Fig. 11.1
Cryoablation console and probe
Importantly, since ablation will result in tissue destruction, it is essential that a core biopsy be performed prior to treatment. Sufficient tissue should be obtained for diagnosis, assessment of estrogen and progesterone receptors, HER2/neu status, and for genomic profiling studies.
Cryoablation treatment protocols have been developed, all involving at least two freeze cycles. The most commonly used algorithm now involves a rapid freeze–thaw–rapid freeze protocol. Regardless of the technique used, it is imperative that the entire lesion is engulfed by the iceball which is easily demonstrated under ultrasound by scanning in multiple planes. The current generation of commercially available cryoablation devices utilizes liquid nitrogen circulating through a hollow, closed-end probe. The probe is placed in the center of the tumor under ultrasound guidance and positioning is confirmed by scanning in multiple planes (see Figs. 11.2, 11.3 and 11.4). The probe is insulated with the exception of the active tip so that there is no risk of cold injury to the skin at the insertion site. The tumor is approached through its long axis, but due to the length of the probe, the incision can often be placed in the lateral, inframammary, or periareolar location to optimize cosmesis. Usually no more than 10–20 cm3 of local anesthetic is required. Saline solution is used to “lift” a lesion away from the pectoralis major muscle, or to “float” a lesion away from the skin surface to avoid cold injury to the muscle or skin. The size of the lesion dictates the duration of the procedure which then determines the size of the iceball that is generated. Unlike cryoablation of a benign fibroadenoma in which the goal is treatment of the lesion while minimizing ablation of the surrounding tissue, current cancer treatment protocols require treating the lesion and a surrounding 1 cm margin of normal tissue. All current devices are able to manually increase the treatment zone intraprodecurally if the lesion is not fully engulfed (see Figs. 11.5 and 11.6).
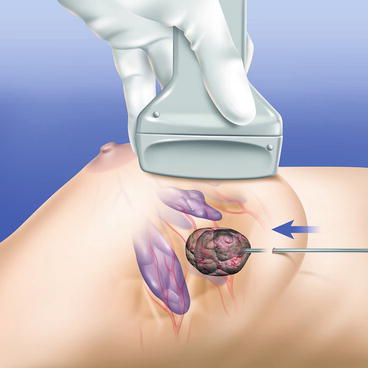
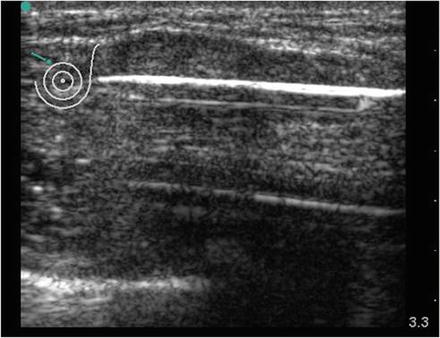
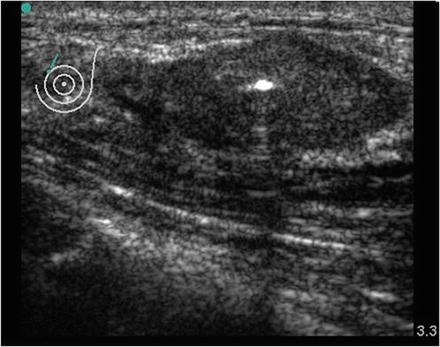
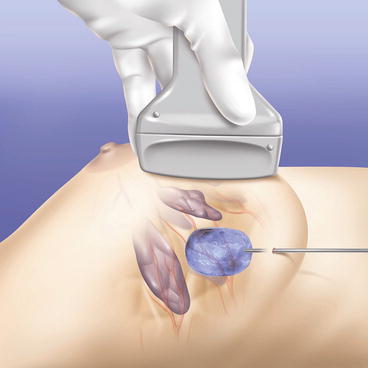
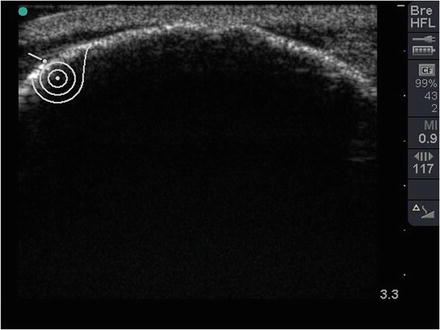
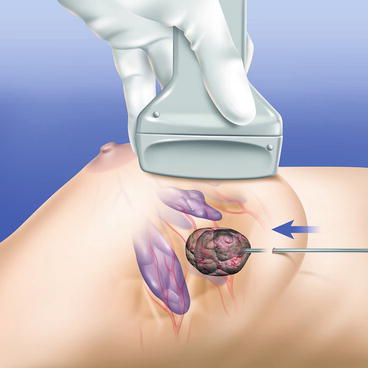
Fig. 11.2
Cryoprobe placement
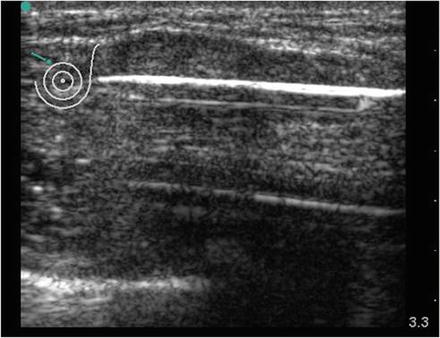
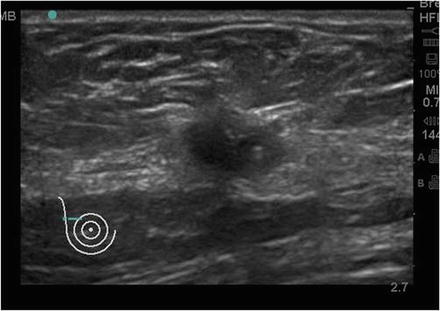
Fig. 11.3
Cryoprobe placement under ultrasound—longitudinal view
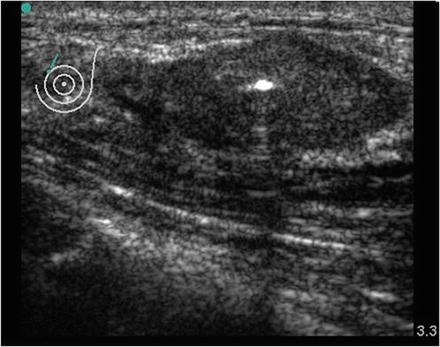
Fig. 11.4
Cryoprobe placement under ultrasound—transverse view
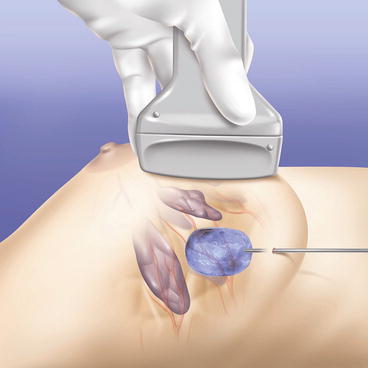
Fig. 11.5
Iceball formation
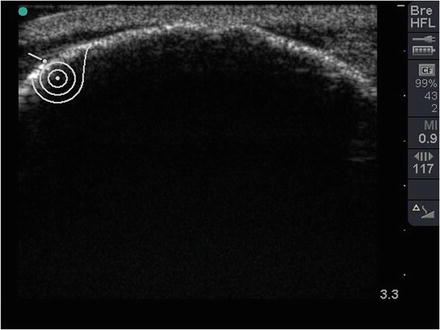
Fig. 11.6
Ultrasound image of iceball formation
After the procedure, the patient should be counseled that there may be a palpable mass. The degree of palpability and the size of the resulting mass will depend on the depth and size of the initial lesion. A modest inflammatory response and induration develops over the first few days after the procedure and some bruising is common. Most patients tolerate the procedure very well and discomfort can usually be managed using nonsteroidal anti-inflammatory agents. Within 1–2 weeks of the procedure the initial inflammation and induration begins to resolve, and if surgical excision is not performed, the patient will notice a gradual decrease in the size of the lesion. Resolution of the inflammatory response can be documented by a combination of physical examination and ultrasound (see Figs. 11.7 and 11.8). In the case of ablation for malignant disease, magnetic resonance imaging (MRI) is proving to be very useful for evaluating the initial tumor response to treatment as well as for follow up in those patients who do not undergo surgical excision. The expected MRI appearance will be that of a non-enhancing zone surrounded by a variably enhancing rim (see Figs. 11.9 and 11.10). If surgical excision is not performed, it is expected that the ablation margin will decrease in size over time. Based on experience with fibroadenoma cryoablation in which the ablated lesion is generally not removed, there has not been difficulty interpreting subsequent mammogram and ultrasound imaging studies [8].