Abstract
Prostate cancer is the second most diagnosed cancer and the fifth leading cause of cancer death among men worldwide. In the 1980s, the development and implementation of Prostate-Specific Antigen (PSA) testing for diagnosing prostate cancer led to a surge in the number of prostate cancer diagnoses. We explore the trends in recommendations and new innovations in adjunctive testing for prostate cancer screening.
1
Introduction
1.1
Background
Prostate cancer is the second most diagnosed cancer and the fifth leading cause of cancer death among men worldwide [ , ]. In 2024, the American Cancer Society estimates 288,300 men in the United States will be diagnosed with prostate cancer, resulting in 34,700 deaths. This makes it the second highest cause of cancer deaths following lung cancer [ ]. While prostate cancer can be a serious disease, most men diagnosed with prostate cancer will not die from it. Of the 1 in 8 men diagnosed, only 1 in 41 men will ultimately die of prostate cancer [ ]. The relatively indolent nature of this common disease has resulted in challenges in creating screening practices. Often, the screening, diagnosis, and treatment of prostate cancer exposes patients to harms (i.e. biopsies, infections, and patient anxiety) that do not always translate to any survival benefit, but instead may result in lasting negative side effects. However, in the instance of aggressive prostate cancer, timely screening, diagnosis, and treatment are crucial to maintain a sufficient window for cure and prevent progression to metastatic disease.
1.2
Do we have a good prostate cancer screening test?
Prior to the development of the prostate-specific antigen (PSA) blood test, there were no reliable markers for the screening and detection of early prostate cancer [ ]. Prostatic acid phosphatase (PAP) had been used to monitor prostate cancer, but could not be used in early disease as it was mainly elevated in the setting of bone metastases [ ]. The ideal screening test should be inexpensive, easy to administer, readily available, reproducible, and highly sensitive and specific. The test should be able to identify disease in a preclinical phase prior to symptom onset with limited associated morbidity [ ]. Screening should be performed in highly prevalent and treatable diseases for which earlier detection can lead to a survival benefit [ ]. The usefulness of screening tests also depend on lead-time bias and the natural history of progression of the cancer. In a slowly progressing disease like low-risk prostate cancer, it is possible to over-value a screening test due to perceived lengthened time to death that may really be due to the earlier detection in the preclinical phase.
To detect more true positive cases than false-positive cases, a good screening test must have a sensitivity exceeding 95% if the specificity is less than or equal to 95% and vice versa [ ]. High specificity is desired over sensitivity when the costs and risks associated with follow up testing are significant, such as invasive biopsy [ ]. Though the perfect screening test does not exist, PSA testing is highly sensitive but not very specific as it can be elevated in a number of benign clinical conditions. This is less than ideal and is why a positive result ultimately requires confirmatory testing by way of prostate biopsy, which is not without risks [ ]. This is not unique to prostate cancer as cervical, breast, lung, and colorectal cancer screening employ a similar methodology and often require invasive confirmatory testing with false positive rates of 5-20% reported amongst all cancer types [ , ].
1.3
Impact of PSA testing
In many ways, the advent of widespread prostate cancer screening was modelled after the Breast Cancer Detection and Awareness Program (BCDAP) by the American Cancer Society that took place between 1986 and 1989 [ ]. In 1963, The Greater New York state Health Insurance Plan project for periodic breast cancer screening with mammography and clinical breast exam had shown substantial promise in lowering breast cancer mortality [ ]. The BCDAP was a push to disseminate information about mammography’s benefits without explicit knowledge of the potential harms of universal screening [ ]. Unlike breast cancer, the first randomized trials of prostate cancer screening were not initiated until the 1990′s, and the widespread implementation of PSA testing led to a surge in the number of prostate cancer diagnoses with unclear mortality benefit [ ]. The lifetime risk of receiving a diagnosis of prostate cancer doubled from 9% in 1985 to 16% in 2009, with 89% of cancers being detected through screening [ ]. This sharp rise in incidence was predominantly due to low-risk, indolent prostate cancer that may ultimately have remained asymptomatic through a man’s lifetime, termed “pseudo-disease”. Along with false positive tests, pseudo-disease was problematic because it resulted in increased costs, overtreatment with life-altering therapies, and emotional distress.
1.4
Shifting recommendations
In 2012, the United States Preventive Services Task Force (USPSTF) issued a Grade D recommendation for prostate cancer screening in men of all ages. This was an extension of a previous 2008 Grade D recommendation in place for screening in men over 75 years of age, which was in place due to the natural long lead time of prostate cancer progression in an older population with often competing comorbid conditions [ , ]. The 2012 amendment was in response to a body of literature suggesting that PSA screening results in an overdiagnosis and over detection of “pseudo-disease” [ ]. Following this, the use of PSA screening declined precipitously, resulting in an expected decrease in the diagnosis and incidence of prostate cancer [ ]. This was alarming in the urologic oncology community due to concerns for an increased incidence of de-novo metastatic and advanced prostate cancer, termed stage migration [ ]. Shortly after this, a published study using Surveillance, Epidemiology, and End Results (SEER) data of men diagnosed with prostate cancer from 2010 to 2015 showed a rise in the incidence of metastatic disease in men 75 years and older [ ]. Although this uptick in metastatic disease at presentation was not seen in younger men aged 50 to 74 due to the slow natural history of prostate cancer progression, it was thought to result from the prior 2008 Grade D recommendation for men older than 75 that reduced PSA screening. This validated the concerns of the urologic community and, after much scrutiny, the USPSTF updated the screening recommendation to a Grade C in men aged 55 to 69 and to a grade D for men over 70 years of age in 2018 [ ]. This permitted men in the target group to choose to be screened following an individualized discussion with their clinicians about the types of available treatments, short- and long-term consequences of treatment, and surveillance.
The full impact of the shifting USPSTF recommendations has not been fully elucidated. In the past decade, several technologies and techniques have been developed to improve screening and diagnosis of prostate cancer and mitigate some of the downstream harms of a positive screen. We will highlight the evidence that informed the USPSTF recommendations and the impact of available screening adjuncts in this highly controversial disease.
1.5
Informing evidence
The controversies in prostate cancer screening are influenced by results from 2 randomized trials with conflicting results. The Prostate, Lung, Colorectal and Ovarian Cancer screening trial (PLCO; NCT00002540) was a large, randomized control trial designed and sponsored by the National Cancer Institute (NCI) to determine the effects of screening on cancer-related mortality in American men and women aged 55 to 74. The prostate arm used annual PSA screening with a threshold of 4 ng/ml to trigger biopsy referral, stopped regular screening at 6 rounds, and found no difference in mortality in trial arms [ ]. Although the trial was initially designed to evaluate the mortality impact of screening versus no screening, the high rate of screening and subsequent biopsy in the control arm resulted in a comparison of the difference in outcomes between organized versus opportunistic screening in the United States. The shifting USPSTF recommendations in 2012 reduce screening were largely based on these findings, though the trial design was somewhat flawed.
On the other hand, the European Randomized Study of Screening for Prostate Cancer (ERSPC; ISRCTN49127736) is a multicenter population-based randomized screening trial in men aged 55 to 69 based in 8 European countries with a primary outcome of prostate cancer mortality [ , ]. Participants were screened every 2 to 4 years with a PSA threshold for biopsy referral of 3 ng/ml. At 16-year follow-up, there was a 21% relative reduction in prostate cancer mortality [ ]. Additionally, within the study’s Swedish Goteborg site, results from 22 years of follow up showed organized screening resulted in a 30% decrease in prostate cancer mortality when compared to opportunistic screening and by ∼ 40% in men tested at least once [ ]. Furthermore, an increased risk of death was found in nontesting men entering the program after age 60, and in men with more than 10 years of follow up after screening termination. [ ] Although each the above trials were conducted in different clinical settings with varying designs and outcome measures, they continue to heavily inform our screening practices.
The European Randomized Study of Screening for Prostate Cancer (ERSPC) was initiated in the early 1990s to evaluate the effect of screening with prostate-specific-antigen (PSA) testing on death rates from prostate cancer. [ ] This study identified 182,000 men between 50 and 74 years in Europe and randomly assigned them to either prostate cancer screening, with a PSA every 4 years, or no screening. This study found that PSA-based screening reduced the rate of death from prostate cancer by 20%, but was associated with a high risk of overdiagnosis [ ]. PSA-based prostate cancer in conjunction with new tools (i.e., risk calculators and multiparametric MRI) make it easier to prevent overtreatment and overdiagnosis. With these advancements in technology, the European Commission updated the 2003 EU Council Screening Recommendations in September of 2022 to include some malignancies (i.e., lung, gastric, and prostate cancer) to the list of population-based quality-assured screening programs [ ].
1.6
Harms from screening, diagnosis, and treatment
Irrespective of management decisions, prostate cancer continues to have a very low mortality rate with a 5-year survival rate of 100% for localized prostate cancer [ ]. However, there is a significant reduction in life-years gained due to a loss in quality-of-life because of prostate cancer screening, diagnosis and management [ ]. Due to the slow growth rate of prostate cancer, men have approximately 15 years before experiencing benefits from prostate cancer screening [ ]. The lengthened lead time from organized screening also increases the duration of exposure to the negative effects of diagnosis and treatment. Prostate biopsy followed be radical prostatectomy, radiation therapy, or androgen deprivation therapy are the mainstays of diagnosis and treatment of prostate cancer. Postbiopsy infection due to increasing antibiotic resistance, rectal injury in radical prostatectomy, and downstream radiotherapy effects such as cystitis, proctitis, incontinence, erectile dysfunction and secondary malignancies are all potential side effects of diagnosis and treatment of prostate cancer. The incorporation of a transperineal approach in prostate biopsies has shown benefits in reducing the incidence of rectal bleeding and infection when compared to a transrectal approach [ , ]. Additionally, this approach provides more adequate sampling of the anterior portion of the prostate gland, especially when combined with advanced imaging techniques such as multiparametric MRI [ ]. Although this a feasible and sensitive approach for the diagnosis of prostate cancer, it is associated with increased pain, post procedure urinary retention, and has not been widely adopted by most urologists [ ].
1.7
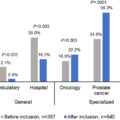
Impact of active surveillance
Many guidelines recommend active surveillance as the preferred form of management in very low and low-risk prostate cancer to minimize treatment harm [ ]. While the use of active surveillance continues to rise nationally, there is still substantial variation in its implementation based on the urologic practice setting [ ]. In men enrolled in an active surveillance program, they have greater exposure to repeated prostate biopsies, digital rectal exams, and increased anxiety and worry, which can impact quality of life [ ]. These factors continue to impact the decision-making process of undergoing prostate cancer screening in eligible men.
1.8
Screening adjuncts
1.8.1
Multiparametric magnetic resonance imaging
Multiparametric Magnetic Resonance Imaging (mp-MRI) is a relatively new imaging modality used to screen for clinically significant prostate cancer. Several studies have investigated the role of mp-MRI in increasing the rate of detection of clinically significant prostate cancer, while also decreasing the rate of detection of clinically insignificant disease, thus decreasing the chance of morbidity from prostate biopsies. One of these studies, the PROMIS trial, found that the use of mp-MRI as a screening tool could prevent 27% of biopsy-naïve men with elevated PSAs from undergoing a prostate biopsy [ ]. Their study found that the use of mp-MRI as a screening tool would lead to a 5% reduction in detection of clinically insignificant cancers [ ]. Other studies showed a similar benefit with mp-MRI, (ref PRECISION and MRI-FIRST study) making this a common part of the current screening algorithm.
1.9
Biomarkers in prostate cancer screening
Researchers have also focused on the development and validation of noninvasive biomarkers employed in screening patients for prostate cancer. To date, there are many biomarkers used in the management of prostate cancer. Many studies have looked at the efficacy of biomarkers in combination with other modalities, such as mp-MRI. Research out of University of California, San Francisco aimed to investigate the role of 4K score, SelectMDx, and ExoDx Prostate in detecting high-grade prostate cancer when combined with mp-MRI. When the biomarkers were combined with an mp-MRI, they found that it missed 0% to 1.43% of clinically significant prostate cancer and avoided 7% to 9% of unnecessary biopsies, which was lower than the biomarkers alone [ ].
2
Conclusion
In conclusion, screening for prostate cancer remains controversial. There are well-founded concerns of overtreatment in many populations of men. The incorporation of mp-MRI, refined biopsy techniques, biomarker testing, and active surveillance in men diagnosed with low-risk disease have mitigated many of these harms. As more evidence becomes available, it is possible that more personalized, risk based, organized screening recommendations incorporating adjunct technologies will be available.
CRediT authorship contribution statement
Daisy Obiora: Writing – review & editing, Writing – original draft. Oluwaseun Orikogbo: Writing – review & editing, Writing – original draft. Benjamin J. Davies: Writing – review & editing. Bruce L. Jacobs: Writing – review & editing.
Declaration of competing interest
Our research group was asked to write a review article detailing the change in prostate cancer screening practices over the past several years. We are sincerely grateful for this opportunity.
References
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree