Complementary and Alternative Medicine in Adolescents and Young Adults
Cora Collette Breuner
KEY WORDS
Acupuncture
Biofeedback
Chiropractic
Complementary alternative medicine (CAM)
Herbal therapies
Homeopathy
Massage
Yoga
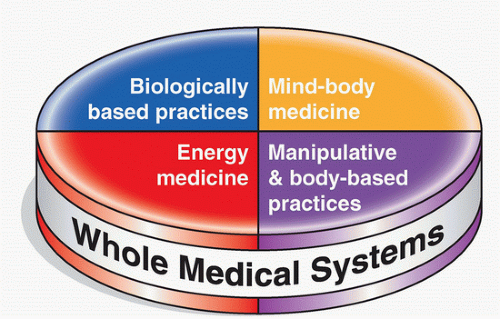
Complementary and alternative medicine (CAM) encompasses a wide spectrum of healing resources, modalities, and practices other than those fundamental to the conventional, traditional health system (Fig. 7.1).
CAM therapies may not be provided in some conventional medicine practices due to insufficient knowledge of efficacy, proof of safety, or lack of availability of specific therapies.
Those who choose CAM approaches may be searching for a way to improve their general health, to alleviate symptoms associated with chronic illnesses, or to ameliorate adverse effects of conventional treatments.1
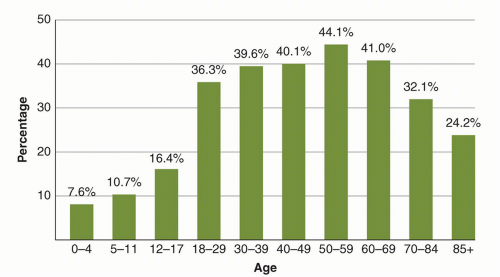
Data suggest that 16.4% of 12- to 17-year-olds and 36.3% of 18- to 29-year-olds are using some form of CAM (Fig. 7.2). CAM was more likely to be used by children and adolescents if parents used CAM and if they were between 12 and 17 years of age. For all children 0 to 17 years of age, CAM use was noted more among White children (12.8%) compared to Hispanic (7.9%) and Black youth (5.9%), in those whose parents reported higher education levels (14.7% >high school), in children with six or more health conditions (23.8%), and, importantly, in children whose families delayed conventional care because of cost (16.9%).2
CAM therapies most frequently used by adolescents and young adults (AYAs) include herbs, vitamins, supplements, chiropractic, homeopathy, massage, and acupuncture.3 Medical conditions most frequently treated with CAM include respiratory and gastrointestinal (GI) ailments, musculoskeletal and skin complaints, and chronic conditions such as cystic fibrosis, cancer, autism, and arthritis.3,4
Clinicians should ask AYAs about their use of any form of CAM, especially herbal products and supplements, during the initial visit and every subsequent office visit to learn of all therapies that a patient is taking or using, to screen for drug-herb interaction, and to provide information to the patient about safety and efficacy. A gentle and knowledgeable approach goes far with the AYA patient and can be quite effective to illustrate that “natural” may not mean safe and an endorsement on an Internet site does not guarantee efficacy. Open communication with the clinician leads to a more informed patient and family who is less likely to rely on erroneous and false information obtained from friends, family, or the Internet.5
An ethical and legal dilemma may present itself to the clinician when a patient wishes to utilize an alternative treatment where there may be a lack of sufficient evidence to support its use and a paucity of safety data. According to Cohen and Kemper,6 important questions for AYAs and their families as health care providers who elect to use CAM include the following:
Will effective care be utilized when the patient’s condition is life-threatening?
Will using a CAM treatment deflect from conventional treatment?
What is known about the safety and/or efficacy of the treatment?
Has the patient consented to the use of CAM?
Would this proposed CAM therapy be acceptable to another clinician?
Overview and Regulation
Herbal retail sales reached an all-time high of $6.4 billion in 2012; up almost 3% in 2011, a growth of 16% over the past five years.8 The Dietary Supplement Health and Education Act (DSHEA) of 1994 defines herbal products as supplements because they are not tested according to the same scientific standards as conventional drugs. Packaging or marketing information does not need to be approved by the US Food and Drug Administration (FDA) before a product reaches the market. Supplements cannot be marketed for the diagnosis, treatment, cure, or prevention of disease, despite evidence to the contrary. They can only describe how the “structure and function” of the human body is affected. No protection is offered against misleading or fraudulent claims. The American Academy of Pediatrics Committee on Children with Disabilities has issued guidelines for discussing CAM use, specifically herbal therapies, with families.9
Herb-Drug Interactions and Toxicity
Important herb-drug interactions that clinicians should be aware of are outlined and easily accessible (www.standardprocess.com/MediHerb-Document-Library/Catalog-Files/herb-drug-interaction-chart.pdf). Antiplatelet activity and interaction with the cytochrome P450 (CYP) 3A4 enzyme system are two significant adverse effects noted in many herbs, in particular St. John’s wort (SJW).10 Patients suffering trauma who visit an emergency room or who are undergoing surgery should be questioned about use of herbal remedies. They should be counseled on the discontinuation of herbal remedies at least 2 weeks before surgery.11,12
A lack of quality control and regulation has resulted in contamination and misidentification of plant species. Herbal preparations may be contaminated with heavy metals or bacteria/fungal organisms while being manufactured or stored.
Dosing Issues and Active Compounds
In conventional medicine, clinicians have become accustomed to using pharmaceutical products standardized with the same strength and high quality; this is not always the case with herbal medicines. Because herbs represent complex entities containing hundreds of constituents, it is difficult to find one particular component representing the active agent. In many cases, particular herbal treatments have been evaluated with a focus on individual extracts and chemical entities such as Ginkgo biloba extract 761 (Egb 761). Patients should be counseled on the use of a clinically studied specific extract in an herbal product. Manufacturers may have their products tested for contamination and standard strength/quality, and the results of these assays are available online with the purchase of a membership (www.consumerlab.com).
The dosage and length of treatment of various herbal remedies are also controversial. With most pharmaceutical agents, as the dosage is increased, there is an increased risk of adverse effects. It is therefore wise to recommend using the lowest dosages of an herbal remedy.
Long-term Use
Most studies involving herbal treatments do not evaluate long-term effects. Herbal remedies should only be used on a limited basis until more data are available regarding long-term safety. AYAs wishing to remain on herbal remedies should be monitored periodically for signs of toxicity and potential adverse effects. Periodic measurements of liver function tests and renal function may be prudent. Ultimately, patients should be advised not to take herbal treatments long-term without the supervision of a clinician.
Use in Pregnancy and Lactation
Women contemplating pregnancy, currently pregnant, or nursing should not use herbal remedies, given the lack of evidence and safety studies.
Common Herbal Remedies
AYAs are likely to use herbal remedies to treat a number of conditions, including obesity, depression and anxiety, sleep disorders, upper respiratory tract infections, and also to improve athletic performance.13,14 AYAs with eating disorders may use herbal remedies to suppress appetite or induce vomiting.15
St. John’s Wort
Uses
SJW has historically been used for depression.
Mechanism of Action
The two active ingredients are hypericin and hyperforin which inhibit the reuptake of serotonin, norepinephrine, and dopamine as well as neurotransmitters.
Clinical Studies
Studies of SJW compared to tricyclic antidepressants (TCAs) and selective serotonin reuptake inhibitors (SSRIs) in patients with mild depression show that SJW was superior to placebo and as effective as low-dose TCAs and SSRIs.16
Adverse Effects
These include GI symptoms, dizziness, and confusion. Phototoxicity may occur with ingestion of high doses.
Drug Interactions
There is a significant interaction with cyclosporine, oral anticoagulants, oral contraceptives, and certain antiretroviral agents including indinavir due to SJW ability to induce the cytochrome P450 (CYP) 3A4 enzyme system.17,18 The concomitant use of SJW with standard antidepressants is also contraindicated because of the risk of serotonin syndrome.
Valerian Root
Uses
Valerian root is used for insomnia and as a sedative. It is also used for migraine headaches, fatigue, and intestinal cramps.
Mechanism of Action
It is felt that valerian root has effects on γ-aminobutyric acid (GABA) receptors, leading to its effects on insomnia.
Clinical Studies
In a review of 18 randomized controlled trails, valerian was effective subjectively for insomnia, although quantitative or objective measurements did not demonstrate efficacy.19
Adverse Effects
These include headache, excitability, uneasiness, and cardiac disturbances.
Drug Interactions
Care should be exercised when combining valerian root with other sedative agents and alcohol.
Chamomile
Uses
Chamomile has been used historically for GI discomfort, peptic ulcer disease, pediatric colic, and mild anxiety.
Mechanism of Action
Chamomile may act via binding to central benzodiazepine receptors.
Clinical Studies
Several small human trials have noted chamomile to have hypnotic-sedative properties. However, none of these trials have been randomized or controlled.
Adverse Effects
Several cases of significant allergic reactions to chamomile have been reported; no significant toxicity has been reported.
Drug Interactions
No drug-herb interactions have been noted.
Multiple supplements advertised effectively on the Internet are touted for weight loss, lipolysis, and decrease in hunger; yet, none have been shown through standard research methods to be proven efficacious.20
Ma Huang (Ephedra)
Uses
Ephedra, also known by its Chinese name Ma Huang, is a naturally occurring substance derived from plants. Its principal active ingredient is ephedra. In 2004, the FDA banned the sale of dietary supplement containing ephedra owing to reported serious adverse effects.
Mechanism of Action
Ephedra acts by increasing the levels of norepinephrine, epinephrine, and dopamine by stimulating α– and β-adrenergic receptors. This combination of adrenergic and dopaminergic effects leads to heightened alertness, decreased fatigue, and a lessened desire for sleep. The addition of caffeine to ephedra appears to blunt the negative feedback effect on the release of norepinephrine. At higher doses, the release of norepinephrine causes anxiety, restlessness, and insomnia.
Clinical Studies
In one randomized, double-blind trial, 90 obese adult subjects received one of the three treatments for 24 weeks: 200 mg caffeine/20 mg ephedrine, leptin A-200 or a combination of the leptin A-200 and caffeine/ephedrine. The caffeine/ephedrine and leptin combination groups lost more weight than the leptin only group.21
Adverse Effects
It is well known that Ma Huang has the potential to cause adverse effects that may be serious and have led to a number of reported deaths. Adverse effects include increased blood pressure, palpitations, tachycardia, chest pain, coronary vasospasm, and even cardiomyopathy. The structural similarity of ephedrine to amphetamine raises concern about possible abuse.
Guarana (Paullinia cupana, P. cyrsan, P. sorbilis)
Uses
Guarana is a small climbing maple plant native to Venezuela and northern Brazil known for the high stimulant content of the fruit. Guarana acts as a stimulant and contains the caffeine-like product guaranine along with theobromine theophylline, xanthine, and other xanthine derivatives and acts as a stimulant.22
Mechanism of Action
The applicable part of the guarana is the seed. Guarana contains 3.6% to 5.8% caffeine compared with 1% to 2% in coffee.
Adverse Effects
Due to the similarity to caffeine, care should be taken to discuss possible overdose of caffeine as guarana has the same toxicity profile.
Garcinia cambogia/Hydroxycitric Acid
Uses
Garcinia is marketed as an herbal weight loss product.
Mechanism of Action
It is thought that hydroxycitric acid can increase fat oxidation by inhibiting citrate lyase, an enzyme that plays a crucial role in energy metabolism during de novo lipogenesis.
Clinical Studies
In vivo studies support the antiobesity effects via increase in serotonin level regulation while reducing de novo lipogenesis. However, results from clinical studies showed both negative and positive antiobesity effects of Garcinia/hydroxycitric acid without definitive positive findings.24
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree