy. The risk is also increased in women of Asian, American Indian, and African descent.
Pathology
Invasive mole develops when molar villi invade the myometrium. Metastases of invading molar villi occur via direct extension through venous channels. Approximately 15% of CHM will result in local invasion, and 5% will develop metastases usually to the lungs or vagina. The development of local invasion after PHM occurs in only 3% to 5% of patients, and metastatic disease is rare. The diagnosis of postmolar GTN is based on a plateau or elevation of hCG levels after molar evacuation rather than on pathology. Therefore, treatment with chemotherapy is frequently initiated without a histopathologic diagnosis other than the antecedent pregnancy.
CCA is a highly malignant disease characterized by hyperplastic and anaplastic syncytioblasts and cytotrophoblasts, absence of chorionic villi, hemorrhage, and tissue necrosis. CCA spreads by directly invading the myometrium and vascular channels, resulting in involvement at distant sites, most commonly the lungs, adnexa, vagina, brain, liver, kidney, intestines, and spleen. In contrast to invasive mole, the vast majority of cases of CCA arise following a nonmolar pregnancy.
PSTT is an extremely rare tumor that arises from the placental implantation site and consists of mononuclear intermediate trophoblasts without chorionic villi that infiltrates between myometrial fibers in sheets or chords. PSTT is associated with less vascular invasion, necrosis, and hemorrhage than CCA. Unlike CCA, PSTT has a propensity for lymphatic metastases. Immunohistochemical staining reveals the diffuse presence of cytokeratin and human placental lactogen (hPL), whereas hCG is only present focally. Because of its slow growth, paucity of symptoms, and low hCG production, early detection is the exception rather than the rule. Most PSTTs follow nonmolar gestations. Because of their relative insensitivity to chemotherapy, the mortality rate of PSTT exceeds that of CCA.
ETT is a rare variant of PSTT that develops from neoplastic transformation of chorionic-type extravillous trophoblast. Like PSTTs, ETTs can present many years after a term delivery. When diagnosed these tumors appear grossly as nodular infiltrates in the myometrium.
Pathology
Invasive mole develops when molar villi invade the myometrium. Metastases of invading molar villi occur via direct extension through venous channels. Approximately 15% of CHM will result in local invasion, and 5% will develop metastases usually to the lungs or vagina. The development of local invasion after PHM occurs in only 3% to 5% of patients, and metastatic disease is rare. The diagnosis of postmolar GTN is based on a plateau or elevation of hCG levels after molar evacuation rather than on pathology. Therefore, treatment with chemotherapy is frequently initiated without a histopathologic diagnosis other than the antecedent pregnancy.
CCA is a highly malignant disease characterized by hyperplastic and anaplastic syncytioblasts and cytotrophoblasts, absence of chorionic villi, hemorrhage, and tissue necrosis. CCA spreads by directly invading the myometrium and vascular channels, resulting in involvement at distant sites, most commonly the lungs, adnexa, vagina, brain, liver, kidney, intestines, and spleen. In contrast to invasive mole, the vast majority of cases of CCA arise following a nonmolar pregnancy.
PSTT is an extremely rare tumor that arises from the placental implantation site and consists of mononuclear intermediate trophoblasts without chorionic villi that infiltrates between myometrial fibers in sheets or chords. PSTT is associated with less vascular invasion, necrosis, and hemorrhage than CCA. Unlike CCA, PSTT has a propensity for lymphatic metastases. Immunohistochemical staining reveals the diffuse presence of cytokeratin and human placental lactogen (hPL), whereas hCG is only present focally. Because of its slow growth, paucity of symptoms, and low hCG production, early detection is the exception rather than the rule. Most PSTTs follow nonmolar gestations. Because of their relative insensitivity to chemotherapy, the mortality rate of PSTT exceeds that of CCA.
ETT is a rare variant of PSTT that develops from neoplastic transformation of chorionic-type extravillous trophoblast. Like PSTTs, ETTs can present many years after a term delivery. When diagnosed these tumors appear grossly as nodular infiltrates in the myometrium.
Clinical presentation
GTN has a varied presentation depending on the antecedent pregnancy, extent of disease, and histopathology. Postmolar GTN (usually invasive mole, occasionally CCA) most commonly presents following evacuation of CHM whose preevacuation uterine size is larger than dates and/or whose hCG level is greater than 100,000 mIU/mL. Bilateral ovarian enlargement is frequently present when the hCG level is markedly elevated. Signs suggestive of persistent disease are an enlarged uterus, irregular bleeding, and persistent bilateral enlarged ovaries. Rarely a metastatic nodule will be present in the vagina, which can bleed vigorously, particularly if biopsied. The Cancer Committee of the International Federation of Gynecologists and Obstetricians (FIGO) has established the following guidelines for the diagnosis of postmolar GTN :
- 1.
Four values or more of hCG plateaued over at least 3 weeks
- 2.
An increase in hCG of 10% or greater for 3 or more values over at least 2 weeks
- 3.
The histologic diagnosis of CCA
- 4.
Persistence of hCG 6 months after molar evacuation.
CCA, the most common histopathologic type of GTN that develops following term pregnancies or miscarriages, may present with nonspecific signs and symptoms, making the diagnosis difficult; this frequently accounts for a delay in diagnosis that often adversely affects prognosis. Therefore, GTN should be considered and an hCG test performed in any woman in the reproductive age group who presents with abnormal uterine bleeding or unexplained metastatic disease. GTN following a term or preterm gestation usually presents with uterine bleeding due to invasion of tumor, or bleeding from a metastatic site. Bleeding from uterine perforation or metastatic lesions may result in abdominal pain, hemoptysis, or melena. Patients with central nervous system metastases often exhibit evidence of increased intracranial pressure from intracerebral hemorrhage, leading to headaches, dizziness, seizures, or hemiplegia. Patients who develop extensive pulmonary metastases may present with dyspnea, cough, or chest pain. PSTTs and ETTs almost always cause irregular bleeding or amenorrhea, frequently long after the antecedent pregnancy. There are rare reported cases of nephrotic syndrome and virilizing syndrome associated with these conditions.
Workup
Once the diagnosis of GTN is suspected or established, a metastatic workup should be undertaken to determine the extent of disease. Selection of appropriate therapy for patients with GTN is based on both the anatomic staging system adopted by FIGO and the Prognostic Scoring System adopted by the World Health Organization (WHO).
The workup needed to adequately stage and score GTN should include:
- 1.
History and physical examination, baseline (pretreatment) serum quantitative hCG level, complete blood and platelet count, and tests of hepatic and renal function
- 2.
Review of all available pathologic specimens.
- 3.
Pelvic ultrasonography to detect the extent and nature of uterine involvement to help identify patients with deep uterine wall involvement who are at risk of uterine perforation, or who would benefit from a tumor-debulking hysterectomy.
- 4.
Chest radiograph to determine the presence of lung metastases. If the chest radiograph is negative a computed tomography (CT) scan of the chest may be obtained because approximately 40% of patients with negative chest radiographs have metastatic lesions on CT scan. Controversy exists as to the significance of these micrometastases with regard to the patient’s response to chemotherapy. In the absence of chest metastases, imaging of other organs may not be necessary because distant metastases are then rarely encountered.
- 5.
Magnetic resonance imaging (MRI) of the brain and abdominopelvic CT scan or MRI are indicated to identify lesions in the brain, liver, and other abdominal organs if the chest radiograph or chest CT indicates the presence of lung metastases.
- 6.
Repeat curettage after molar evacuation is not indicated unless there is excessive uterine bleeding associated with retained molar tissue. Controversy exists as to whether repeat dilation and curettage reduces the incidence of persistent postmolar GTN.
- 7.
Cerebrospinal fluid/plasma hCG ratio is sometimes used to confirm cerebral involvement.
- 8.
Additional imaging such as 18 F-fluorodeoxyglucose positron emission tomography (FDG-PET) may be useful to accurately identify sites of metabolically active disease or viable metastases and to help determine the potential for tumor resectability.
Staging and risk assessment
In 2002, the FIGO adopted a combined anatomic staging ( Box 1 ) and modified WHO risk-factor scoring system ( Table 1 ) for GTN. The FIGO stage is designated by a Roman numeral followed by the modified WHO score designated by the Arabic number separated by a colon. PSTTs and ETTs are classified separately. Treatment is based on the total score, which signifies the risk of the patient developing drug resistance. Patients whose WHO scores are less than 7 are considered to be at low risk, and patients with scores greater than 6 are considered to be at high risk of developing drug resistance. Patients with nonmetastatic disease (Stage I) and low-risk metastatic GTN (Stages II and III, score <7) can be treated initially with single-agent chemotherapy with cure rates approaching 80% to 90%. On the other hand, patients classified as having high-risk metastatic disease (Stage IV and Stages II–III with scores >6) require multiagent chemotherapy, possibly with adjuvant radiation and/or surgery, as indicated, to achieve similar cure rates. There is growing evidence that patients with low-risk GTN who have a large tumor burden reflected in hCG levels of greater than 100,000 mIU/mL and/or prognostic scores of 5 to 6 are associated with an increased risk of initial drug resistance and, therefore, should be treated initially with multiagent chemotherapy. The use of the FIGO staging/scoring system has become the accepted basis for determining the optimal initial therapy that affords the patient the best outcome with the least morbidity.
Stage I
Disease confined to the uterus
Stage II
Disease extends to the outside of the uterus, but is limited to the genital structures
Stage III
Disease extends to the lungs, with or without genital tract involvement
Stage IV
All other metastatic sites
| Prognostic Factors | Score | |||
|---|---|---|---|---|
| 0 | 1 | 2 | 4 | |
| Age (y) | <40 | >39 | — | — |
| Antecedent pregnancy | Mole | Abortion | Term | — |
| Interval (mo) a | <4 | >3, <7 | >6, <13 | >12 |
| Pretreatment serum hCG (mIU/mL) | <10 3 | 10 3 to <10 4 | 10 4 to <10 5 | >10 5 |
| Largest tumor, including uterine (cm) | — | 3 to <5 | >4 | — |
| Site of metastases | Lung | Spleen, kidney | Gastrointestinal tract | Brain, liver |
| Number of metastases | — | 1–4 | 5–8 | >8 |
| Prior failed chemotherapy | — | — | Single drug | Two drugs |
a Interval (in months) between end of antecedent pregnancy (where known) or onset of symptoms.
Treatment of low-risk GTN
Patients with nonmetastatic (Stage 1) and low-risk metastatic GTN (Stages II–III, score <7) should be treated initially with single-agent methotrexate (Mtx) or actinomycin D (actD). Several different outpatient protocols have been used and have yielded fairly comparable results ( Box 2 ). The variability in primary remission rates reflect differences in drug dosages, schedules, and routes of administration, as well as patient selection criteria. In general, the weekly intramuscular (IM) and intermittent intravenous (IV) infusion of Mtx and the biweekly single-dose actD protocols are less effective than the 5-day Mtx or actD protocols and the 8-day Mtx/folinic acid (FA) regimen. Despite these differences in primary remission rates, all patients with low-risk GTN are eventually cured, with preservation of fertility when desired.
Mtx Regimens
- 1.
Mtx: 0.4–0.5 mg/kg IV or IM daily for 5 days
- 2.
Mtx: 30–50 mg/m 2 IM weekly
- 3.
Mtx/FA:
- a.
Mtx 1 mg/kg IM or IV on days 1, 3, 5, 7
- b.
FA 10 mg PO days 2, 4, 6, 8
- a.
- 4.
High-dose Mtx/FA
- a.
Mtx 100 mg/m 2 IV bolus
- b.
Mtx 200 mg/m 2 12 h infusion
- c.
FA 15 mg every 12 h in 4 doses IM or PO beginning 24 h after starting Mtx
- a.
Actinomycin D Regimens
- 1.
actD 10–12 μg/kg IV push daily for 5 days
- 2.
actD 1.25 mg/m 2 IV push every 2 weeks
Abbreviations: actD, actinomycin D (Cosmegan); FA, folinic acid (calcium leucovorin); IM, intramuscular; IV, intravenous; Mtx, methotrexate; PO, by mouth.
At the New England Trophoblastic Disease Center (NETDC), the initial regimen consists of the sequential use of 8-day Mtx/FA and 5-day actD regimens. A recent study from NETDC found the 8-day Mtx/FA protocol to be not only a highly effective regimen but the most cost-effective as well. Most patients are treated initially with Mtx because it has fewer side effects than actD. actD should be used as first-line therapy in patients with evidence of preexisting or chemotherapy-related hepatic dysfunction, or who have had a known adverse reaction to Mtx, and as sequential therapy if the patient exhibits Mtx resistance. Unlike Mtx, which can be given IM or IV, actD must be administered through an adequate vein to reduce the risk of local tissue injury due to extravasation. The most bothersome side effects of actD are severe nausea and vomiting (which is rarely encountered with Mtx), hair loss, and a pruritic acneiform rash. Treatment is usually continued at 2- to 3-week intervals until the hCG level becomes undetectable. One or two courses of consolidation therapy are administered after gonadotropin remission (3 consecutive weekly undetectable hCG titers) is achieved in patients with Stage I GTN who require sequential or multiagent therapy, and in all patients with low-risk Stage II and III metastatic GTN. The authors usually do not administer consolidation therapy to patients with FIGO Stage I GTN (nonmetastatic disease) who respond completely to the initial single-agent regimen. In select patients with Stage I GTN and low FIGO scores (<3), it is their practice to closely monitor the hCG level after the first course of therapy and administer additional courses only if the hCG level fails to decline by 1 log within 18 days, if the hCG level plateaus or rises.
If the hCG level declines by less than 1 log, the patient is considered to be relatively resistant to that drug, and either an alternative agent is considered or the dose of the original drug is escalated, toxicity permitting. In general, patients with low-risk GTN should be treated with the least toxic effective therapy. When resistance to single-agent therapy is encountered for both Mtx and actD, combination chemotherapy with either MAC (Mtx, actD, and cyclophosphamide) or EMA/CO (etoposide, Mtx, actD, cyclophosphamide, and vincristine) is initiated. Factors found to be associated with resistance to initial Mtx chemotherapy were high pretreatment hCG levels, nonmolar antecedent pregnancy, and clinicopathologic diagnosis of CCA. The use of etoposide as in EMA/CO in GTN patients has been associated with an increased risk of secondary tumors including leukemia, breast and colon carcinoma, and melanoma. For that reason it is the authors’ policy to use MAC as the combination chemotherapy in patients with low-risk GTN who become resistant to single-agent therapy.
Regardless of the treatment protocol used, chemotherapy should be continued until the hCG level becomes undetectable. At that point consolidation therapy may be indicated, as discussed earlier. Chemotherapy is changed to an alternative singe-agent regimen if the hCG level plateaus above normal during treatment, or if toxicity precludes adequate dose or frequency of treatment. Multiagent therapy should be initiated promptly if resistance to sequential single-agent chemotherapy develops as reflected by inadequate hCG response or disease progression.
Table 2 summarizes the authors’ experience with the treatment of low-risk GTN patients at the NETDC. A total of 745 women with low-risk GTN were treated between 1965 and 2010. Complete remission was achieved with single-agent chemotherapy in 501 of 588 patients (85.2%) with Stage I GTN, 17 of 21 patients (81%) with low-risk Stage II disease, and 108 of 136 patients (79.4%) with low-risk Stage III GTN. All 118 patients (15.8%) with low-risk GTN who developed resistance to initial single-agent therapy achieved remission with combination chemotherapy with or without surgery.
| Stage | No. of Patients | No. of Remissions |
|---|---|---|
| I | 588 | 588 (100%) |
| Initial Therapy | 502 (85.4%) | |
| Sequential Mtx/actD | 459 | |
| Combination chemotherapy a | 1 | |
| Hysterectomy b (with adjunctive chemotherapy) | 33 | |
| Local resection b (with adjunctive chemotherapy) | 9 | |
| Resistant Therapy | 86 (14.6%) | |
| Combination chemotherapy a | 71 | |
| Hysterectomy/local resection b | 14 | |
| Pelvic infusion | 1 | |
| II | 21 | 21 (100%) |
| Initial Therapy | 17 (81%) | |
| Sequential Mtx/actD | 17 | |
| Resistant Therapy | 4 (19%) | |
| Combination chemotherapy a | 4 | |
| III | 136 | 136 (100%) |
| Initial Therapy | 108 (79.4%) | |
| Sequential Mtx/actD | 108 | |
| Resistant Therapy | 28 (20.6%) | |
| Combination chemotherapy a | 28 |
a Includes MAC (methotrexate, actinomycin D, cyclophosphamide), EMA (etoposide, methotrexate, actinomycin D), EMA/CO (EMA, cyclophosphamide, vincristine), EMA/EP (EMA, cisplatin).
Hysterectomy was used as initial therapy in 33 patients with Stage I GTN who no longer wished to preserve fertility. Because of the risk of occult metastatic disease, it is the authors’ practice to administer adjunctive chemotherapy with either high-dose IV Mtx/FA or bolus actD at the time of surgery. Hysterectomy should also be considered when the uterus is extensively involved with tumor to prevent or treat hemorrhage, perforation, and/or infection. Under these circumstances, hysterectomy may shorten the duration of treatment with multiagent chemotherapy in patients with resistance to single-agent therapy.
In summary, cure rates for both nonmetastatic and low-risk metastatic GTN should approach 100% with the use of single-agent Mtx and actD administered sequentially and the use of multiagent protocols when resistance to single agents develops. Approximately 10% to 30% of low-risk patients will develop resistance to the initial agent used and thus require a second drug, and 15% to 20% will require multiagent chemotherapy with or without hysterectomy to achieve remission. The patients most likely to prove resistant to single-agent therapy are those with higher risk scores.
Treatment of high-risk GTN
Patients with high-risk metastatic GTN (FIGO Stage IV and Stages II–III, score >6) should be treated initially with multiagent chemotherapy with or without adjuvant radiation therapy and/or surgery. During the 1970s and 1980s the preferred first-line multiagent regimen consisted of Mtx, actD, and cyclophosphamide or chlorambucil (MAC), which achieved cure rates in this group of patients of 50% to 71%. In the 1980s etoposide was found to be a highly effective agent for GTN when used as a single agent in patients with low-risk disease and in combination with Mtx, actD, cyclophosphamide, and vincristine (EMA/CO). EMA/CO is now the preferred primary combination chemotherapy regimen in high-risk metastatic GTN with an 80% to 90% remission rate. Tables 3 and 4 summarize the most commonly used multiagent protocols for patients with high-risk GTN and low-risk GTN who are resistant to single agents.
| Day | Drug | Dose |
|---|---|---|
| Protocol for EMA/CO | ||
| 1 | Etoposide actD Mtx | 100 mg/m 2 by infusion in 200 mL saline over 30 min 0.5 mg IVP 100 mg/m 2 IVP 200 mg/m 2 by infusion over 12 h |
| 2 | Etoposide actD Folinic acid | 100 mg/m 2 by infusion in 200 mL saline over 30 min 0.5 mg IVP 15 mg every 12 h × 4 doses IM or PO beginning 24 h after starting Mtx |
| 8 | Cyclophosphamide Vincristine | 600 mg/m 2 by infusion in saline over 30 min 1 mg/m 2 IVP |
| Protocol of EMA/EP | ||
| 1 | Etoposide actD Mtx | 100 mg/m 2 by infusion in 200 mL saline over 30 min 0.5 mg IVP 100 mg/m 2 IVP 200 mg/m 2 by infusion over 12 h |
| 2 | Etoposide actD Folinic acid | 100 mg/m 2 by infusion in 200 mL saline over 30 min 0.5 mg IVP 15 mg every 12 h × 4 doses IM or PO |
| 8 | Cisplatin Etoposide | 60 mg/m 2 IV with prehydration 100 mg/m 2 by infusion in 200 mL saline over 30 min |
| Day | Drug | Dose |
|---|---|---|
| 1 | Mtx | 1 mg/kg IM |
| actD | 0.5 mg IVP | |
| Cyclophosphamide | 3 mg/kg IVB over 45–60 min | |
| 2 | FA | 0.1 mg/kg PO a |
| actD | 0.5 mg IVP | |
| Cyclophosphamide | 3 mg/kg IVB over 45–60 min | |
| 3 | Mtx | 1 mg/kg IM |
| actD | 0.5 mg IVP | |
| Cyclophosphamide | 3 mg/kg IVB over 45–60 min | |
| 4 | FA | 0.1 mg/kg PO a |
| actD | 0.5 mg IVP | |
| Cyclophosphamide | 3 mg/kg IVB over 45–60 min | |
| 5 | Mtx | 1 mg/kg IM |
| actD | 0.5 mg IVP | |
| Cyclophosphamide | 3 mg/kg IVB over 45–60 min | |
| 6 | FA | 0.1 mg/kg PO a |
| 7 | Mtx | 1 mg/kg IM |
| 8 | FA | 0.1 mg/kg PO a |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree