The Joint Commission (TJC), are unexpected occurrences involving death or serious physical or psychological injury, or the risk thereof. Tracking, reporting, and analyzing complications are critical to prevention.
Extensive edema that deprives the patient of urgently needed fluid and medications
Necrosis (localized death of tissue)
Thrombophlebitis with the subsequent danger of embolism
 PATIENT SAFETY
PATIENT SAFETYPractice. The scale was revised in 2010 to include psychometric properties. The tool was edited for pediatric use by researchers from Children’s Medical Center of Dallas; Box 10-1. The infiltration scale was removed from the Standards of Practice, and a recommended scale is now available in INS’ Policies and Procedures for Infusion Nursing. (www.ins1.org/onlinestore)
Deprive the patient of fluid and drug absorption at the rate essential for successful therapy
Limit veins available for venipuncture, complicating therapy
Predispose the patient to infection
Grade | Appearance |
0 | Asymptomatic Flushes easily |
1 | Localized swelling Flushes with difficulty Discomfort at site |
2 | Evidence of slight swelling at site or below site Redness Discomfort at site |
3 | Moderate swelling Pain at site Skin cool to touch Blanching present Diminished pulse below the site |
4 | Severe swelling Infiltration Skin cool to touch Blanching Necrosis Blistering Diminished or absent pulses Pain at site Capillary refill > 4 seconds |
Adapted from Pop, R. (2012). A pediatric peripheral intravenous infiltration assessment tool. Journal of Infusion Nursing, 35(4), 243-248. | |
 PATIENT SAFETY
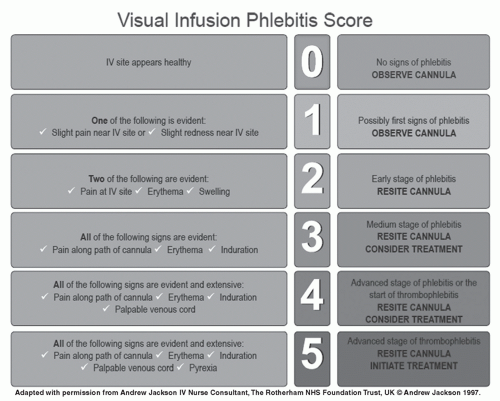
PATIENT SAFETYirritate the vein intima, causing injury and resultant phlebitis. The cannula should closely approximate the lumen of the vessel to avoid mechanical phlebitis. Proper taping and securement are essential.
Duration of the infusion
Composition of the solution
Site of the infusion
Venipuncture technique
Method used for cleansing the skin
 PATIENT SAFETY
PATIENT SAFETYduring sterilization and to maintain the stability of the solution during storage. Solutions and medications with a high pH or osmolality predispose the vein intima to irritation. The more acidic an IV admixture, the greater the risk. In addition, additives such as potassium chloride, vancomycin hydrochloride, and many antineoplastic agents can contribute to chemical phlebitis.
 PATIENT SAFETY
PATIENT SAFETYineffective filtration, placement of a large-gauge cannula in a small vessel, and failure to change tubings, dressing, injection site caps, and cannulas consistent with the INS Standards of Practice. Measures for preventing postinfusion phlebitis are provided in Box 10-4.
Ensure that a skilled clinician is performing venipuncture.
Apply antiseptic technique.
Check compatibility of solutions and medications prior to mixing/administering.
Use filters to prepare medications and solutions.
Use final filtration, as recommended, for administering medications and solutions.
Add a buffer agent to known irritants.
Rotate peripheral infusion sites.
Change the solution container per INS recommendations.
Change accessories, including caps and needleless devices, at the time of peripheral catheter change and as needed.
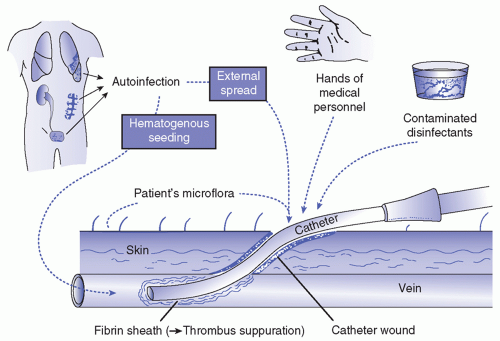
obstruct circulation but also form an excellent trap for bacteria, whether the bacteria are carried by the bloodstream from an infection in a remote part of the body or enter the body through a subcutaneous orifice. Khalidi, Kovacevich, Papke-O’Donnell, and Btaiche (2009) found that “The use of needleless positive pressure connector valves (PPVs) on venous access devices (VADs) has helped to decrease VAD occlusion rates, but catheter-related bloodstream infections (CRBSI) rates vary.”
 EVIDENCE FOR PRACTICE
EVIDENCE FOR PRACTICETABLE 10-1 APPROXIMATE RISKS OF BLOODSTREAM INFECTION ASSOCIATED WITH VARIOUS TYPES OF ACCESS DEVICES | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
 PATIENT SAFETY
PATIENT SAFETY
Refrain from using veins in the lower extremities.
Select veins with ample blood volume when infusing irritating substances.
Avoid veins in areas over joint flexion and use an arm board if the vein must be located in an area of flexion.
Anchor the catheter securely with a stabilization device to prevent motion, which may loosen the catheter.
TABLE 10-2 GENESIS OF THROMBOSIS | |||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Age younger than 1 year or older than 60 years
Granulocytopenia
Immunocompromised state
Loss of skin integrity
Distant infection that might contribute to hematogenous seeding.
Filter infusions of blood or plasma through an adequate filter to remove any particulates that could promote small emboli formation.
Do not perform venipuncture in the veins of the lower extremities. These veins are particularly susceptible to trauma that predisposes the patient to thrombophlebitis. Although superficial veins rarely seem to
be the source of emboli (INS, 2011), a thrombus may extend into the deep veins, resulting in a potentially viable clot; superficial and deep veins unite freely in the lower extremities.
Avoid applying positive pressure to relieve clot formation.
 PATIENT SAFETY
PATIENT SAFETY
Check for patency of the lumen of the catheter by kinking the infusion tubing approximately 8 inches from the catheter. Then, kink and release the tubing between the catheter and the pinched tubing. If the tubing becomes hard and meets with resistance, obstruction is evident. The catheter should be removed and the infusion reinstated.
Take special precautions with drug additives. Reconstituted drugs must be completely dissolved before being added to parenteral solutions because it is the inherent nature of red blood cells to adhere to particles, adding to the danger of clot formation.
Examine fluids to detect particulate matter.
 PATIENT SAFETY
PATIENT SAFETY PATIENT SAFETY
PATIENT SAFETYStay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree