•Incidence: 1 %
•Associated features
–Plasmablastic morphology
–Other extramedullary locations
–Plasma cell leukemia
–Increased lactate dehydrogenase
•MRI: diffuse leptomeningeal enhancement (with or without masses)
•Median survival: 3 months
Significant peripheral neuropathy at the time of diagnosis is uncommon in patients with MM [90]. The M-protein plays a pathogenetic role in the neuropathy associated with anti-myelin-associated glycoprotein (anti-MAG) in patients with IgM MGUS and in Waldenström’s macroglobulinemia. However, in other instances whether the M-protein is involved in the pathogenesis of peripheral neuropathy is unclear. In patients with IgG or IgA M-protein, the incidence of peripheral neuropathy is lower than in patients with the IgM type [96–98]. Peripheral neuropathy associated with IgG or IgA M-protein may be either demyelinating or axonal and resembles chronic inflammatory demyelinating peripheral neuropathy. Interestingly, patients with IgG- or IgA-associated peripheral neuropathies respond better than the IgM type to plasmaphoresis. Finally, peripheral neuropathy in patients with MM may be due to axonal degeneration resulting from amyloid deposition. In this case, other manifestations of systemic primary AL amyloidosis such as nephrotic syndrome, congestive heart failure, carpal tunnel syndrome, orthostatic hypotension or massive hepatomegaly may be present [10].
Peripheral neuropathy in patients with MM can be caused by neurotoxic agents. The most frequent neurotoxic drug included in the therapeutic regimens for multiple myelomas in the past decades was vincristine. Vincristine can result in paresthesias, numbness, constipation, paralytic ileus or mandibular pain leading to dose reductions or treatment discontinuation [10]. In the last 10 years, two other neurotoxic drugs, thalidomide and bortezomib, have been introduced in the treatment of MM. Thalidomide produces a sensory dose-related peripheral neuropathy in virtually all patients if there is a prolonged exposure to the drug [99, 100]. Although some degree of improvement overtime can occur, the thalidomide-associated peripheral neuropathy is usually non-reversible [100]. In clinical practice, when a patient develops numbness or paresthesia, the dose must be reduced and the symptoms carefully followed. In the authors’ experience, even with dose reductions, the peripheral neuropathy usually worsens and the drug must be subsequently discontinued. Other possible neurologic effects which can be reversible with dose reductions or drug discontinuation are distal tremor, instability and ataxia. The proteasome inhibitor bortezomib causes peripheral neuropathy and/or neuropathic pain in about 35 % of the patients [101, 102]. Contrasting with thalidomide, the bortezomib-associated neuropathy is reversible in about 70 % of the patients with the recommended dose reductions or drug discontinuation [103]. In bortezomib-associated peripheral neuropathy, the median time to reversal is about 3 months. Bortezomib causes significant orthostatic hypotension in about 10 % of the patients. It can be severe and can persist from a few days to more than 2 months after drug discontinuation. It is dose related and, when it resolves, treatment can be reinitiated at a lower bortezomib dose without recurrence. A recent review on treatment-related peripheral neuropathy in multiple myeloma has been reported [104].
Special Presentations
Plasma Cell Leukemia
PCL is defined by the presence of more than 20 % of plasma cells in peripheral blood or an absolute plasma cell count of more than 2 × 109/L [104–109]. The incidence of PCL is between 2 % and 4 % of all myelomas. There are two variants of PCL: the primary form presents in patients with no previous evidence of MM while the secondary form consists of a leukemic transformation in a previously recognized MM. About 60 % of the cases of PCL are primary (pPCL) and the remaining 40 % are secondary (sPCL).
The reason why some patients with MM present with or evolve to a picture of PCL is unknown. Primary PCL is a distinct clinicopathologic entity with presenting features, response to therapy and prognosis different from those of classic MM [104]. Furthermore, in patients with pPCL who respond to chemotherapy, the picture of PCL almost always reappears at relapse, whereas only 2 % of the patients with MM evolve to a sPCL [110]. On the other hand, there is growing evidence that sPCL is also a distinct clinical entity from pPCL with different genetics and emerging as part of the terminal phase of MM [111].
Plasma cells from patients with pPCL show a higher expression of CD20 than plasma cells from patients with MM [109]. Also, the plasma cells from PCL usually lack CD56 antigen, which is important in anchoring plasma cell to bone marrow stroma and thus preventing the circulation of myeloma cells to peripheral blood as well as their migration to extramedullary sites [109, 112]. Other immunophenotypic characteristic of the plasma cells in pPCL is the overexpression of CD27 [113]. Interestingly, it has recently been shown that CD27 overexpression can lead to the activation of nuclear factor kB (NF-kB) resulting in anti-apoptotic enhancement [113]. This can have therapeutic implications since NF-kB, which plays a major role in the survival of malignant plasma cells, is inhibited by bortezomib.
The molecular basis of PCL is poorly understood. More than 80 % of the patients show a diploid or hypodiploid DNA content while about 60 % of the patients with MM have the more favorable DNA hyperdiploidy [111, 114]. In the recent series by Tiedemann et al. [111], standard cytogenetics showed complex karyotypes with hypodiploidy or pseudodiploidy, particularly in pPCL. The frequency of IgH (14q32) translocations by FISH analysis was common in both types of PCL with 87 % and 82 % for pPCL and sPCL, respectively [111]. In two series, the incidence of t(11;14) in PCL was 33 % and 42 % [114, 115]. In a Mayo Clinic study [111] the frequency of t(11;14) by FISH or by informative karyotype in pPCL was as high as 71 %. Contrasting with the findings in sPCL where no cases of t(4;14) or t(14;16) were observed in pPCL. Of note, p53 loss due to mutation or deletion was found in 56 % of the patients with pPCL and in 83 % of the patients with sPCL [111]. IgH translocation t(11;14) is a favorable prognostic factor in MM. However, its high prevalence in a so aggressive form of plasma cell dyscrasia such as PCL suggests that this translocation when combined with high-risk cytogenetic abnormalities such as loss of p53 confers a different prognosis. Deletion of 13q by FISH is observed in 85–92 % of the patients with PCL [111]. Both Ras mutation and p16 methylation are observed in 27 % of the patients with pPCL. A high incidence of other poor cytogenetic features such as c-myc upregulation, chromosome 1p losses and 1q gains have been recently reported in patients with pPCL [116]. Although pPCL and sPCL share some genetic abnormalities, these are not identical. Thus, sPCL tend to have a lower rate of t(11;14) and a higher incidence of t(4;14) and t(14;16) and a higher incidence of p53 loss as well as a higher incidence of PTEN deletion, the latter causing Akt activation [117]. It has been suggested that PTEN loss can be involved in the transition from MM to sPCL [111, 118].
The main clinical and laboratory features, response to therapy and survival of patients with pPCL reported in the four largest series are summarized in Table 34.2. The median age ranged between 53 and 57 years, which is about 10 years less than the median age observed in the general myeloma populations. However, in a recent epidemiology study including 291 patients diagnosed between 1973 and 2004 the median age was 67 years [119]. Primary PCL has a more aggressive clinical presentation than MM with a high frequency of extramedullary involvement (liver, spleen, lymph nodes, extraosseous plasmacytomas), anemia, thrombocytopenia, hypercalcemia and renal function impairment. In contrast, the incidence of lytic bone lesion is lower than in MM. The proportion of patients with light chain myeloma ranges from 28 % to 44 % while in most myeloma series the proportion of patients with light chain (Bence Jones) myeloma is about 15 % [105, 108, 109, 111]. Finally, a high proportion of patients with pPCL have increased lactate dehydrogenase and beta2-microglobulin serum levels and a high plasma cell proliferative activity measured by labeling index or by S-phase [105, 109].
Table 34.2
Primary plasma cell leukemia: clinical and laboratory features
Feature | Noel and Kyle [105] | Dimopoulos et al. [108] | García-Sanz et al. [109] | Tiedemann et al. [111] |
|---|---|---|---|---|
No. of patients | 25 | 27 | 26 | 41 |
Median age (years) | 53 | 57 | 55 | 54 |
Sex, M/F | 15/10 | NR | 12/14 | 24/17 |
Extramedullary involvement (%) | >50 | 37 | 23 | 22 |
Lytic bone lesions (%) | 44 | NR | 48 | 35 |
Hemoglobin <10 g/dL (%) | >50 | 82 | 54 | >50 |
Platelet count <100 × 109/L (%) | >50 | 67 | 48 | >50 |
Calcium ≥11 mg/dL (%) | >50 | 44 | 48 | >50 |
Creatinine ≥2 mg/dL (%) | NR | 37 | 44 | NR |
M-protein type (%) | ||||
IgG | 12.5 (2/16) | 52 | 54 | 28 |
IgA | 25 (4/16) | 15 | 4 | 13 |
IgD | 6 (1/16) | 0 | 8 | 2 |
Light-chain | 44 (7/16) | 28 | 31 | 41 |
Non-secretory | 12.5 (2/16) | 7 | 4 | 8 |
Response to treatment (%) | 47 | 37 | 38 | NR |
Median survival (months) | 6.8 | 12 | 8 | 11.1 |
The median survival of patients with PCL is poor. In the four largest reported series, the median survival has ranged from 6.8 to 12 months [105, 108, 109, 111]. In addition, the median survival of the 291 patients included in a recently published epidemiology study was only 4 months [119]. Furthermore, the survival rate at 5 years from diagnosis is less than 10 % in all series [105, 108, 109, 111, 119] and unlike MM, in which it has been an improvement in survival in the last years, the survival of patients with PCL has not improved since 1973 [119]. These poor results on survival reflect the lack of significant efficacy of therapy in pPCL. Although a partial response can be achieved in over 50 % of the patients, the disease relapses in a few months and becomes refractory. The response rate is higher and the median survival tends to be longer with combination chemotherapy than with single alkylating agents with prednisone [108, 109]. In a series of 272 patients with pPCL who underwent ASCT reported by the European Group for Blood and Marrow Transplantation (EBMT), the median survival was only 25.7 months as compared to 63.3 months for the remaining myeloma patients. Consider that this is a Registry study and the selection bias represented by younger age and favorable response status to receive an ASCT the EBMT results are far from satisfactory [120]. Encouraging results have been reported with the association of bortezomib and dexamethasone [121–123]. It seems that induction with a bortezomib-containing regimen followed by intensification with ASCT is the best current treatment approach [123]. Given the poor prognosis of pPCL, an allogeneic transplantation with dose-reduced intensity conditioning after ASCT should be considered in patients younger than 65 years. In patients younger than 50 years, a myeloablative allogeneic transplantation after induction might also be an option.
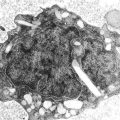
Non-Secretory Myeloma
Non-secretory MM is characterized by the absence of detectable M-protein in serum and urine by immunofixation (IFE) and it accounts for about 3 % of all the patients with MM [124–128]. The free light chain (FLC) ratio is abnormal in approximately two-thirds of the patients with apparent non-secretory myeloma. Immunoperoxidase or immunofluorescence studies on plasma cells should be performed for all patients in whom non-secretory myeloma is suspected. With these studies, a cytoplasmic M-protein is identified in about 85 % of the cases [126, 128]. These patients could be named as non-excretory myeloma. In the remaining 15 % of the cases, no M-protein is found in the cytoplasm of the plasma cells and these patients are diagnosed as “non-producer” or truly non-secretory myeloma [126, 129–132]. In non-secretory myeloma, ultrastructural study of plasma cells shows the typical features observed in patients with secretory myeloma. In contrast, in some cases of non-producer myeloma, plasma cells are highly undifferentiated even at ultrastructural study. Interestingly, in patients with non-secretory myeloma, the background immunoglobulins are even more reduced than in patients with a serum and/or urine M-protein [127].
The lack of M-protein in serum and urine of patients with non-secretory myeloma may be explained through different mechanisms (1) the inability of myeloma cells to excrete the immunoglobulin, (2) the low synthetic rate of immunoglobulin production, (3) increased immunoglobulin intracellular degradation, and/or (4) rapid extracellular degradation of abnormal immunoglobulins. They are myelomas, particularly of light chain type (Bence Jones only) in which the quantity of light chains in serum and urine is very small (i.e., 24-h light chain urine protein excretion of less than 200 mg) [128]. These cases should be named oligo-secretory or low-secretory rather than non-secretory. In fact, in the experience of the authors, non-secretory myeloma with serum and urine negative IFE is exceedingly rare. In the oligo-secretory myeloma, the light chain is of kappa type in about 75 % of the cases [124, 128]. The reason for the kappa light chain predominance is unknown. The mechanisms that could result in non-producer myeloma can be (1) a defective gene with true non-synthetic capability, (2) synthesis of an antigenically unrecognizable immunoglobulin or its fragments, or (3) very rapid intracellular degradation. Since non-secretory myeloma is very rare, for patients in whom no M-protein is found by serum and urine IFE, immunohistochemistry studies of the tumor cells are extremely important, because metastatic carcinoma, such as hypernephroma, must be excluded before the diagnosis of non-secretory myeloma is accepted.
The presenting features of non-secretory myeloma are similar to those observed in patients with an M-protein, except for the absence of renal insufficiency (Table 34.3). The majority of patients have decreased polyclonal immunoglobulins and many of them have lytic bone lesions.
Table 34.3
Presenting features in non-secretory myeloma
Feature | Azar et al. [127a] | Dreicer and Alexanian [127] | Cavo et al. [126] | Bourantas [125] |
|---|---|---|---|---|
No. of patients | 7 | 29 | 7 | 9 |
Median age (years) | 62 | 54 | 55 | 53 |
No. of patients with creatinine ≥2 mg/dL | NR | 0 | 0 | 1 |
No. of patients with high tumor mass (Durie-Salmon stage III) | NR | 2a | 6 | 8 |
No. of patients with lytic bone lesions | 6 | 29 | 5 | 9 |
Due to the lack of measurable M-protein, response to treatment and relapse cannot be monitored by changes in the M-protein levels. The evaluation of response must be based on a decrease in the proportion of bone marrow plasma cells, reduction in extramedullary plasmacytomas and no increase in the number and size of lytic bone lesions. Specific definitions for response, relapse and progression for non-secretory myeloma were developed in the EBMT criteria [133]. Also, the serum free-light chain measurement can be helpful in monitoring the response to therapy and follow-up in non-secretory myeloma as outlined by the International Myeloma Working Group response criteria [134, 135]. In the largest reported series of patients with non-secretory myeloma, the response rate to the initial therapy was 80 % [127]. In several studies, the survival of patients with non-secretory myeloma was similar to that of patients with measurable M-protein [126, 136]. However, in two series the median survival was 39 and 45 months [125, 127], slightly longer than in the general myeloma population.
Immunoglobulin D Myeloma
Immunoglobulin D myeloma (IgD myeloma) accounts for about 2 % of all myelomas [137–139]. The data on IgD myeloma come from reports of small series, two large reviews of the reported cases in the literature [140, 141] and the single-institution experience in 21 and 53 patients, respectively [142, 143].
The median age of patients with IgD myeloma is between 55 and 60 years, slightly lower than in the general myeloma population. The presenting symptoms are not different from those observed in other immunoglobulin types [143] (Table 34.4). However, the incidence of extramedullary involvement ranges between 19 % and 63 % [139, 141, 143]. In one of these studies, 7 of 53 (13 %) patients had extradural plasmacytomas at diagnosis [143]. Jancelewicz et al. [140] reported associated amyloidosis in 44 % at autopsy. However, in the Mayo Clinic experience, the frequency of associated systemic amyloidosis was 19 % [143]. The incidence of renal insufficiency is higher in IgD myeloma [140–143]. The serum electrophoretic pattern is different from that of IgG or IgA myeloma, and is similar to the one found in light chain myeloma. Thus, an M-spike on serum electrophoresis is found in only 60 % of the patients and rarely exceeds 20 g/L [143]. Moreover, almost all patients with IgD myeloma have light chain proteinuria, which exceeds 1 g/24 h in more than half of the patients [143]. These features are characteristics of light chain or Bence Jones myeloma. The frequency of lambda light chain is about 60 % [143]. Immunoglobulin D myeloma should be investigated in patients with light chain proteinuria, particularly in those with lambda type and normal renal function in whom a discrete M-spike is observed on the serum electrophoretic pattern. The main characteristics of IgD myeloma, compared with those of IgG, IgA and light chain myeloma, in the Mayo Clinic series, are shown in Table 34.5 [143]. In summary, patients with IgD myeloma usually present with a small spike or no evident band on serum electrophoresis and with heavy light chain proteinuria. About 20 % have associated systemic amyloidosis. Since these features are also characteristic of light chain myeloma, IgD myeloma can be considered as a variant of Bence Jones myeloma, the presence of the IgD M-protein and the predominance of the lambda light chain being the only distinctive features [143].
Table 34.4
IgD myeloma: clinical and laboratory features
Feature | Jancelewicz et al. [140] | Fibbe and Jansen [142] | Shimamoto et al. [141] | Bladé et al. [143] |
|---|---|---|---|---|
No. of patients | 133 | 21 | 165 | 53 |
Median age (years) | 56 | 59 | 55 | 60 |
Sex, M/F | 98/31 | 15/6 | 125/40 | 33/20 |
Extramedullary involvement (%) | >23 | NR | 27 | 19 |
Lytic bone lesions (%) | 79 | 43 | NR | 72 |
Hemoglobin <10 g/L (%) | 29 | 33 | NR | 72 |
Calcium ≥11 mg/dL (%) | 30 | 33 | 34 | 22 |
Creatinine ≥2 mg/dL (%) | 31a | 38 | 43 | 33 |
κ/λ | 115/13 | 19/2 | 133/29 | 32/20 |
Median survival (months) | 13.7 | 17 | 12 | 21 |
Table 34.5
Comparison of IgD multiple myeloma with other immunologic types (Mayo Clinic series)
Feature | IgG (n = 900) | IgA (n = 354) | Light chains only (n = 396) | IgD (n = 53) |
|---|---|---|---|---|
Median age in years | 65 | 64 | 65 | 60 |
Sex (M/F) | 564/336 | 199/155 | 238/158 | 33/20 |
Hemoglobin <10 g/dL (%) | 30 | 36 | 29 | 29 |
Creatinine ≥2 mg/dL (%) | 18 | 22 | 34 | 33 |
Calcium ≥11 mg/dL (%) | 11 | 16 | 22 | 22 |
Serum M protein (g/dL) | ||||
Median, range | 3.5 (0.2–11.8) | 3.2 (0.3–8.3) | 1.0 (0.5–3.0) | |
Urinary M protein (g/24 h) | ||||
Median, range | 0.4 (0.01–26.8) | 0.4 (0.01–35.6) | 1.8 (0.01–30.2) | 2.0 (0.08–18.6) |
Light-chain type | ||||
κ/λ ratio | 2.4/1 | 1.6/1 | 1.3/1 | 0.6/1 |
Associated amyloidosis (%) | 5 | 2 | 13 | 19 |
Median survival (months) | 31.8 | 25.1 | 23.7 | 21.4 |
The response to therapy in patients with IgD myeloma is similar to the response observed in other immunoglobulin types. The response rate to combination chemotherapy is higher than the response to a single alkylating agent. In several series, the median survival of patients with IgD myeloma has ranged from 12 to 17 months [139–142]. However, Fahey et al. [144], in a series of 15 patients, reported a median survival of 2 years. In the Mayo Clinic series, including 53 patients, the median survival was 21 months [143]. Of note, the median survival of the 26 patients diagnosed after 1980 was 31 months. Three patients from this series survived for more than 10 years and one was considered to have been cured since he died from an unrelated cancer 21 years after the diagnosis of IgD myeloma with no evidence of myeloma at autopsy [145].
IgM Myeloma
Although the presence of an IgM monoclonal protein is characteristically associated with IgM monoclonal gammopathy of undetermined significance or Waldenström’s macroglobulinemia, there are cases of MM in whom the monoclonal protein is of IgM type (IgM myeloma) [146, 147]. The IgM myeloma accounts for 0.5–1 % of all patients of MM. Apart from the recognition of the IgM protein, the clinical and laboratory features are consistent with the clinical picture of MM. Thus, the proliferating cells have a plasmacytic morphology, many patients develop anemia, renal insufficiency, hypercalcemia or lytic bone lesions. Although the experience is limited, it seems that the survival is similar to the general population with MM. The treatment approach should be the same as in other immunological types of MM [146, 147].
POEMS Syndrome (Osteosclerotic Myeloma)
POEMS syndrome is characterized by polyneuropathy, organomegaly, endocrinopathy, M-protein, and skin changes [148–152]. The most prominent features are a chronic demyelinating polyneuropathy, predominantly motor, and sclerotic skeletal lesions [150, 152]. Hepatomegaly is present in about half of the patients. Splenomegaly and lymph node enlargement, gynecomastia and testicular atrophy may occur. The more frequent skin manifestations are hyperpigmentation, hypertrichosis and angiomatous lesions on the trunk. The presence of volume overload (peripheral edema, pleural effusions, ascites) is frequent. About 50 % of the patients have papilledema. Pulmonary manifestations associated with POEMS syndrome are frequent and includes pulmonary hypertension, restrictive lung disease and respiratory muscle weakness [153]. IgA is the most frequent M-protein and almost all cases show a lambda light chain. The hemoglobin level is normal or elevated and thrombocytosis is common. The M-protein size is typically less than 30 g/L and the proportion of BMPC is less than 5 %, thus resembling the values observed in MGUS. Biopsy of the sclerotic lesion is generally necessary to confirm the diagnosis. An increase in the blood levels of vascular endothelial growth facts (VEGFs) is usually confirmatory [154]. The evolution to MM never occurs. In patients with localized sclerotic plasmacytoma radiation therapy is the treatment of choice. Patients with disseminated disease should be treated with systemic therapy similar to patients with multiple myeloma [154]. In patients younger than 70 years with no clinical contraindications, the treatment of choice is the administration of high-dose melphalan followed by autologous stem cell rescue [155]. Of note, a delayed engraftment as well as a high incidence of engraftment syndrome have been observed after ASCT in POEMS syndrome [156]. The role of anti-VEGF, immunomodulatory drugs such as lenalidomide and proteasome inhibitors has not yet been established [154].
Solitary Plasmacytoma of Bone
Solitary plasmacytoma of the bone occurs in less than 5 % of all plasma cell neoplasms and the median age at presentation is about 10 years less than in MM [157–161]. The axial skeleton is more commonly involved, thoracic vertebrae being the most usual location. Severe back pain and spinal cord compression are the more frequent presenting features. The diagnosis of solitary plasmacytoma of bone is based on the histologic evidence of a plasma cell tumor. In addition, a complete skeletal survey must show no other lesions. The bone marrow aspirate may show either no increase or less than 10 % plasma cells (Table 34.6). Approximately, 50 % of the patients have a small serum and/or urine M-protein. Therapy of the solitary lesion usually results in disappearance of the M-protein, although in some patients the M-protein may persist after tumoricidal radiation; this is associated with an increased risk of progression. There must be no evidence of anemia, hypercalcemia or renal function impairment due to the plasmacytoma. Treatment consists of radiation at a dose ranging from 40 to 50 Gy [162]. Large plasmacytomas (>5 cm) are at a higher risk of progression [163]. Overt MM develops in approximately 55 % of the patients while an additional 20 % have local recurrences or develop new focal lesions. Progression usually occurs within the first 2 years of follow-up. Thus the progression-free survival at 10 years is only 25 % [158–163]. The predictors of progression are: older age, non-vertebral location, size >5 cm, increased angiogenesis and either abnormal kappa/lambda free light chain ratio or the presence of light chains in the urine [163–165].
Table 34.6
Solitary plasmacytoma of bone
No M-protein in serum and/or urinea |
Single lytic bone lesions due to clonal plasma cell proliferation |
Bone marrow not consistent with multiple myeloma |
Normal skeletal survey and MRI (of spine and pelvis) if done |
No related organ or tissue impairment other than solitary bone lesion |
Extramedullary Plasmacytoma
Extramedullary plasmacytoma is a plasma cell tumor that originates outside the bone marrow [157, 166–168]. The usual location is the upper respiratory tract, including nasal cavity and sinuses nasopharynx and larynx. Rhinorrhea and nasal obstruction are the most frequent symptoms. Extramedullary plasmacytomas may occur in any organ including the gastrointestinal tract, brain, thyroid, breasts, testes or lymph nodes [166–168]. There is a predominante of IgA M-protein. The diagnosis is based on the finding of a plasma cell proliferation in an extramedullary site and the absence of MM (Table 34.7). Treatment consists of tumoricidal radiation (i.e., 40–50 Gy). The plasmacytoma may recur locally or metastize to regional lymph nodes in about 25 % of the patients; however, the development of MM occurs in only 15 % of the cases [166–168].
Table 34.7
Extramedullary plasmacytoma
No M-protein and/or urinea |
Extramedullary tumor due to a clonal plasma cell proliferation |
Normal bone marrow |
Normal skeletal survey |
No related organ or tissue impairment |
Macrofocal Myeloma
Dimopoulos et al. [169] reported that 10 out of their 51 patients younger than 40 years with MM fulfilled the criteria for, they coined as, “macrofocal myeloma.” This variant of MM is characterized by multiple skeletal lesions with or without soft-tissue masses, less than 10 % bone marrow plasma cells, low tumor burden and a favorable outcome. This myeloma in very young patients was previously recognized [170, 171]. Further studies are warranted to explain the macrofocal myeloma growth and to assess the real incidence of this variant at older ages and it prognosis across different ages [169].
Extramedullary Involvement with Soft-Tissue Plasmacytomas in Multiple Myeloma
In MM the plasma cells have a strong dependence on the bone marrow microenvironment. In fact, MM is considered as the model of tumor/microenvironment interaction [172, 173]. However, in some instances the plasma cells escape the bone marrow resulting in extramedullary growth. The existence of soft-tissue involvement with myeloma is well known [174]. Autopsy studies have shown extraskeletal involvement in about 70 % of the patients with MM [175, 176]. The reported incidence of extramedullary disease as either MM or extramedullary disease in MM ranges from 7 % to 18 % [143, 177–179]. In one of these studies, 20 % of the patients had plasmacytomas at more than one site at diagnosis [178]. An additional 15–20 % of the patients developed extramedullary plasmacytomas during the course of the disease [177]. In the study by Varettoni et al. [179], 45 % of the patients with extramedullary disease at diagnosis had EMP at the time of relapse. It has been suggested that patients who have undergone allogeneic transplantation with dose-reduced intensity conditioning as well as those treated with novel drugs have a higher rate of extramedullary relapse [180–185].
Extramedullary myeloma can result from local growth, hematogenous spread or can be triggered by invasive surgical procedures (Table 34.8) [186]. Local growth is the most common mechanism and consists of soft tissue masses arising from focal bone involvement, particularly vertebrae, ribs, sternum or skull. The hematogenous spread consists of (1) single or multiple large highly vascularized subcutaneous nodules with a red purple appearance, (2) multiple nodules, usually small, in the skin, liver, breast, kidney, or other organs, and (3) CNS involvement. The authors of this chapter have seen plasmacytomas arising in laparotomy scars, catheter insertions as well as extensive extramedullary local myeloma growth from bone surgery or fractures [187]. The plasma cells from EMP usually show an immature or plasmablastic morphology and patients with extramedullary disease have a more aggressive clinical behavior.
Table 34.8
Mechanisms of extramedullary involvement in multiple myeloma
Local growth Soft-tissue masses arising from focal bone involvement (vertebrae, ribs, sternum, skull) |
Hematological spread Single or multiple large subcutaneous tumors Multiple nodules (skin, liver, breast, kidney) Lymph nodes Central nervous system |
Triggered by invasive procedures performed during myeloma evolution Surgical scars Laparotomy, catheter insertions Bone surgery and/or fractures Extensive local spread |
The possible mechanisms to explain the extramedullary spread are (1) decreased expression of adhesion molecules (VLA-4, CD44, and CD56), (2) downregulation of selectin-P, (3) low expression of chemokine receptors (CCR1, CCR2, and CXCR4), (4) downregulation of tetraspanins expression, and (5) bone marrow hypoxia.
In a recent study, using a time-dependent statistical methodology, it has been shown that the presence of extramedullary involvement at any time during the course of the disease was associated with a shorter PFS and OS [179]. In other study, patients with EMP had poorer prognosis when treated with conventional chemotherapy [178]. However, in the previous two studies, patients who were given ASCT had similar outcome, irrespective of the presence or absence of extramedullary involvement, thus indicating that high-dose therapy can overcome the negative impact of EMD. Concerning the efficacy of novel drugs, others and we have reported that patients with extramedullary disease do not respond to thalidomide and also that it can be a dissociation between medullary and extramedullary response to thalidomide [188–190]. In contrast to thalidomide, several reports on the efficacy of bortezomib on EMP have been published [191, 192]. We have also seen a dissociation between medullary and extramedullary response to bortezomib [190]. There is no published experience on the efficacy of lenalidomide on extramedullary plasmacytomas.
References
1.
2.
3.
4.
5.
Lacy MQ, Donovan KA, Heimbach JK, et al. Comparison of interleukin-1 beta expression by in situ hybridization in monoclonal gammopathy of undetermined significance and multiple myeloma. Blood. 1999;93:300–5.PubMed
6.
Lust JA, Donovan KA. The role of interleukin-1 beta in the pathogenesis of multiple myeloma. Hematol Oncol Clin North Am. 1999;13:1117–25.PubMedCrossRef
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree