Control and study of the first-time outbreak of angiostrongyliasis cantonensis in P.R. China
Outline
During October to November in 1997, there was an outbreak of “cryptogenetic weird disease” called “eosinophilic meningeomyeloradiculitis syndrome” in Wenzhou, Zhejiang, which was characterized by multiple paroxysmal severe body pain and pain upon contact with the skin. The disease raised general social attention. Thereby, a “specialist team” was soon organized, which was comprised of six units—— the neurology department of the first affiliated hospital of Wenzhou Medical College (WMC), the second affiliated hospital of WMC, the parasitological office of WMC, epidemic-prevention stations, and the second and the third demotic hospital of Wenzhou. Since October 1997, the team has carried out the clinical diagnosis, epidemiological study, epidemic focus investigation and sero-immunology diagnosis. Finally, they have broken through the difficulties and ascertained the causation, clinical feature and the mode of transmission of the disease. Furthermore, they found the way of prevention and countermeasure. This “weird disease” was demonstrated to be a syndrome of “larvae migrans in nervous system”, caused by “angiostrongylus cantonensis”. It is the first “angiostrongyliasis cantonensis” outbreak in mainland China. The present study will make a complete presentation of this epidemiological investigation. [1]
1. Discovery of eosinophilic meningeomyeloradiculitis syndrome
Between October 3-5th, 1997, there came the first patient who was a middleaged government officer, complaining of aching pain all over the body and weakness of limbs. At first, he felt a slight fever, headache and cenesthopathy, which appears as a common cold, so he took some Coldrex himself. In the next three days, he also suffered from paroxysmal severe pain of his right sternocostal part between the seventh and eighth costa, which became worse each day and prevented him from sleeping. When the pain struck, it was so intolerable that it felt as though something was cutting his skin. Each attack lasted for several minutes. The pain could not be relieved by kneading the skin, but it seemed that it could be relieved by pinching the muscle on the left back. With no effective resolution, the patient asked for help from Professor Rongyuan Zheng, a well-known neurology specialist in the first affiliated hospital of WMC. After a series of examinations, the results were as follows: physical examination revealed normal; chest X-ray was clear and normal; peripheral blood leukocytes increased, mainly lymphocytes, as reported by an autoanalyzer. Clinically, such severe radiculalgia was extremely rare and it is essential to make a differential diagnosis rigorously, provide close observation and
symptomatic treatment to the patient.
symptomatic treatment to the patient.
In the following 10 days, Professor Zheng had examined another two patients who had similar pain complaints. The second patient, a female, and also a middleaged government officer, had suffered from paroxysmal pain on the right side of her body for two days, which was initially diagnosed as “thoracic segment herpes zoster”. She was admitted to the dermatology ward on October 12th. Besides that the peripheral blood leukocytes increased, regular test and chest X-ray test were all normal. The third patient, a young male manager, suffered from a fever (T 38 °C), slight headache, with paroxysmal pain on the left leg and dorsum pedals, whose peripheral blood leukocytes, mainly lymphocyte, increased. Physical examination found no abnormalities. He was admitted to the infectious diseases department. After examining the patients, Professor Zheng has listed his suggestions as follows: (1) Lumbar puncture of these two patients indicated slight increase of WBC, mainly eosinophile granulocyte. (2) On the basis of this result, we had reason to doubt that there were systematic errors in the result of the peripheral blood which was counted by an autoanalyzer, so we counted it manually and found that the increase of WBC was mainly comprised of acidophic cell but not lymphocytes as reported previously. Therefore, the disease was dubbed eosinophilic meningeomyeloradiculitis syndrome. Until October 18th, the first affiliated hospital of WMC had admitted eight patients with similar clinical characteristics, which heightened Professor Zheng’s attention. In order to investigate the causation, Professor Zheng has looked up the related literature and set about an epidemiological investigation, such as interviewing patients, to determine exposure history prior to one month in order to search for the causation [1].
2. Outbreak and control of eosinophilic meningeomyeloradiculitis syndrome
Since October 19th, there have appeared more and more similar cases. The disease broke out in Wenzhou.
2.1 Investigating the first cases to rule out risk factors and to search for the causation.
The most important issue now was to determine the causation accurately, to disrupt and block the chain of infection completely, and to control the epidemic effectively. After receiving the report of the epidemic, the epidemic-prevention station set about to search for the risk factors from the early cases. They found that almost all the patients attended the same meeting held in Xueshan Hotel. By surveying the internal and external environment of Xueshan Hotel and inquiring into the exposure history of the patients, it was determined that the patients had dinner in the same hotel, which might be the suspicious transmission site. They had all eaten a new kind of special mixed cool raw food [1].
2.2 Organizing a specialist group meeting by the government to solve the problem together.
On November 7th, the Wenzhou city health administration convened specialists from five urban hospitals, epidemic-prevention station and WMC to analyze the epidemic reports and to try to ascertain the causation. The experts considered many possible diseases: viral infection in
nervous system such as occipital neuralgia, intercostal neuralgai, herpes zoster, viral cerebrospinal meningitis; spirochetal infection such as Lyme disease; parasitic infection, such as shashitsu, trichiniasis, Toxocara canis disease, distomatosis pulmonum, Gnathostomasiamense and angiostrongyliasis; neurosis, such as hysteria and somatization disorder. Finally, the conference made a group decision based on Professor Zheng’s proposal: (1) It was related to the new food. (2) It was preliminarily diagnosed to be a parasitic infection of the nervous system, and most likely to be larva migrans of angiostrongylus cantonenis. (3) Though cryptogenic, emergency measures were taken to relieve the pain of the patients by administering to them helminthicide treatment with Zental. (4) National People’s Congress would still convoke in Xueshan hotel as previously planned but the new special mixed raw food was strictly prohibited. (5) Urban hospitals should obtain and preserve patients’ serum and cerebrospinal fluid sample for future research. The suggestion of Professor Weiping Yi was also adopted: (1) According to epidemic management regulations, the information of the disease should not be revealed to TV, newspaper and radio before the epidemic had been controlled. (2) An overall and in-depth epidemiological investigation led by Wenzhou Center of Disease Control, in collaboration with clinical workers, should be carried out immediately, and the workers of parasitology should set about to investigate the focus of the epidemic. According to the advice of Baochu Lin, the chairman of Epidemic Prevention Station, a united working group comprised of clinical, epidemiological and parasitological specialists, was organized and three team leaders were appointed: Professor Zheng (neurological expert in the first affiliated hospital of WMC) for the clinical portion; Baochu Lin (Chairman of the Epidemic Prevention Station) for the epidemiological portion; and Changwang Pan (professor in the Parasititology Department of WMC) for the parasitological portion. (3) Application for emergency funds from the government should be filed for research on the disease etiology.
nervous system such as occipital neuralgia, intercostal neuralgai, herpes zoster, viral cerebrospinal meningitis; spirochetal infection such as Lyme disease; parasitic infection, such as shashitsu, trichiniasis, Toxocara canis disease, distomatosis pulmonum, Gnathostomasiamense and angiostrongyliasis; neurosis, such as hysteria and somatization disorder. Finally, the conference made a group decision based on Professor Zheng’s proposal: (1) It was related to the new food. (2) It was preliminarily diagnosed to be a parasitic infection of the nervous system, and most likely to be larva migrans of angiostrongylus cantonenis. (3) Though cryptogenic, emergency measures were taken to relieve the pain of the patients by administering to them helminthicide treatment with Zental. (4) National People’s Congress would still convoke in Xueshan hotel as previously planned but the new special mixed raw food was strictly prohibited. (5) Urban hospitals should obtain and preserve patients’ serum and cerebrospinal fluid sample for future research. The suggestion of Professor Weiping Yi was also adopted: (1) According to epidemic management regulations, the information of the disease should not be revealed to TV, newspaper and radio before the epidemic had been controlled. (2) An overall and in-depth epidemiological investigation led by Wenzhou Center of Disease Control, in collaboration with clinical workers, should be carried out immediately, and the workers of parasitology should set about to investigate the focus of the epidemic. According to the advice of Baochu Lin, the chairman of Epidemic Prevention Station, a united working group comprised of clinical, epidemiological and parasitological specialists, was organized and three team leaders were appointed: Professor Zheng (neurological expert in the first affiliated hospital of WMC) for the clinical portion; Baochu Lin (Chairman of the Epidemic Prevention Station) for the epidemiological portion; and Changwang Pan (professor in the Parasititology Department of WMC) for the parasitological portion. (3) Application for emergency funds from the government should be filed for research on the disease etiology.
During November and December, we had convened three separate conferences to discuss the progress of the research and to consider the solution. By the end of 1997, under the leadership of Professor Zheng, the three leaders had decided to report to the authority institution the program of assembling specialists in order to determine the cause of the disease [1].
2.3 Ascertaining the epidemiological situation, exposed population group and mode of transmission through epidemiological investigation [2].
In order to confirm the cause of the disease, we should first search the possible causal association and the mode of transmission; secondly, we should pay close attention to the epidemiological situation and trend; and thirdly, we should confirm the risk factors of the disease.
2.3.1 Epidemic situation
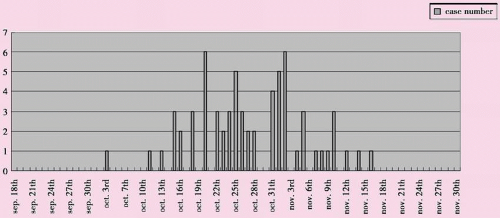
The entire epidemic disease process started on October 3rd, and ended on November 16th. During that time, there were a total of 65 cases. The peak in the epidemiology curve occurred from October 20th to November 5th, during which a total of 45 patients fell ill (69.2%), with an average of 3 to 6 cases per day (see Figure 14.1).
Retrospective case study: Firstly, environmental studies were conducted to
test whether there were any pathogenic organisms, but none were found. We then focused on case investigation by asking some of the first patients about their exposure histories, particularly diet.
test whether there were any pathogenic organisms, but none were found. We then focused on case investigation by asking some of the first patients about their exposure histories, particularly diet.
2.3.2 Retrospective cases study
The survey showed that most of the patients were government officials and fell ill after a trip, family-plan conference, carbon black meeting, alumni association meeting or social dinner. Therefore, we confirmed that people who had attended those five conferences were the exposed population and we conducted further epidemiological study on them.
Statistical results indicated that most of the patients (82.4%, or 28 out of 34) had eaten a new kind of food which was made of raw fresh snail. “Eating snail meat” may be the most significant risk factor.
2.3.3 Retrospective cohort study
To demonstrate whether the onset was related to eating the snail meat. The results revealed that: (1) During the epidemic period, 47 out of 182 people who had participated in those five meetings developed illness, with an attack rate of 25.82%. (2) Forty-seven out of 105 persons who ate the snail meat were affected; the attack rate and attributive risk both were 44.8%. Among the 77 individuals who did not eat the snail meat, no one fell ill, resulting in a significant difference between these two groups (P<0.001). (3) Among the 29 individuals who ate four pieces or more, 25 persons fell ill, with an attack rate of 86.2%. Among the 76 persons who ate less than four pieces, 22 fell ill, with the attack rate of 28.9%. By comparing the groups who ate ≥4 pieces with those who ate <4 pieces, the difference between the two groups was significant (X2 =27.53, P<0.001), RR=2.98, showing a significant dose-effect relationship. The results indicated that “eating snail meat” was a risk factor and also a possible mode of transmission. However, there was no apparent relationship between incidence and age, sex, career and residence.
2.4 Cutting off the chain of infection to control the epidemic of disease effectively.
According to the literature, “eosinophilic meningitis” or eosinophilic spinal neurodocitis once broke out over southeast Asia and
Taiwan province of China. The former was due to angiostrongyliasis cantonesis, yet the latter was due to Gnathostoma siamense. On the basis of the highly suspected diagnosis of “larva migrans in nervous system”, and the exposure history of “eating snail meat”, the causational hypothesis that infection of worm larva was caused by eating snail has been corroborated. Therefore, it is reasonable to carry out two valid intervention programs to prevent the prevailing of the disease.
Taiwan province of China. The former was due to angiostrongyliasis cantonesis, yet the latter was due to Gnathostoma siamense. On the basis of the highly suspected diagnosis of “larva migrans in nervous system”, and the exposure history of “eating snail meat”, the causational hypothesis that infection of worm larva was caused by eating snail has been corroborated. Therefore, it is reasonable to carry out two valid intervention programs to prevent the prevailing of the disease.
2.4.1 Intervention program
a. Publishing announcement: prohibiting the supply of snail meat and abolishing the snail market. b. Publicizing through media: after November 10th, announcing that “Eating snail results in weird disease” and omophagia is harmful to one’s health” through the media.
2.4.2 The epidemic had been effectively controlled
After the two intervention programs were implemeted, the epidemic had been quickly controlled (see Figure 14.1). In mid-November, the National People’s Congress was still held in Xueshan Hotel. Due to the abolition of the snail market, no one became ill among the more than 1,000 patrons. From then on, the weird disease mostly associated after dining at Xueshan Hotel disappeared. It is indicated that “eating snail meat” is closely related to the “weird disease” and the effect of the intervention is significant, thereby confirming that “eating snail meat” is the risk factor as well as the main mode of transmission for the disease.
3. Investigation of epidemic focus
Where does the snail meat come from? Where is the epidemic focus? What kind of spiral vagina is pathophorous? What is the mode of transmission? What is the infection rate and the infectiosity? Is Wenzhou a new found epidemic focus for parasitic disease? All these should be investigated to determine the truth.
3.1 Searching for the epidemic focus
The researchers worked to determine the pathogen in snails which was bought from the markets and the restaurants, but they found nothing.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree