Regardless of cancer origin or age of onset, the disease and its treatment can produce short- and long-term sequelae (ie, sexual dysfunction, infertility, or lymphedema) that adversely affect quality of life (QOL). This article outlines the primary contemporary issues or concerns that may affect QOL and offers strategies to offset or mitigate QOL disruption. These contemporary issues are identified within the domains of sexual functioning, reproductive issues, lymphedema, and the contribution of health-related QOL in influential gynecologic cancer clinical trials.
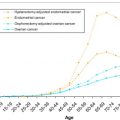
Gynecologic cancers account for approximately 11% of the newly diagnosed cancers in women in the United States and 18% in the world. The most common gynecologic malignancies occur in the uterus and endometrium (53%), ovary (25%), and cervix (14%). Cervical cancer is most prevalent in premenopausal women, during their childbearing years, whereas uterine and ovarian cancers tend to present in the perimenopausal or menopausal period. Vaginal and vulvar cancers and malignancies arising from gestation, or gestational trophoblastic neoplasms, occur to a lesser extent. Regardless of cancer origin or age of onset, the disease and its treatment can produce short- and long-term sequelae (ie, sexual dysfunction, infertility, or lymphedema) that adversely affect quality of life (QOL). This article outlines the primary contemporary issues or concerns that may affect QOL and offers strategies to offset or mitigate QOL disruption. These contemporary issues are identified within the domains of sexual functioning, reproductive issues, lymphedema, and the contribution of health-related QOL (HRQOL) in influential gynecologic cancer clinical trials.
Cancer, treatment, and sexuality
Gynecologic cancer and its treatment directly affect the sexual and reproductive organs. Surgical staging is the standard of care in treating most gynecologic malignancies and may involve the removal of the uterus and ovaries. Any cancer treatment that impairs (or removes) the ovaries can negatively affect vaginal health because of hormonal deprivation, resulting in abrupt, intense, and prolonged symptoms, including hot flashes, vaginal dryness, dyspareunia, and an overall decrease in QOL. Premenopausal and perimenopausal women diagnosed with gynecologic cancer are at high risk for ovarian failure (or surgical menopause) and sexual dysfunction, leading to emotional distress, possible disruption of social and intimate relationships, and in some cases treatment-induced infertility. Women diagnosed after menopause who have been using estrogen replacement are often advised to stop taking the hormone (especially with uterine cancer), triggering an abrupt and severe exacerbation of menopausal symptoms. Vaginal atrophy can be severe for those treated with surgical removal of the ovaries, pelvic radiation, or chemotherapy.
Other factors, such as age and relationships, can impact the sexual function of gynecologic cancer patients and survivors. Reported rates of sexual activity range from 10% to 50% in older ovarian cancer patients compared with 77% to 81% in younger patients. Many women are not sexually active because of the physical health of their partner or quality of their relationship. Misperceptions among couples, such as female cancer survivors reporting greater vaginal changes and dryness than their partner, highlight the need for relationship communication, especially for those experiencing pain.
Sexual morbidity is associated with poor psychologic adjustment and QOL in women treated for gynecologic cancer in the immediate posttreatment period and in long-term survival. Dyspareunia, vaginal dryness, and loss of desire are the most common sexual difficulties after cancer treatment. Women experiencing persistent, bothersome menopausal symptoms (ie, vaginal dryness) are at higher risk for distress and depression. Vasomotor symptoms can also be sexually disruptive by interfering with sleep and energy, and therefore require early assessment and management. Vaginal atrophy is associated with vaginal dryness, tightness, itching, burning, and pain during sexual activity or gynecologic examinations. It can also increase risk of vaginal and urinary tract infections. To alleviate these symptoms, it is important to improve lubrication, moisture, and the pH of the vagina.
Simple solutions to improve vaginal health include vaginal moisturizers and lubricants. Vaginal moisturizers are nonhormonal, over-the-counter products intended to be used several times a week consistently for overall vaginal health and comfort, regardless of sexual activity. Vaginal moisturizers hydrate the vaginal mucosa; improve the balance of intracellular fluids in the vaginal epithelium for up to 2 to 3 days (or two times per week); and restore a premenopausal vaginal pH in postmenopausal women. Women with a history of cancer often need to administer vaginal moisturizers up to three to five times per week because of the abrupt estrogen deprivation associated with cancer treatment (ie, ovarian failure or removal). For best absorption and benefit, vaginal moisturizers should be applied at bedtime and used regularly.
Vaginal lubricants, made in liquid or gel form, minimize dryness and pain during sexual activity. Water- or silicone-based lubricants are recommended, and when used properly can prevent irritation and mucosal tears, which can lead to postcoital pain or infection. Treating vaginal dryness and pain (dyspareunia) often leads to improvement in sexual response, such as better desire, subjective arousal, and ability to reach orgasm. The literature shows psychoeducational interventions promote sexual function, satisfaction, and well-being.
Surgery and Sexuality
Type and radicality of surgery is often linked to extent of sexual dysfunction. Treatment of vulvar intraepithelial neoplasia or vulvar cancer can range from local vulvar excision to radical vulvectomy, and in some cases, resection may involve the clitoral area. Older age and extensive vulvar excisions are associated with poorer sexual function and QOL. Decreased lubrication, shortened vaginal length, lack of sensation, and dyspareunia are associated with radical hysterectomy ; however, nerve-sparing approaches have led to improved QOL and reduction of bladder, sexual, and intestinal sequelae, without compromising surgical outcome. Pelvic exenteration is one of the most radical, but potentially curative, treatment strategies for advanced or recurrent gynecologic malignancy. The procedure is an en bloc resection of the pelvic organs (ie, uterus, cervix, vagina, ovaries, lower urinary tract, and rectosigmoid colon) first described by Brunschwig in 1948. This procedure requires a motivated patient, with a good support network to assist in the recovery period. Provision of information and presurgical preparation for potential changes to a woman’s body (ie, sexual function and ostomy care) are crucial for postoperative adjustment. Technologic improvements in imaging have allowed for better selection of patients (no distant metastases) most likely to benefit from this extensive surgical procedure. The best candidates are those who are younger and have recurrent cervical cancer and pathologically negative surgical margins.
Radiation and Sexuality
Studies show external-beam radiation therapy (EBRT) is associated with bowel side effects (eg, diarrhea and fecal leakage), which limit patient activities and QOL. Pelvic radiation to the vagina, especially at high doses, can cause agglutination, ulceration, or stenosis. Vaginal lubrication is often decreased because of loss of small blood vessels and direct damage to the vaginal mucosa. Vaginal depth and elasticity can be compromised by radiation therapy, adversely affecting sexual function. Inflammation to mucosal surfaces of the vagina can contribute to dyspareunia. Chronic fibrotic changes to the pelvis may worsen vaginal atrophy over time, creating chronic difficulties up to 5 years or more posttreatment, although sexual activity or vaginal dilator therapy can help.
High-dose intravaginal radiation therapy (HDIVRT) has recently shown decreased morbidity compared with EBRT. The Postoperative Radiation Therapy in Endometrial Carcinoma (PORTEC) study showed that HDIVRT was effective in vaginal disease control, with fewer toxicities and better QOL than EBRT. Other studies comparing EBRT with HDIVRT have reported excellent recurrence-free and overall survival rates. These findings suggest that early stage endometrial cancer patients can avoid the high morbidity associated with EBRT by receiving HDIVRT. The PORTEC-2 Trial did confirm, however, that HDIVRT patients experience vaginal toxicities (dryness, tightening, and shortened vagina) and dyspareunia. The paucity of data regarding the influence of these side effects on sexual function, survivorship, and QOL was noted by the authors. This area of research warrants further investigation because IVRT is gaining favor as a treatment modality.
Informational Needs and Communication
Recent survey studies have assessed cancer patients’ satisfaction and awareness of available sexual health resources and intervention strategies. Sexuality is important to cancer patients, but less than half (45%) receive information on the potential impact of cancer treatment on sexual function. Preliminary survey results demonstrate that female cancer survivors (gynecologic and breast) are not satisfied with current sexual health resources and are not communicating concerns with their medical team. In this cohort, over two-thirds (77%) expressed comfort mentioning sexual health issues with their medical team, but less than one-third (32%) discussed the topic. Sixty-five percent indicated a preference to receive written educational material followed by a discussion with their medical team. Even though 72% thought it would be helpful to speak with a sexual health expert, only 10% had done so.
Because of a lack of time and overcrowded schedules, many physicians prefer to focus on physical assessment and “combating the disease” rather than intimacy, sexuality, or other issues of QOL and survivorship. Furthermore, many healthcare providers do not have the training or resources to discuss, assess, or provide treatment plans for sexual problems. In the setting of open communication, women can often gain insight, reduce concerns, and have their experience normalized, in addition to having health promotion strategies (eg, vaginal moisturizers) suggested and reinforced. Some patients may be unaware that cancer can have latent effects or significantly influence sexuality and vaginal health, which is especially problematic in women with gynecologic cancer; as a result, sexual concerns are seldom addressed.
Female patients with cancer have indicated that treatment toxicities, prognosis, and long-term effects are among the most important topics to discuss during follow-up, and they welcome the opportunity to discuss sexual function, side effects, and symptoms. However, physicians cite a lack of time as an impediment to exploring QOL issues. Checklists or brief surveys may be an excellent method to screen for vaginal dryness, discomfort, and other survivorship concerns (ie, lymphedema). These methods are ideal because of the minimal amount of materials and personnel needed, and allow for an opportunity to elicit concerns in a time-efficient manner within the clinical setting to provide information or triage for referrals.
Assessment of Sexual Function
For evidence-based research, validated empiric measures are needed. Although many sexual function measures have been developed, the contemporary measures of sexual health have focused on the use of the Female Sexual Function Index (FSFI), both in long and short forms, and recently the Patient-Reported Outcomes Measurement Information System (PROMIS). Sexual dysfunction and symptoms in cancer survivors may differ from those experienced by women in the general population. Although the FSFI has strong psychometric qualities, it has not been validated in cancer cohorts. Recent data suggest the FSFI is a reliable, valid measure of sexual functioning for cancer populations, but scoring issues must be addressed to avoid reporting artificially low FSFI scores and estimates of female sexual dysfunction prevalence. Short versions of the FSFI have also been developed in the general population (FSFI-6 SF [Italy]) and tested in the oncology setting (FSFI CA-6) to facilitate screening for sexual dysfunction in busy clinical practices. An abridged FSFI-6 short form (SF) of the full FSFI-19 was recently validated in female outpatients reporting sexual dysfunction. However, when the psychometrics of the FSFI-6 SF was investigated in a sample of cancer survivors, a different six-item set was found to perform better. The revised items’ contents measured sexual functioning more reliably in this cohort, particularly in the domains of lubrication and satisfaction, perhaps reflecting differences in the nature of dysfunction between cancer survivors and outpatients in reproductive medicine clinics. The FSFI CA-6 SF was also examined using the Item Response Theory models to identify the one item on each of the six FSFI domains that had the most optimal measurement properties. The results are very promising, with internal consistency reliability of 0.86 and Pearson correlation of 0.97 with the full FSFI.
The recent development of the PROMIS Network ( http://www.nihpromis.org/ ) has offered a system of highly reliable, valid, flexible, precise, and responsive assessment tools to measure patient-reported health status. The objective of the PROMIS-Sexual Function tool continues this work by providing a flexible and psychometrically robust measure of sexual function within oncology. To date, development procedures have included review of the sexual function measure literature, focus group methodology, and development of a conceptual model for PROMIS sexual function measures for cancer patients. Future steps for the PROMIS sexual function measure include large-scale item testing, psychometric evaluation, validation, and translation. Brief assessment tools are essential to reduce patient burden and allow for assessment of this important domain within future clinical trials.
Reproductive issues
Cancer-related infertility can cause persistent feelings of sadness and grief lasting well into survivorship. Premature menopause or loss of reproductive function is not only associated with poorer emotional functioning but also greater risk for sexual difficulties. The relationship between infertility and long-term QOL in female cancer survivors shows that reproductive concerns are of great importance and centrally linked to psychosocial outcomes. Even women who undergo fertility-preserving surgery experience distress and reproductive concerns postoperatively over time.
Fertility-preserving surgery is an option for a select group of young gynecologic cancer patients. Cervical cancer is one of the most common cancers in women less than age 40, who are still in their childbearing years. Over the past two decades, radical trachelectomy, which allows for the preservation of the uterus, has been established as a feasible alternative in the management of cervical cancer for those desiring future fertility. An estimated 48% of women diagnosed with early stage cervical cancer in their reproductive years would meet the criteria for radical trachelectomy. The recurrence rate is less than 5% and the death rate is less than 2%, comparable with those of radical hysterectomy. Most pregnancies (∼75%) after radical trachelectomy reach the third trimester and are delivered at term (37+ weeks). These women, however, often have reproductive concerns and anxiety. A recent large series noted a 15% infertility rate in these patients with the need for reproductive assistance. Forty percent of the infertility was caused by neocervical stenosis. Other issues include dyspareunia and lymphedema. Women may not spontaneously offer information about these issues unless specifically queried because they may not consider perceived mild or intermittent issues worthy of discussion with their doctor. It may be useful and time efficient to use a checklist or symptom diaries to review potential survivorship concerns.
Young women diagnosed with endometrial cancer in their childbearing years may be eligible for conservative management with hormonal therapy. This option can be used in the treatment of complex atypical hyperplasia (precancerous condition) and low-risk endometrial cancer (ie, grade 1 histology with no myometrial invasion). Complex atypical hyperplasia of the endometrium is often treated with hysterectomy because of the high risk (29%) of progression to endometrial cancer and the 25% to 42% risk of having unidentified endometrial cancer within the specimen. Women should only be considered for conservative management after careful evaluation, including a dilatation and curettage and radiologic imaging. Patients should be counseled on the limited data with a conservative approach, risk of disease progression both during and after progestin therapy, duration of treatment, the 5% risk of ovarian metastasis, and the 10% to 29% risk of synchronous ovarian malignancy. Patients undergoing conservative nonsurgical treatment for early endometrial cancer should have regular follow-up, with endometrial sampling every 3 to 6 months. Some experts advocate definitive surgical treatment on completion of childbearing or tumor recurrence.
Ovarian cancer is less common in premenopausal women; yet, some women, including those with a diagnosis of malignant germ cell tumors, sex cord tumors, tumors of low malignant potential, or stage IA invasive ovarian cancer, may be appropriate for fertility-sparing treatment. One of the largest series on the experience of treating young women with fertility-sparing surgery for the treatment of malignant germ cell tumors showed 81% undergoing unilateral salpingo-oophorectomy and staging, with a 90% to 100% survival rate. Adult granulosa cell tumors of the ovary tend to exhibit disease unilaterally, yet 2% to 8% of these tumors may present bilaterally in the ovary. It is reasonable, but controversial, to consider removal of the other ovary and completion hysterectomy in women treated conservatively after childbearing has been completed. In women diagnosed with borderline tumors with a strong desire to preserve fertility, conservative management is not an unreasonable option if the tumor is confined to one ovary and treated with unilateral salpingo-oophorectomy plus complete surgical staging. Stage I epithelial ovarian cancer can be managed conservatively in some cases if the cancer is confined to the ovary. However, preservation of the uterus and contralateral ovary needs to be conducted in the setting of a comprehensive surgical staging procedure, with in-depth counseling about the risk of recurrence and possible adjuvant therapy. Patients treated conservatively for stage I ovarian cancer should also be closely followed with CA-125 monitoring every 3 months and transvaginal ultrasound for a minimum of 2 years. Definitive surgery may be advised after childbearing is complete.
Reproductive Options
Reproductive assistance consisting of cryopreservation of gametes (oocyte or sperm) or embryos can be a viable option for biologic offspring when there are concerns about premature menopause and infertility. Nevertheless, this option requires a functional uterus on treatment completion or may require the assistance of another individual or third party for family-building options. Techniques include egg (oocyte) donation; sperm donation; embryo donation; and in vitro fertilization with or without a gestational carrier (surrogacy). Adoption is another alternative, although the literature notes that some adoption agencies may be reluctant to consider cancer survivors as potential parents because of concerns about recurrence or late health risks after cancer treatment. Despite the risk of cancer-related infertility, many women report unmet informational needs about reproductive health either before or during treatment. Delivery of adequate information and proper preparation has been noted to reduce anxiety and distress and enhance coping and QOL.
Reproductive issues
Cancer-related infertility can cause persistent feelings of sadness and grief lasting well into survivorship. Premature menopause or loss of reproductive function is not only associated with poorer emotional functioning but also greater risk for sexual difficulties. The relationship between infertility and long-term QOL in female cancer survivors shows that reproductive concerns are of great importance and centrally linked to psychosocial outcomes. Even women who undergo fertility-preserving surgery experience distress and reproductive concerns postoperatively over time.
Fertility-preserving surgery is an option for a select group of young gynecologic cancer patients. Cervical cancer is one of the most common cancers in women less than age 40, who are still in their childbearing years. Over the past two decades, radical trachelectomy, which allows for the preservation of the uterus, has been established as a feasible alternative in the management of cervical cancer for those desiring future fertility. An estimated 48% of women diagnosed with early stage cervical cancer in their reproductive years would meet the criteria for radical trachelectomy. The recurrence rate is less than 5% and the death rate is less than 2%, comparable with those of radical hysterectomy. Most pregnancies (∼75%) after radical trachelectomy reach the third trimester and are delivered at term (37+ weeks). These women, however, often have reproductive concerns and anxiety. A recent large series noted a 15% infertility rate in these patients with the need for reproductive assistance. Forty percent of the infertility was caused by neocervical stenosis. Other issues include dyspareunia and lymphedema. Women may not spontaneously offer information about these issues unless specifically queried because they may not consider perceived mild or intermittent issues worthy of discussion with their doctor. It may be useful and time efficient to use a checklist or symptom diaries to review potential survivorship concerns.
Young women diagnosed with endometrial cancer in their childbearing years may be eligible for conservative management with hormonal therapy. This option can be used in the treatment of complex atypical hyperplasia (precancerous condition) and low-risk endometrial cancer (ie, grade 1 histology with no myometrial invasion). Complex atypical hyperplasia of the endometrium is often treated with hysterectomy because of the high risk (29%) of progression to endometrial cancer and the 25% to 42% risk of having unidentified endometrial cancer within the specimen. Women should only be considered for conservative management after careful evaluation, including a dilatation and curettage and radiologic imaging. Patients should be counseled on the limited data with a conservative approach, risk of disease progression both during and after progestin therapy, duration of treatment, the 5% risk of ovarian metastasis, and the 10% to 29% risk of synchronous ovarian malignancy. Patients undergoing conservative nonsurgical treatment for early endometrial cancer should have regular follow-up, with endometrial sampling every 3 to 6 months. Some experts advocate definitive surgical treatment on completion of childbearing or tumor recurrence.
Ovarian cancer is less common in premenopausal women; yet, some women, including those with a diagnosis of malignant germ cell tumors, sex cord tumors, tumors of low malignant potential, or stage IA invasive ovarian cancer, may be appropriate for fertility-sparing treatment. One of the largest series on the experience of treating young women with fertility-sparing surgery for the treatment of malignant germ cell tumors showed 81% undergoing unilateral salpingo-oophorectomy and staging, with a 90% to 100% survival rate. Adult granulosa cell tumors of the ovary tend to exhibit disease unilaterally, yet 2% to 8% of these tumors may present bilaterally in the ovary. It is reasonable, but controversial, to consider removal of the other ovary and completion hysterectomy in women treated conservatively after childbearing has been completed. In women diagnosed with borderline tumors with a strong desire to preserve fertility, conservative management is not an unreasonable option if the tumor is confined to one ovary and treated with unilateral salpingo-oophorectomy plus complete surgical staging. Stage I epithelial ovarian cancer can be managed conservatively in some cases if the cancer is confined to the ovary. However, preservation of the uterus and contralateral ovary needs to be conducted in the setting of a comprehensive surgical staging procedure, with in-depth counseling about the risk of recurrence and possible adjuvant therapy. Patients treated conservatively for stage I ovarian cancer should also be closely followed with CA-125 monitoring every 3 months and transvaginal ultrasound for a minimum of 2 years. Definitive surgery may be advised after childbearing is complete.
Reproductive Options
Reproductive assistance consisting of cryopreservation of gametes (oocyte or sperm) or embryos can be a viable option for biologic offspring when there are concerns about premature menopause and infertility. Nevertheless, this option requires a functional uterus on treatment completion or may require the assistance of another individual or third party for family-building options. Techniques include egg (oocyte) donation; sperm donation; embryo donation; and in vitro fertilization with or without a gestational carrier (surrogacy). Adoption is another alternative, although the literature notes that some adoption agencies may be reluctant to consider cancer survivors as potential parents because of concerns about recurrence or late health risks after cancer treatment. Despite the risk of cancer-related infertility, many women report unmet informational needs about reproductive health either before or during treatment. Delivery of adequate information and proper preparation has been noted to reduce anxiety and distress and enhance coping and QOL.
Surgical treatment and risk of lymphedema of the lower extremity
The incidence of lymphedema of the lower extremity (LLE) after treatment for gynecologic cancer, and its risk factors, are not well known. Retrospective studies indicate nodal sampling as a factor in LLE development. A recent trial reported statistically significant early and late postoperative complications in women who underwent lymphadenectomy (N = 81; P = .001) compared with those who did not. Lymphedema and lymphocysts were the main difference in noted morbidity between the groups. Shorter length of hospitalization has significantly differed between women undergoing and not undergoing lymphadenectomy (6 vs 5 days, respectively), although it is unclear if this finding translates into a quicker recovery by surgical type. Resumption of activities was a significant finding in the evaluation of other surgical studies (LAP2) and could be an important consideration in future cost and QOL analyses.
There are no prospective data empirically assessing LLE to determine the implications of lymph node factors (number of lymph nodes removed). Formal assessment in future study designs is crucial because it may be vastly underrecognized. Patient-reported outcomes (PROs) should be included to determine the potential impact of adverse effects on activities and QOL. Infection is also a contributing factor and may be a concern when conducting nodal dissection as part of the staging process. Carlson and colleagues showed that vulvar infection and inguinal wound breakdown were prevalent in women undergoing lymphadenectomy.
Lymphedema has been identified as a chronic, disruptive, and disfiguring condition, and requires long-term management. Although not life threatening, this late effect of cancer treatment is gaining more attention as patients live longer because of improved survival outcomes. Research on the psychomorbidity of upper-extremity lymphedema allows clinicians to extrapolate information about the potential difficulties faced by women with LLE. Nevertheless, there are no empiric data to fully comprehend psychosocial, functional, or QOL issues experienced by gynecologic cancer survivors coping with lymphedema. Many cancer survivors struggle with changes to their body long after treatment has been completed. Thus, the psychomorbidity of LLE on a patient’s QOL can be significant. Lymphedema can be socially embarrassing or undermine confidence in appearance or body image. A small retrospective study with vulvar cancer survivors showed LLE decreased QOL through loss of work, decreased socialization, and poor self-esteem and body image. Recurrent infections have also been highlighted as a negative compounding result of this condition. Some patients associated lymphedema with a sign of recurrence or progression of disease, causing heightened anxiety and fear. The chronic nature of this condition also serves as a constant reminder of one’s cancer history. The significance of the current research on the psychological and QOL data is directly related to the study design and methods in which these domains were measured. Many studies did not include lymphedema-specific measures when assessing emotional, social, and QOL impact of this condition. It is also difficult to fully comprehend the prevalence or extent of burden in those living with this condition without accurate incidence data. This lack of clarity stresses the importance of prospectively studying QOL variables in conjunction with lymphedema and disease-specific measurements.
New Surgical Techniques
Over the past several decades, minimally invasive surgical procedures, including laparscopically assisted and robotically assisted approaches, have been increasingly used. Minimally invasive surgical techniques can decrease patient morbidity for women undergoing surgical staging for gynecologic cancer by reducing blood loss, complications, postoperative pain, and length of hospitalization compared with laparotomy. The Gynecologic Oncology Group (GOG) conducted a national cooperative trial (LAP2) comparing laparoscopy with laparotomy for comprehensive surgical staging of uterine cancer. Laparoscopic surgical staging was found to be a feasible and safe alternative to laparotomy and demonstrated shorter hospitalization (2 days less), less pain, and fewer moderate-to-severe postoperative adverse events. In addition, patients undergoing laparoscopic surgical staging had higher QOL, better physical functioning, positive body image, less pain and interference with QOL, and a faster recovery (resumption of activities and return to work) than those receiving laparotomy over the 6-week postoperative period.
Robotically assisted surgical procedures use computer-assisted technology to provide improved dexterity and precision of instruments, with three-dimensional imaging. Compared with laparoscopy, robotic-assisted procedures are fairly new; however, the use of the da Vinci surgical system has quickly become an integral part of gynecologic oncology. Robotically assisted techniques have been used in the treatment of early stage endometrial and cervical cancers. A recent retrospective study showed that the robotically assisted hysterectomy in patients with endometrial cancer had a higher lymph node yield ( P <.0001), decreased hospital stay ( P <.0001) and estimated blood loss ( P <.001), and lower postoperative complication rate (5.9%) compared with laparotomy (29.7%; P <.0001). A recent cost comparison of robotic, laparoscopic, and open hysterectomy for treatment of endometrial cancer found laparoscopic surgery to be the least expensive, but robotic surgery was associated with a shorter recovery time. Robotically assisted hysterectomy may be preferable to laparoscopic hysterectomy, but prospective studies evaluating long-term outcomes with robotically assisted procedures are lacking.
The sentinel lymph node (SLN) concept was initially introduced for the treatment of melanoma, which revolutionized the field, and has now been examined in other diseases. Sentinel lymph node biopsy (SLNB) is a technique that provides accurate information about the status of lymph nodes without subjecting patients to comprehensive lymphadenectomy. This surgical innovation has been associated with a significant reduction in morbidity in the short (ie, infection) and the long term (ie, LLE). Studies have confirmed that objectively measured lymphedema rates after SLNB are significantly decreased compared with axillary lymph node dissection, with lymphedema rates of approximately 3% with SLNB versus approximately 20% with axillary lymph node dissection at 6 months’ follow-up, without compromise to outcome. Specifically for gynecologic cancers, surgical treatment of vulvar cancer requires inguinal lymph node dissection (unilateral or bilateral) to assess regional metastasis; as a result, the risk of postoperative complications and wound breakdown are particularly high for these women. SLNB may be a reasonable option for a select group of these patients. Recent studies have shown its value in early stage cervical cancer, and treatment algorithms have been suggested. Research with patients with endometrial cancer has suggested that the extent of nodal sampling is a factor in the development of symptomatic lymphedema, although the extent (ie, number of lymph nodes removed) is debatable, and SLNB may help solve the debate. Overall, SLNB is an innovative technique with the potential to improve QOL by minimizing morbidity; however, before implementing this as standard of care outside of the cancer center setting, larger validation studies are needed to establish safety and accuracy of this concept in gynecologic oncology.
HRQOL and PROs in clinical trials
QOL data can accurately describe a population, predict outcomes, guide clinical decisions, screen for disease or dysfunction, and inform the allocation of resources. Although potentially illuminating the meaning of the experience of illness, it also opens the appreciation of the complexity of medical issues, and reflects disease- and treatment-related symptoms, physical performance, patient satisfaction, control of disease, fears and hopelessness, expectations, social and cultural context, and personal values. Given the chronic and often incurable nature of many gynecologic malignancies, the toxicity or tolerability of a specific therapy can be as important as its efficacy, and HRQOL measurement can provide information about the impact of the disease and its treatment to aid clinicians in selecting antineoplastic and supportive care therapy. PROs are data collected directly from the patient, and the field has evolved to recognize HRQOL and symptom-specific measures and outcomes that influence trial development and care.
HRQOL in Clinical Trials
Approximately 10% of all cancer clinical trials include HRQOL as one of the main end points. Vital data that quantify the impact of treatment on HRQOL have been provided in recent upfront (first line) ovarian cancer clinical trials. To date, five completed phase III studies in the upfront treatment of ovarian cancer have included validated HRQOL outcome measures, and in every instance HRQOL was helpful in determining the best regimen.
For example, the Canadian European Intergroup trial OV.10 established the benefit of paclitaxel in treating ovarian carcinoma. One hundred fifty-two of the patients accrued in Canada completed the European Organization for Research and Treatment of Cancer Quality of Life Questionnaire C30 and a trial-specific checklist. Compliance was excellent (81%–93%), and although there was a deterioration in HRQOL domains immediately after chemotherapy (Day 8 of cycle 1), in both arms there was an improvement in global HRQOL during treatment and follow-up. Although there was greater neurologic and muscle toxicity for paclitaxel, this did not adversely affect HRQOL.
The Arbeitsgemeinschaft Gynaekologische Onkologie trial established the benefit of carboplatin. Previous data had confirmed that carboplatin and cisplatin resulted in equivalent survival. However, this study showed that the carboplatin/paclitaxel arm was associated with superior HRQOL (physical, role, and cognitive) in functioning and better outcomes in three symptom scales (carboplatin/paclitaxel associated with less nausea and vomiting [ P <.001]; less appetite loss [ P <.001]; and less fatigue [ P = .033]), with better overall HRQOL ( P = .012).
The SCOTROC trial validated the role of docetaxel where HRQOL was a primary end point. The SCOTROC study compared carboplatin/docetaxel with carboplatin/paclitaxel as first-line chemotherapy for stage IC to IV ovarian cancer and demonstrated a clear advantage for docetaxel in terms of less neurotoxicity. SCOTROC demonstrated that meaningful HRQOL differences between treatment regimens can be reported by patients using validated instruments.
However, in recurrent and resistant disease where combinations do not provide a survival advantage over single-agent palliative chemotherapy in women with relapsed ovarian cancer, the EORTC’s QLQ-30 did not detect between-arm HRQOL differences, although excessive toxicity was observed. Some of these toxicities are “paper” (laboratory) toxicities (with potential consequences), such as thrombocytopenia, and therefore not assessed by PROs.
Although some investigators remind us that it is impossible to measure a “sunbeam with a ruler,” the systematic development of validated instruments (questionnaires) has allowed important randomized clinical trials to report HRQOL. The present challenge is to translate what has been learned from clinical trials into clinical practice. Ovarian cancer has provided an opportunity to develop and validate new tools, such as the abdominal discomfort module and neurotoxicity subscale, both piloted in protocol GOG-172 (IV vs IP chemotherapy). This has contributed to lowering the dose and changing the schedule of drugs in clinical practice and in the new study (GOG-252).
Cardinal Symptoms and Concerns During the Gynecologic Cancer Disease Trajectory
Multiple factors influence HRQOL: demographic, physical, psychological, social, sexual, and spiritual. Prominent among the toxicities and symptoms that can diminish HRQOL in patients with gynecologic cancer are pain, bowel and bladder problems, emotional distress, neuropathy, alopecia, nausea and vomiting, anemia, and fatigue. In ovarian cancer, for example, there are clearly defined seasons in the disease trajectory of gynecologic tumors when the goals are cure (initial therapy); remission (for potentially platinum-sensitive disease); durable palliation (of relatively resistant disease); and the relief of suffering (palliative care). Initial presentation of ovarian cancer is associated with nonspecific symptoms, but may be more commonly associated with pelvic or abdominal pain, increased abdominal size or bloating, and difficulty eating or feeling full. Different phases of the disease have unique symptom issues, and the field is starting to evaluate subtle influences on HRQOL, such as disrupted sleep. Some data suggest that patients may be most compromised in functional well-being, and this is harder to elucidate and harder still to help.
Palliative chemotherapy: HRQoL implications
Many currently used first- and second-line chemotherapeutic agents can induce significant toxicities, and potentially diminish HRQOL. The treatment of recurrent ovarian cancer has defined the popular paradigm of continual single-agent palliative chemotherapy despite little evidence for a survival advantage for this approach and powerful, randomized controlled data that suggest premature initiation of chemotherapy is associated with poorer HRQOL. Eventually, all women develop chemotherapy-resistant tumors, and response rates are poor, with a median 2-year survival of only 20% for those with platinum-resistant ovarian cancer. Women with recurrent ovarian cancer experience an average of 12 concurrent symptoms, and these symptoms directly influence HRQOL, some related to the disease and some directly related to the treatment. The most common side effects of chemotherapy include hair loss and peripheral neuropathy, one obvious and one hidden, but both constant reminders of being a cancer patient. The most important symptoms identified in surveying 455 physicians and nurses at 17 National Comprehensive Cancer Network institutions were fatigue, pain, nausea, weight loss, fear, and HRQOL. This has been further revised to reduce the 30 items to 18 in the NFOSI-18 symptom index, assessing 51 women with advanced ovarian cancer and 10 gynecologic oncologists.
With respect to ovarian cancer, the suggestion that there may be a survival advantage for a subgroup of patients on maintenance therapy mandates that there is a better appreciation of impact of treatment on QOL. For patients with advanced disease, the worth of palliative chemotherapy can be anecdotally clear, but is supported only by a limited evidence base. Doyle and colleagues examined the value of palliative chemotherapy in 27 women with refractory and recurrent ovarian cancer, only 26% of whom had a documented tumor response and in whom overall median survival was subsequently only 11 months. Sixty-five percent of women expected that chemotherapy would make them live longer, and 42% expected that it would cure them. After two cycles of chemotherapy, HRQOL improvements were seen in global and emotional functioning using the EORTC QLQ C-30. These improvements lasted a median of 2 and 3 months, respectively. The diminishing returns of benefit with later lines of chemotherapy, however, mandate carefully weighing the merits of every intervention. More recently, large randomized ovarian cancer trials incorporating HRQOL endpoints have been reported. However, the sample size and power to detect differences is important. For example, ICON IV reported no significant difference in HRQOL despite survival differences between platinum treatment and carboplatin in combination with paclitaxel in patients with platinum-sensitive recurrent disease, reinforcing that the better control of disease often translates into better HRQOL and can compensate for treatment-related morbidity.
Chemotherapy Toxicity: Neurotoxicity
Platinum compounds, the mainstay of treatment for most gynecologic malignancies, are associated with cumulative myelosuppression neurotoxicity; nephrotoxicity; and severe noncumulative toxicities, including anemia and nausea and vomiting. Neurotoxicity, anemia, and nausea and vomiting all have well-known adverse effects on HRQOL. Paclitaxel in combination with a platinum compound is now considered the standard of care as first-line chemotherapy for advanced ovarian cancer. However, paclitaxel has a number of toxicities (eg, granulocytopenia, anemia, and thrombocytopenia) that overlap those of the platins, and the coadministration of paclitaxel and a platinum compound can potentially increase the frequency or severity of shared toxicities. Additionally, paclitaxel itself is associated with peripheral neuropathy, which can add to the disease burden. In a study of multimodal therapy, radiation therapy in combination with cisplatin alone, cisplatin plus fluorouracil and hydroxyurea, or hydroxyurea alone was assessed in women with locally advanced cervical cancer. Both cisplatin groups achieved gains in overall survival and progression-free survival; however, patients who received radiation therapy plus the three-drug regimen experienced more leukopenia and other hematologic effects of grade 3 and grade 4 toxicity than did patients in the other two groups ( P <.001).
Administration of glutamine or the antidepressant venlafaxine may be helpful in cases of paclitaxel-induced neuropathy, and amifostine may provide protection from cisplatin-induced neuropathy ; however, there is no drug to reliably prevent or cure chemotherapy-induced neuropathy. Therapeutic interventions for neurotoxicity remain controversial, with vitamin B 6 possibly reducing the efficacy of alkylator chemotherapy. Nonpharmacologic approaches to treatment of chemotherapy-induced neuropathy are based on patient education about potential neuropathic side effects; impact of these side effects on performance of daily activities (eg, buttoning clothes, walking, sensing control pedals while driving, or checking water temperature); and related safety issues.
Chemotherapy Toxicity: Intraperitoneal Therapy
Ovarian cancer tends to be chemosensitive and confines itself to the surface of the peritoneal cavity for much of its natural history. These features have made it an obvious target for intraperitoneal (IP) chemotherapy. At least eight well-conducted randomized trials in nearly 2000 women receiving primary treatment for ovarian cancer showed women were less likely to die if they received an IP component to the chemotherapy (hazard ratio [HR] = 0.79; 95% confidence interval [CI], 0.70–0.90), and the disease-free interval (HR = 0.79; 95% CI, 0.69–0.90) was also significantly prolonged. There was greater serious toxicity with regard to gastrointestinal effects, pain, and fever but less ototoxicity with the IP than intravenous route.
Wenzel and colleagues reported the first analysis of the HRQOL results of the widely cited phase III study of IV paclitaxel and cisplatin versus IV paclitaxel, IP cisplatin, and IP paclitaxel in optimal stage III epithelial ovarian cancer (GOG-172) using the FACT-O, GOG-NTX, and FACT-GOG Abdominal Discomfort measures. HRQOL was assessed before randomization (baseline); before cycle 4; and 3 to 6 weeks and 12 months posttreatment. Patients receiving IP therapy reported significantly worse HRQOL and abdominal pain before cycle 4 ( P <.0001) and worse HRQOL 3 to 6 weeks posttreatment ( P = .0035). Neurotoxicity was significantly worse both 3 to 6 weeks after completing chemotherapy ( P = .0004) and 1 year later ( P = .0018). However, there were no significant HRQOL or abdominal discomfort differences between arms 1 year posttreatment. Clinicians are aware of this trade-off and the magnitude of the impact of using this route for chemotherapy. This clearly contributes to the continued reluctance to accept IP therapy as a standard of care, but drives the next phase of studies designed to find more acceptable, less toxic therapeutic combinations.
Chemotherapy Toxicity: Combination Therapy
In the palliation of recurrent metastatic solid tumors, a popular paradigm is the sequential use of single-agent therapy to minimize toxicity. In contrast, when tumors are chemosensitive, combination platinum-based therapy is the standard in almost all gynecologic malignancies. In only two diseases is a triplet of chemotherapy the standard of care: germ cell tumors and endometrial cancer. The Cochrane meta-analysis of less chemotherapy compared with combination in advanced endometrial cancer included more than 1000 patients. Progression-free survival was significantly improved, but there was only a trend toward improved survival (HR = 0.90; 95% CI, 0.80–1.03). As expected, toxicity was generally higher with the combination chemotherapy regimens. Only one trial, GOG-177, showed a significant survival benefit from the addition of paclitaxel to combination chemotherapy, again with the expense of increased toxicity. Paclitaxel, adriamycin, and cisplatin with granulocyte colony-stimulating factor produced less grade 4 neutropenia (36% vs 50%) but more grade 3 peripheral neuropathy (12% vs 1%), for an absolute improvement in 12-month overall survival of 58% for paclitaxel, adriamycin, and cisplatin versus 50% for adriamycin and cisplatin.
In cervical cancer, HRQOL has been assessed using FACT-Cx, consisting of the Functional Assessment of Cancer Therapy (FACT-G) plus a cervix cancer-specific subscale, the Brief Pain Inventory-Short Form, and a neurotoxicity subscale. Scores were stable over time and considerably lower than the general population norms. The addition of paclitaxel to cisplatin produced a significantly higher response rate and progression-free survival, with no overall survival advantage. Despite greater myelosuppression with combination chemotherapy, there was no significant impact on the overall HRQOL score, but HRQOL and PROs have supported this as the standard of care.
Chemotherapy Toxicity: Integration of Novel Biologics
The recent attempt to add chemotherapy agents in a rational fashion in the treatment of advanced ovarian cancer (GOG-182/ICON-V) has not substantially impacted the cure rate for the disease. With the addition of gemcitabine to carboplatin and paclitaxel, there was considerable excess grade 3 and 4 toxicity. However, just as the era of increasing benefit to chemotherapy draws asymptotically to a ceiling, the hope of benefit from novel biologics has dawned, adding complex HRQOL measurement questions. The term “novel biologic” is potentially misleading in that many cytotoxics are targeted to specific biologic functions, but the term is taken to mean agents that are designed, rather than discovered, and target biologic pathways important in the development of cancer. Many affect fundamental mechanisms of cellular life in which fatigue may be a prominent side effect, and therefore a major focus of future PRO research.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree