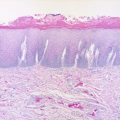
Fig. 12.1
Excision of lesion of the upper lip

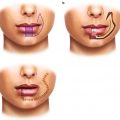
Fig. 12.2
Tension-free primary closure of the upper lip with re-approximation of the mucosa, orbicularis oris, and vermilion
12.3 Hematoma
Every effort should be placed on hemostasis. Undiagnosed or missed hematoma will lead to wound dehiscence. The lips are highly vascular with their blood supply based upon the labial arteries (branches of the facial artery). Bleeding should be controlled with either suture ligature or ligaclips. Bipolar cautery is preferred as it directly coagulates the bleeding vessels yet minimizes tissue trauma and necrosis. Extrinsic factors such as underlying coagulopathies, antiplatelet medications, and hypertension should all be addressed prior to surgery.
12.4 Infection
Infection rates for lip reconstruction secondary to cancer resection are low (range 0–17.9 %) [7, 8]. Reasons for this include proper aseptic surgical technique and the excellent vascularity associated with the lips and face. Wound infections are more common in the setting of lip defects due to animal/human bites, trauma patients, or in previously irradiated patients. Localized wound infections are treated with incision and drainage, culture, and broad-spectrum antibiotics. A small packing may be placed into the wound and allow the wound to granulate in. A more extensive infection may require tissue debridement. A common mistake is to attempt to repair the open wound defect too early, often resulting in further wound dehiscence and delayed healing.
12.5 Flap Necrosis
Flap necrosis is often a result of poor surgical technique/flap selection, wound tension, hematoma, or aggressive infection. Rotational flaps such as the Abbe/Estlander flap are dependent on the maintenance of its labial arterial pedicle. Excessive exposure of the vascular pedicle to minimize tissue bulk and increase rotational arc can result in damage or kinking of the pedicle [1, 5, 6, 9, 10]. Venous congestion and outflow obstruction manifest as an edematous, bluish-discolored flap. Arterial insufficiency manifests with poor capillary inflow, pallor, and lack of arterial Doppler signal. Treatment includes early detection, suture release, and possible flap reorientation. Early division (prior to 2–3 weeks) of a pedicled flap (especially in the irradiated patient) can also result in partial or total flap loss [9, 11].
12.6 Esthetics
Scarring can be minimized by placing the incisions along the circumoral resting skin tension lines and by keeping the incisions within the esthetic units of the lips whenever possible. For example, a shield or W-excision may be used instead of a wedge excision in order to avoid extension of the wound into the mental crease. Incisions within the nasolabial and mentolabial creases can help hide scars. Step-ladder incisions (broken lines) can help to break up scar lines as well [1, 4, 7, 8, 11]. Tension-free closure is essential to help prevent wound dehiscence and unesthetic scars.
Misalignment of the vermilion is usually due to error in technique and can be treated by re-excision and direct primary closure or local tissue rearrangement with a Z-plasty [11, 12]. This problem can be avoided with initial identification of the vermilion prior to surgical incision with either a fine marker, ink tattoo, or a fine non-resorbable suture. Tissues can become edematous during surgery, and landmarks may be less recognizable at the time of closure.
Reconstruction of lip defects close to the commissure can cause alterations in the level/height of the lip vermilion due to difference in vermilion height. Advancement of the mucosa at the time of initial reconstruction or secondary local tissue rearrangement can help to correct this deformity.
Postoperative wound care includes topical antibiotic ointments, avoidance of smoking, and mild hypoallergenic cleansing soaps to remove excessive scabbing. Skin sutures can be removed at 5–7 days to help minimize suture marks. Steri-strips can be used to help reinforce the wound during the first few weeks. Daily lip massage with vitamin E-based ointments can help to soften the scar by breaking down the deep scar tissue. Topical silicone sheeting agents can also be applied to decrease scarring. Sun care includes minimizing exposure and the use of sun blocks and hats. Scar revision surgery and resurfacing procedures should not be performed until scar maturation (usually 6–12 months postoperatively) [12]. Scar revision surgery must be performed with caution in the irradiated patient (see Figs. 12.3 and 12.4).



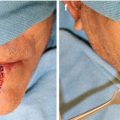
Fig. 12.3
Lip wound breakdown with healing by secondary intention resulting in widened scar

Fig. 12.4
Lip scar revision surgery requiring re-excision and re-approximation of the vermilion border
Lip fullness is considered a sign of youth and beauty in many cultures. Loss of lip fullness can occur after lip repair especially in cases requiring vermilionectomy. Mucosal advancement flaps and tongue flaps can help recreate the destroyed vermilion; however, the thinned and retracted appearance still often remains. Techniques to help correct such deformities include localized V-Y mucosal advancement flaps, tissue rearrangement, fat grafting, and the use of tissue fillers. Both synthetic filler materials (i.e., Juvederm®) and fat injections have been described as well for this purpose. Patients must be told that the tissue fillers are less predictable in the previously operated patient and that multiple injections may be required to achieve the desired results [1, 11, 12].
12.7 Microstomia
In an effort to preserve lip function and esthetics, techniques of primary closure or various rotation-advancement flaps are utilized to close larger lip defects. Although the lips are quite elastic, once defects approach greater than 25 % of the upper lip or 30–40 % of the lower lip, some element of microstomia will occur [11]. The problem of limited mouth opening and decreased oral aperture is further complicated in situations of previous reconstruction and radiation. Often, patients complain of difficulty feeding, requiring smaller bites of food to be consumed at one time and increased time required for food consumption (see Figs. 12.5, 12.6, 12.7, and 12.8). Microstomia is also challenging for edentulous patients as it becomes more difficult if not impossible to insert and remove dentures. Various prosthodontic techniques to alleviate this issue include the fabrication of a two-piece denture with each half being inserted separately and the use of fixed retained implant prostheses [13, 14].


Fig. 12.5




Microstomia secondary to extensive lower lip reconstruction using the Bernard-Fries flap (Courtesy of Dr. Robert A. Ord, University of Maryland)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree