Highlights
- •
In preclinical studies, it has been demonstrated that antihistamines may reverse macrophage immunosuppression, reactivate t-cell cytotoxicity, and enhance the immunotherapy response.
- •
By use of individual patient data from the IMvigor210 and the IMvigor211 trials, we found that the concomitant use of antihistamines with atezolizumab in the setting of second line treatment for metastatic urothelial carcinoma improves oncological and survival outcomes.
- •
This effect deserves further prospective investigation ideally with a randomized controlled trial of antihistamine versus no antihistamine use.
Abstract
Objectives
Survival outcomes of patients with metastatic urothelial carcinoma (mUC) are still suboptimal and strategies to enhance response to immune-oncology (IO) compounds are under scrutiny. In preclinical studies, it has been demonstrated that antihistamines may reverse macrophage immunosuppression, reactivate T cell cytotoxicity, and enhance the immunotherapy response. We aimed to evaluate the role of concomitant antihistamines administration on oncological outcomes among patients with mUC.
Materials and Methods
We relied on individual patient data from IMvigor210 (phase II single-arm trial on second line atezolizumab for mUC) and IMvigor211 trials (phase III randomized trial on second line atezolizumab vs chemotherapy for mUC). Among individuals treated with IO we identified patients who did and did not receive antihistamines. Multivariable Cox or competing-risks regression models were used to predict progression-free survival (PFS), overall survival (OS), and cancer-specific survival (CSS). The impact of antihistamines on the outcomes was assessed after adjusting for potential confounders.
Results
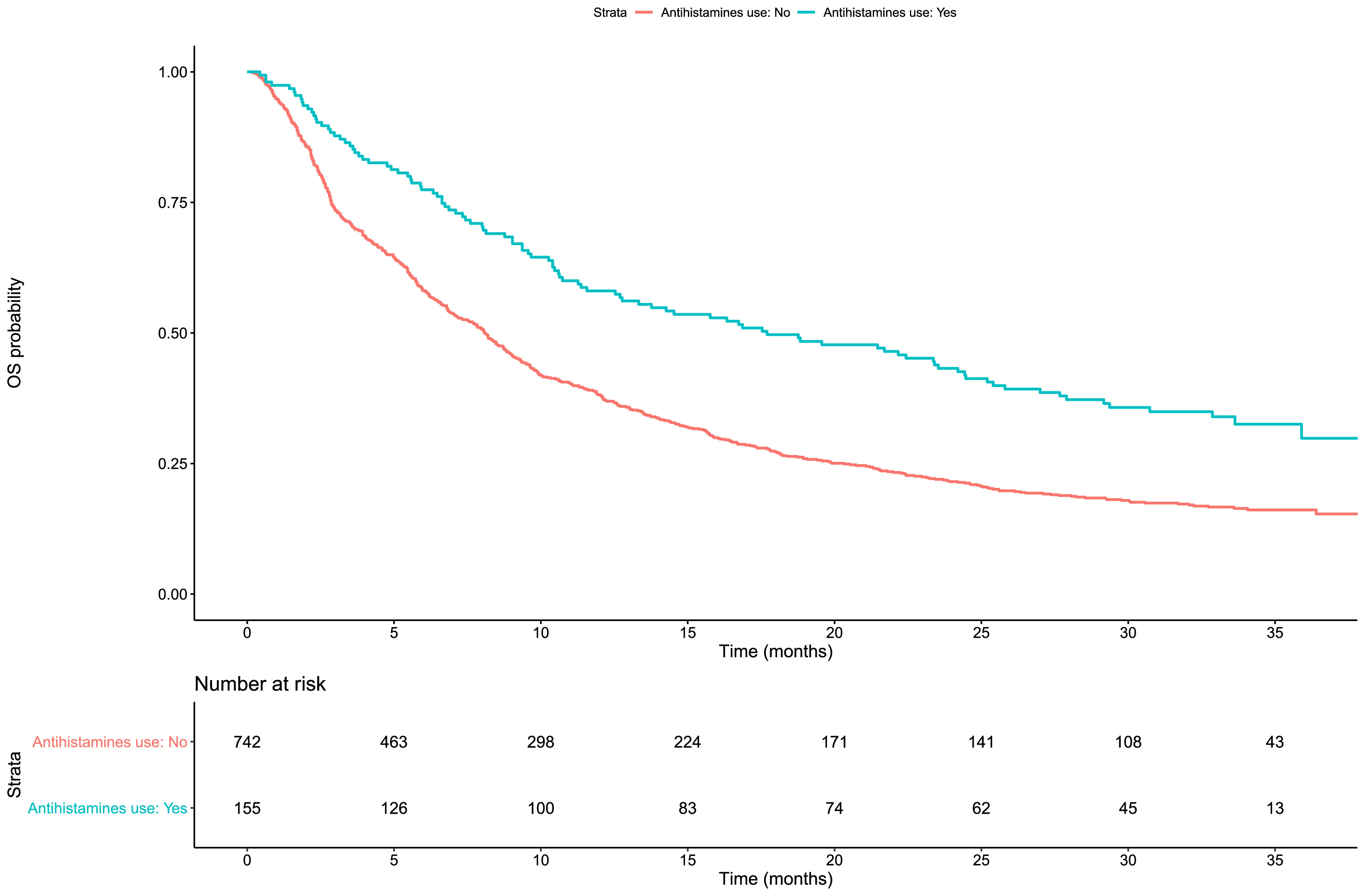
Among 896 patients with locally advanced or metastatic urothelial cancer who had progressed after first-line chemotherapy, 155 (17 %) received antihistamines during the delivery of IO. Patients receiving antihistamines had longer OS (Hazard Ratio [HR]:0.59; 95 % Confidence interval [CI]: 0.47-0.74; P < 0.001), PFS (HR:0.70; 95 %CI: 0.57-0.87; P = 0.001) and CSS [sHR:0.58; 95 %CI:0.45-0.75; P < 0.001)] relative to those who had not used antihistamine drugs. A sensitivity analysis, after the exclusion of patients who experienced adverse events and received antihistamines, yielded similar findings of prolonged CSS (sHR 0.78; 95 %CI: 0.59-0.98, P = 0.031) and OS (HR 0.71; 95 %CI: 0.52-0.94, P = 0.021).
Conclusions
Concomitant antihistamines administration was associated with improved OS, CSS, and PFS in patients receiving atezolizumab as second line treatment for mUC. Further mechanistic and clinical investigation is warranted to elucidate the role of antihistamines in IO.
1
Introduction
The prognosis of patients with locally advanced or metastatic urothelial carcinoma (mUC) is still suboptimal with a 5-year overall survival of approximately 6 % [ ]. First-line chemotherapy regimens on cisplatin can increase overall survival, but the majority of patients progress despite treatment [ , ]. Over the last decade, a paradigm shift occurred in the treatment landscape of mUC with the introduction of immuno-oncology (IO) compounds [ ]. Recent advances led to the approval of pembrolizumab in combination with enfortumab vedotin and nivolumab plus gemcitabine and cisplatin by the Food and Drugs administration (FDA) and European Medicines Agency (EMA) for patients with mUC in the first line setting [ , ]. In the second line setting, in light of the results of KEYNOTE-045, CheckMate-275 and IMvigor211 trials, pembrolizumab, nivolumab and atezolizumab, respectively, were approved by the EMA and the FDA [ , , ]. However, the response rate to these therapies is still suboptimal. A recent metanalysis on patients with mUC treated with IO reported a median OS of less than 13 months and a median progression free survival (PFS) of approximately 3 months [ ].
In this context, it is of interest to determine potential factors that might influence responses to IO. Preclinical and clinical data suggest that antihistamines may improve cancer outcomes in different settings, particularly when IO is administered, by reversing T cell dysfunction [ ]. However, the effect of antihistamines in second line IO treatment for mUC has not been investigated. With that in mind, in this study we aimed to evaluate the potential positive impact of antihistamines on oncological outcomes of patients with mUC treated with atezolizumab in a phase 2 (IMvigor210) and a phase 3 randomized control trials (IMvigor211) compared to those who did not have any antihistamines [ , ].
2
Methods
2.1
Study cohort
Data from the intention to treat population of the IMvigor210 ( ClinicalTrials.gov Identifier: NCT02108652 ) and from the atezolizumab arm of IMvigor211 (ClinicalTrials.gov Identifier: NCT02302807 ) were made available through Vivli, Inc. ( www.vivli.org ) and used according to the Hoffmann–La Roche policy.
The IMvigor210 trial was a single-arm phase II trial enrolling patients with locally advanced or metastatic urothelial carcinoma who had progressed after platinum-based chemotherapy, receiving atezolizumab 1200 mg IV every 3 weeks [ , ]. Participants have been enrolled into 2 different cohorts. Cohort 1 (n, 119) consisted of participants who were treatment-naïve and ineligible for cisplatin-based chemotherapy while cohort 2 (n, 310) included participants who had progressed during or following a platinum-based chemotherapy regimen. The IMvigor211 trial was a phase III randomized clinical trial in patients with locally advanced or metastatic urothelial carcinoma who had progressed after platinum-based chemotherapy who were randomized to receive atezolizumab (1200 mg IV every 3 weeks) or chemotherapy (docetaxel [75 mg/m2 IV every 3 weeks], paclitaxel [75 mg/m2 IV every 3 weeks], or vinflunine [320 mg/m2 IV every 3 weeks]) [ ]. Only the treatment arm of the IMvigor211 was used for the purpose of our analysis (n, 467).
2.2
Variables and outcomes definition
Overall, the variables used in this analysis were classified according to the original publications of the IMvigor210 and 211.
For our purpose, antihistamine use was defined as use of any oral histamine receptor antagonist concomitant to immunotherapy administration, either related to an acute adverse-events related to the immunotherapy or as a chronic at-home use for other clinical reasons.
Adverse events (AE) were reported by the investigators using grading based on the National Cancer Institute’s (NCI) Common Terminology Criteria for Adverse Events, version 4.0 [ , , ].
We used the variable defined as prognostic factor as used in the original trials, defined as a count of three prognostic factors, i.e., time from previous chemotherapy <3 months, ECOG performance status ≥1, and hemoglobin <10 g/dL. We categorized the variable for the purposes of our analyses into 0 and 1+.
Start of follow up was defined as the time of randomization in the IMvigor211 and the time of first atezolizumab dose in the IMvigor210. OS was defined as the time from start to follow up to death from any cause or censoring at end of follow up. Cancer specific survival (CSS) was defined as the time from start to follow-up to death from cancer or censoring at end of follow up. Time to other cause mortality was defined as the time from start to follow-up to death from other cause or censoring at end of follow up. Progression-free survival (PFS) was defined as the time from start to follow up to the time to progression (defined according to the RECIST – version 1.1 – criteria), death, or censoring at end of follow-up. The definitions of the variables and outcomes were identical in the two trials.
2.3
Statistical analysis
Patients were stratified according to antihistamine use. Medians and interquartile ranges (IQR) were used for continuous variables and numbers and proportions for categorical variables. Kruskall-Wallis and Chi‐square test were used for continuous and categorical variables, respectively, to assess differences in clinical characteristics between the 2 groups, i.e., antihistamine users versus non-users.
The Kaplan-Meier (KM) method was used to evaluate OS and PFS after stratifying patients according to antihistamine use. The log-rank test was adopted to test the equality of the survival functions. The cumulative incidence method was used to estimate cancer specific mortality and other cause mortality after accounting for the occurrence of other cause mortality, that was considered as the competing event. A multivariable Cox regression was used to predict OS and PFS; whereas a multivariable competing-risks regression was used to predict CSS after accounting for other cause mortality. A directed acyclic graph (DAG) was used to identify and explicitly represent the set of potential confounders to be adjusted in regression models ( Supplementary Fig. 1 ) [ ]. To reduce outcome heterogeneity, the effect antihistamine use on survival outcomes was adjusted for baseline age, sex, body mass index (BMI), tumor stage, and histology, count of prior treatments, type of prior chemotherapy, PD-L1 expression (IC0/1 or IC2/3), number of prognostic factors (0 or 1+), number of metastases sites, and presence of visceral metastases.
Statistical analyses were conducted on Rstudio statistical software version 3.4.3 (The R Foundation for Statistical Computing). All tests were 2‐sided, with a significance level set at 0.05.
2.3.1
Sensitivity analysis
A sensitivity analysis was conducted by excluding patients who developed an IO-related adverse event (irAE) because irAEs during IO may be associated with survival and oncological outcomes [ ] and may also influence antihistamine use because some irAEs may be treated with antihistamines [ ]. Thus, as shown in Supplementary Fig. 1 , the presence or absence of irAEs should be adjusted for because it can confound the effect of antihistamine use on survival outcomes.
In addition, to account for possible immortal time bias, we performed a landmark analysis on OS, CSS and PFS, fitted at the median follow-up of the patients included in this study.
Moreover, we performed a supplementary analysis using multivariable Cox regression analysis for OS and PFS and competing-risk analysis for CSS to assess the effect of antihistamines use in the control arm of the IMviogr211, where the IOs were not used.
Finally, we performed a supplementary analysis using Kaplan Meier and multivariable Cox regression analyses for OS, PFS and competing-risk analysis for CSS by excluding Cohort 1 of IMvigor 210, in order to repeat analyses only on those who had progressed after platinum-based chemotherapy.
3
Results
3.1
Population description
Clinical characteristics of patients according to antihistamine use are reported in Table 1 . Among the 896 individuals, 155 (17 %) used antihistamines during the trials. Baseline (i.e., at the start of follow up) age, sex, BMI, tumor stage and histology, count of prior treatments, type of prior chemotherapy, PD-L1 expression (IC0/1 or IC2/3), number of prognostic factors (0 or 1+), number of metastases sites, and presence of visceral metastases were not significantly different between those who used and those who did not use antihistamines.
| Antihistamines users | Antihistamines nonusers | p | |
|---|---|---|---|
| N° of patients | N = 155 | N = 741 | |
| Median Age (IQR) | 68 (62-75) | 67 (60-73) | >0.9 |
| Female | 64 (41 %) | 297 (40 %) | >0.9 |
| Median BMI (IQR) | 27.4 (23.6-31.5) | 26.0 (23.3-29.8) | >0.9 |
N° of prior systemic therapies:
| 21 (14 %) 62 (40 %) 72 (46 %) | 80 (11 %) 357 (48 %) 304 (41 %) | 0.3 |
Type of previous systemic therapies:
| 35 (23 %) 12 (7.7 %) 85 (54 %) 2 (1.3 %) | 179 (24 %) 51 (6.9 %) 421 (57 %) 10 (1.3 %) | 0.5 |
Histology:
| 140 (90 %) 15 (10 %) | 670 (90 %) 71 (10 %) | 0.5 |
Tumor stage:
| 49 (32 %) 48 (31 %) 42 (27 %) 15 (10 %) | 267 (36 %) 179 (24 %) 195 (26 %) 90 (14 %) | 0.18 |
N° of metastasis sites:
| 12 (7.7 %) 44 (28 %) 61 (39 %) 38 (25 %) | 50 (6.7 %) 220 (30 %) 243 (33 %) 228 (30 %) | 0.4 |
Presence of visceral metastasis
| 119 (77 %) 36 (23 %) | 571 (77 %) 170 (23 %) | >0.9 |
Liver metastasis
| 37 (24 %) 118 (76 %) | 201 (27 %) 540 (73 %) | 0.72 |
Prognostic factors:
| 66 (43 %) 89 (57 %) | 276 (37 %) 465 (63 %) | 0.7 |
PD-L1 expression
| 107 (69 %) 48 (31 %) | 539 (73 %) 202 (27 %) | 0.16 |
Overall, 645 patients died of cancer-related causes, whereas 59 died of other causes; 700 patients experienced disease progression while on treatment. The median (IQR) follow up was 17.7 (6.7-32.4) months for patients receiving antihistamines and 7.7 (2.8-18.2) months for those not receiving any antihistamines.
3.2
Antihistamines use and immunotherapy
At 2-years, the OS, CSS and PFS probabilities were, 46 %, 48 % and 23 %, respectively for patients who received antihistamines, whereas the OS, CSS and PFS probabilities were 23 %, 32 % and 13 % for those who did not receive antihistamines. The Kaplan-Meier functions for OS and PFS are displayed in Fig. 1 and 2 , respectively. Patients who received concomitant antihistamines had prolonged OS relative to those who did not receive antihistamines, i.e. median OS 17.7 (12.7-24.5) vs. 8.1 (7.1-8.9) months, respectively ( P < 0.001). Patients who received concomitant antihistamines had prolonged PFS relative to those who did not receive antihistamines, i.e., median PFS 4.9 (4.1-6.7) vs. 2.3 (2.2-2.7) months, respectively ( P < 0.001). The cumulative incidence curves for the CSS outcome are displayed in Fig. 3 . Patients who received antihistamines had prolonged CSS compared to those who did not receive antihistamines drugs, i.e., median CSS 22.8 (16.4-26.4) vs. 9.3 (7.6-10.1) months, respectively ( P < 0.001).