Highlights
- •
Mean medical care costs in the year following radical cystectomy were similar between bladder cancer patients who received an ileal conduit and those who received a neobladder.
- •
Mean monthly medical care costs were highest during the first quarter following radical cystectomy and decreased in the 3 quarters thereafter, among bladder cancer patients who underwent radical cystectomy and received a urinary diversion.
- •
The presence of post-cystectomy complications, advanced tumor stage at cystectomy, and death in the quarter were important drivers of medical care costs in the year following radical cystectomy.
Abstract
Purpose
Bladder cancer is 1 of the most costly cancers, however there is limited research on medical care costs by type of urinary diversion. The objective of our study was to compare medical care costs of the 2 most common urinary diversions in the year following radical cystectomy.
Methods
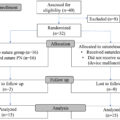
The Bladder Cancer Quality of Life Study included patients diagnosed with bladder cancer who underwent radical cystectomy and received an ileal conduit (IC, n = 821) or neobladder (NB, n = 181) in 3 integrated health systems. Medical care costs per patient per quarter were estimated for the year following cystectomy. Multivariable generalized linear models with a gamma distribution and log link were used to estimate mean monthly medical care costs (2022 USD$), adjusted for patient demographic and clinical characteristics.
Results
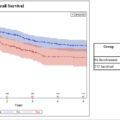
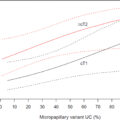
In multivariable analysis, mean monthly costs per quarter were not significantly different between IC and NB patients in the 12 months following cystectomy. Overall, mean monthly costs in IC and NB patients were highest during the first quarter and decreased thereafter. Factors associated with higher mean costs across all quarters included presence of any complications and advanced tumor stage at cystectomy (all P < 0.001).
Conclusion
Our study addresses an important knowledge gap by quantifying the medical costs of bladder cancer patients by urinary diversion type and comparing costs of different treatment approaches. Studies that assess patient-reported outcomes and out-of-pocket costs, by urinary diversion type, are warranted to inform treatment decision-making and cost conversations.
1
Introduction
Bladder cancer imposes significant health impacts, with approximately 81,180 new diagnoses and 17,100 deaths expected in the United States (US) in 2022 [ ]. It is also among the most costly cancers, with total annual national expenditures in the US projected to reach $11.6 billion by 2030 [ ]. For patients with advanced disease, treatment often involves removal of the bladder (radical cystectomy). Patients who have a radical cystectomy undergo urinary system reconstruction through urinary diversion (UD), among which the majority receive either an ileal conduit or neobladder [ ]. These treatment approaches are characterized by periods of high healthcare service use, with high risk of complications and readmission, and estimated 90-day direct hospital costs of nearly $40,000 (in US Dollars [USD]) [ ].
Previous research on medical costs of bladder cancer patients following radical cystectomy has largely focused on identifying drivers of high costs [ ]. Few studies having assessed medical care costs by UD type [ , ], most of which were based on medical care claims data. Nevertheless, understanding the direct medical costs associated with different UD types is important for comparative effectiveness analyses, as well as to inform cost containment efforts and guide treatment decision-making.
The Bladder Cancer Quality of Life (BCQOL) Study was a large mixed-method, comparative effectiveness study developed to compare costs, complications, and patient- and family-centered outcomes among bladder cancer patients undergoing cystectomy with a UD. The objective of the current analysis was to compare total medical care costs in the year following radical cystectomy between ileal conduit and neobladder patients, in addition to identifying potential drivers of cost. We hypothesized that medical care costs would differ by UD type.
2
Materials and methods
2.1
Study population
We included data on 1,002 adult (ages ≥ 21 years) patients who were members of one of three integrated health care systems who were diagnosed with bladder cancer between 01/01/2010–05/30/2015 and who underwent radical cystectomy with urinary diversion [ ]. The integrated health systems included three Kaiser Permanente (KP) regions—KP Northwest (Oregon and southwest Washington state), KP Northern California, and KP Southern California – serving a total of approximately 9.8 million members. For the current analysis, we included patients who received ileal conduit ( n = 821) or neobladder ( n = 181) UDs and excluded patients who received a continent pouch UD ( n = 30). The study received institutional review board approval from all 3 health systems.
2.2
Data sources
Data for this study were obtained from clinical and administrative data systems at the three participating sites, and included: demographic variables – age at cystectomy, sex, race, and Hispanic ethnicity; study site; health insurance type; clinical variables – year of cystectomy, UD type, Charlson-Deyo Comorbidity Index [ ], American Joint Committee on Cancer (AJCC) stage at cystectomy, presence of any complications in the year following cystectomy, vital status, robot-assisted surgery, and months since cystectomy. We extracted utilization data from hospital discharge abstracts; claims; hospital, emergency room, same-day surgical, and medical office ambulatory care encounters. Data were standardized across the participating sites according to specifications established by the Health Care System Research Network’s Virtual Data Warehouse [ ].
2.3
Medical care cost estimates
Medical care costs were calculated by applying cost coefficients to monthly counts of the following utilization categories: inpatient days, same-day surgeries, hospital ambulatory encounters, emergency room visits, and outpatient clinic visits. Outpatient visit counts were further divided into the following groups: primary care, oncology, nephrology, urology, cardiology, and other specialty visits. Cost coefficients were based on average cost per visit per utilization category, using a hybrid methodology from Medicare fee schedules (e.g., inpatient day, hospital ambulatory, same-day surgery) [ ] and administrative data from KP (i.e., medical care costs for services provided both in network and out of network. Cost coefficients used in the analysis are shown in Supplementary Table 1 . Monthly medical care costs per patient were estimated from the month of radical cystectomy (month 0) through the 11 months following cystectomy, then averaged across quarters: Quarter 1 (Q1) = month 0 through month 2; Quarter 2 (Q2)=month 3 through month 5; Quarter 3 (Q3) = month 6 through month 8; and Quarter 4 (Q4) = month 9 through month 11. Costs of the initial surgery were included as part of the first quarter cost estimates. Costs were adjusted for inflation using the Consumer Price Index for Medical Care in 2022 [ ].
2.4
Statistical analysis
We calculated descriptive statistics for patients with each UD type, including frequencies, means, proportions, and standard deviation (SD), for patient demographic and clinical characteristics [ ]. We present the mean and SDs for unadjusted monthly medical care utilization rates, by quarter and UD type, for the following service categories: inpatient stays and days, emergency department (ED) visits, primary care (PC) visits, and specialist visits.
To account for confounders, we developed a propensity score using logistic regression that included race, Hispanic ethnicity, health insurance type, sex, receipt of neoadjuvant therapy, body mass index and study site as predictors. The variables included in the propensity score were considered potential confounders based on prior research [ ]. To check the performance of the propensity score in achieving balance, we calculated standardized differences between the ileal conduit and neobladder patients before and after adjustment for the propensity score. The largest standardized difference prior to propensity score adjustment was .46 (for site 1) whereas after adjustment all values were near zero, with the largest difference being .015 for sex; well below the .10 cutoff proposed by Normand et al. [ ] and the 0.25 cutoff by Rubin [ ].
We used generalized linear models with a gamma distribution and log link [ ] to estimate mean monthly medical care costs per quarter, adjusting for UD type, age at cystectomy, Charlson-Deyo Comorbidity Index, presence of any complications, stage at cystectomy, year of cystectomy, robot-assisted surgery, death in quarter, and the propensity score. Adjustment variables were selected based on prior literature on medical costs of bladder cancer [ ]. Few studies having assessed medical care costs by UD type [ , ] Cost estimates and 95% confidence intervals (95% CI) for UD type, tumor stage at cystectomy, presence of any complications, surgical approach, and death in quarter were obtained from the multivariable model. In this complete-case study, SAS [version 9.1] and STATA [version 15] were used for all statistical analyses.
3
Results
3.1
Patient demographics
Study population characteristics by UD type are presented in Table 1 . Patients who received a neobladder were more likely to be younger (age at cystectomy ≤ 64 years, 59% vs. 22%, P < 0.001), female (90% vs. 76%, P < 0.001), have a lower comorbidity burden (Charlson-Deyo Comorbidity Index ≤ 2, 48% vs. 27%, P < 0.001), have lower tumor stage (AJCC stage at cystectomy 0 or 1, 30% vs. 21%, P < 0.001), and have undergone robotic surgery (22% vs. 8%, P <0.001) than patients who received an ileal conduit. Patients who received a neobladder were less likely than those who received an ileal conduit to die within the first year of surgery (13% vs. 25%, P < 0.001).
| Urinary Diversion Type | ||||
|---|---|---|---|---|
| Ileal Conduit | Neobladder | |||
| ( n = 821) | ( n = 181) | |||
| n | % | n | % | |
| Age group at Cystectomy a | ||||
| < 55 years | 26 | 3.2 | 37 | 20.4 |
| 55–64 years | 157 | 19.1 | 69 | 38.1 |
| 65–74 years | 296 | 36.1 | 59 | 32.6 |
| ≥ 75 years | 342 | 41.7 | 16 | 8.8 |
| Sex a | ||||
| Male | 627 | 76.4 | 162 | 89.5 |
| Female | 194 | 23.6 | 19 | 10.5 |
| Race | ||||
| White | 686 | 83.6 | 147 | 81.2 |
| Non-White | 135 | 16.4 | 34 | 18.8 |
| Hispanic Ethnicity | ||||
| Hispanic | 79 | 9.6 | 20 | 11.1 |
| Non-Hispanic | 742 | 90.4 | 161 | 89.0 |
| Charlson Comorbidity Index a | ||||
| ≤ 2 | 218 | 26.6 | 86 | 47.5 |
| 3 | 161 | 19.6 | 35 | 19.3 |
| 4 | 132 | 16.1 | 22 | 12.2 |
| ≥ 5 | 310 | 37.8 | 38 | 21.0 |
| AJCC Stage at Cystectomy a | ||||
| 0 or I | 171 | 20.8 | 55 | 30.4 |
| II | 194 | 23.6 | 64 | 35.4 |
| III or IV | 456 | 55.5 | 62 | 34.3 |
| Body Mass Index (BMI) | ||||
| Normal | 249 | 30.3 | 57 | 31.5 |
| Overweight | 349 | 42.5 | 72 | 39.8 |
| Obese | 223 | 27.2 | 52 | 28.7 |
| Surgical Approach a | ||||
| Robotic | 67 | 8.2 | 40 | 22.1 |
| Open | 754 | 91.8 | 141 | 77.9 |
| Any complications in the year following cystectomy | ||||
| Yes | 624 | 76.0 | 150 | 82.9 |
| No | 197 | 24.0 | 31 | 18.1 |
| Died within year after surgery a | 202 | 24.6 | 23 | 12.7 |
| Follow-up Time, months a | ||||
| Mean (SD) | 10.4 (3.1) | 11.2 (2.3) | ||
| Median (IQR) | 12.0 (8.3, 12.5) | 12.0 (9.6,12.8) | ||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree