Highlights
- •
Tumor size has a higher predictive ability for prognosis in IOIO therapy compared to IOTKI.
- •
Time-dependent AUC analysis shows tumor size consistently predicts PFS and OS in IOIO therapy.
- •
Tumor size outperforms nephrectomy status and IMDC risk classification in IOIO cases.
- •
Tumor size should be a key factor in treatment decisions for mRCC, especially in IOIO therapy.
Abstract
Objectives
We aimed to investigate the prognostic significance of tumor size in metastatic renal cell carcinoma (mRCC) by comparing the effectiveness of dual immune checkpoint inhibitor (IOIO) and immune checkpoint inhibitor combined with tyrosine kinase inhibitor (IOTKI) therapies.
Methods
This retrospective observational study included patients with mRCC diagnosed between October 2014 and February 2024 who received IOIO or IOTKI treatment at Kobe University Hospital and 5 affiliated hospitals. Clinical and imaging data were collected, and target lesions were measured according to RECIST v.1.1 criteria. Time-dependent ROC curve analysis was performed to evaluate the prognostic value of tumor size, nephrectomy status, and IMDC risk criteria for progression-free survival (PFS) and overall survival (OS).
Results
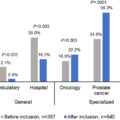
The study included 180 mRCC patients, consisting of 99 receiving IOIO therapy and 81 receiving IOTKI therapy. Time-dependent AUC analysis showed that tumor size had a higher predictive ability for PFS and OS in the IOIO group than the IOTKI group. In multivariate analysis, tumor size was a significant independent prognostic factor for PFS (HR: 1.010, 95% CI: 1.004–1.016, P < 0.001) in the IOIO group. Moreover, the AUC for tumor size was consistently superior in predicting outcomes compared to nephrectomy status and IMDC risk classification in the IOIO group. Kaplan-Meier curves indicated that tumor size effectively stratified PFS in both nephrectomized and non-nephrectomized cases.
Conclusion
Tumor size significantly impacts the prognosis of mRCC patients treated with IOIO therapy, demonstrating greater predictive ability than nephrectomy status and IMDC risk classification. These findings suggest that tumor volume should be considered a critical factor in treatment decision-making for renal cancer, particularly in patients undergoing IOIO therapy.
1
Introduction
It is widely recognized that tumor size significantly impacts treatment outcomes and prognosis in various types of cancer [ ]. Larger volume tumors are more challenging to completely resect surgically, and the increased number of cancer cells may lead to greater resistance to treatment, complicating therapeutic efforts [ ]. Therefore, formulating treatment strategies that consider tumor volume is crucial. Recently, the advent of immune checkpoint inhibitors (ICIs) has enabled the provision of more effective treatments for metastatic renal cell carcinoma (mRCC) with substantial tumor sizes. Notably, combination therapies, such as ipilimumab-nivolumab, which involve dual ICI (IOIO) therapy, and avelumab-axitinib, pembrolizumab-axitinib, nivolumab-cabozantinib, and pembrolizumab-lenvatinib, which combine ICIs with tyrosine kinase inhibitors (IOTKI), have emerged [ ]. However, the differentiation in the use of these treatments and their effectiveness on different patient subgroups remain unclear.
Our previous study on the impact of prior nephrectomy on the efficacy of IOIO and IOTKI treatments [ , ] found that nephrectomy significantly affects prognosis in IOIO therapy but has a lesser impact in IOTKI therapy. The sum of tumor size changes significantly depending on the presence of nephrectomy. However, our previous studies did not thoroughly examine how this size affects prognosis. We conducted a retrospective analysis to investigate the impact of tumor size on prognosis in IOIO and IOTKI treatments.
2
Methods
This study was a retrospective observational study targeting patients with metastatic renal cell carcinoma. The subjects were patients diagnosed with mRCC between October 2014 and February 2024 who received either IOIO or IOTKI treatment and had available clinical and imaging data from Kobe University Hospital and 5 affiliated hospitals. This study was approved by the Ethics Committee of Kobe University (No. B240026) and was conducted in accordance with the Declaration of Helsinki.
Clinical characteristics and blood test data were collected within 3 days before the initiation of systemic therapy. Imaging data included chest and abdominal CT and bone scintigraphy performed before IOIO or IOTKI treatment. mRCC was diagnosed based on radiologists’ interpretation of imaging studies during routine clinical practice. Non-clear cell RCC was diagnosed according to WHO classification and confirmed by pathological assessment. In this study, target lesions were measured according to Response Evaluation Criteria in Solid Tumors v.1.1 criteria [ ]. The sum of target lesions was recorded as a continuous variable, and patients without target lesions were excluded. The selection of both systemic treatments (IOIO or IOTKI) and the decision to perform nephrectomy were determined by the treating physicians based on their clinical judgment at the time of treatment.
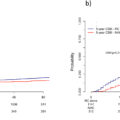
Data analysis was performed using R software. To evaluate the performance of the sum of target lesions over time and IMDC risk in predicting progression-free survival (PFS) and overall survival (OS), we used time-dependent receiver operating characteristic (ROC) curve analysis. This method assesses how well the size of the target lesions predicts patient outcomes at different time points. The area under the ROC curve (AUC) was calculated for each time point from 15 to 365 days for the IOIO and IOTKI groups. The AUC represents a measure of the model’s ability to distinguish between patients who experience the event (progression or death) and those who do not at each time point.
We plotted the AUC over time by calculating the ROC curve at multiple time points, providing a dynamic view of how the prognostic value of tumor size, nephrectomy status, and IMDC risk criteria evolved during the follow-up period.
Survival curves were created using the Kaplan-Meier method, based on the cut-off values obtained from the time-dependent ROC curves predicting disease control at 1 year. These curves were then compared using the log-rank test to determine if there were significant differences in survival between groups with different tumor sizes. Additionally, a Cox proportional hazards model was used to perform multivariate analysis, adjusting for factors such as IMDC status, histological subtype, prior nephrectomy, and the presence of liver or bone metastasis, to assess the independent prognostic value of tumor size for PFS and OS.
3
Results
A total of 193 patients with mRCC received first-line combination therapy with ICIs. After excluding 13 patients without target lesions, we enrolled 99 patients who received IOIO therapy and 81 patients who received IOTKI therapy. The median observation period was 29.5 months (range: 1.6–102.7 months) for the IOIO group and 14.2 months (range: 2.4–43.9 months) for the IOTKI group. A total of 101 patients experienced disease progression, and 69 died. The patient selection process for this study is outlined in a flowchart provided in Supplementary Fig. 1 .
Patient backgrounds are shown in Table 1 . In the IOIO group, 58 patients (58.6%) underwent nephrectomy, with a median target lesion size of 66 mm (range: 10–245 mm). In the IOTKI group, 34 patients (41.5%) underwent nephrectomy, with a median target lesion size of 103 mm (range: 10–265 mm). The IOIO group also provided detailed patient backgrounds according to nephrectomy status. The median total size of the target lesions was 31 mm in the group with previous nephrectomy and 126 mm in the group without nephrectomy.
| Entire cohort | IOIO group according to nephrectomy status. | ||||
|---|---|---|---|---|---|
| IOTKI therapy | IOIO therapy | Without nephrectomy | Nephrectomy | ||
| N=82 | N=99 | N=41 | N=58 | ||
| Age, median (years, range) | 71 (48–89) | 70 (30–84) | 70 (30–84) | 70 (32–83) | |
| Sex (%) | Male | 68 (81.0) | 78 (78.8) | 33 (80.5) | 45 (77.6) |
| Female | 16(19.0) | 21 (21.2) | 8 (19.5) | 13 (22.4) | |
| BMI, median (range) | 22.4 (15.5–39.2) | 22.4 (15.0–32.6) | 22.2 (15.0–30.6) | 22.5 (16.7–32.6) | |
| Histological type (%) | Clear RCC | 72 (87.8) | 75 (75.8) | 30 (73.2) | 45 (77.6) |
| Non clear RCC | 10 (11.9) | 24 (24.7) | 11 (26.8) | 13 (22.4) | |
| Nephrectomy (%) | Presence | 34 (41.5) | 58 (58.6) | 0 | 58 (100) |
| IMDC risk classification(%) | Favorable | 8 (9.8) | 0 | 0 | 0 |
| Intermediate | 37 (45.1) | 60 () | 15 (38.6) | 45 (77.6) | |
| Poor | 37 (45.1) | 39 () | 26 (63.4) | 13 (22.4) | |
| Multiple metastasis (%) | Presence | 61 (74.4) | 90 (90.9) | 38 (92.7) | 52 (89.7) |
| Liver metastasis (%) | Presence | 16 (19.5) | 14 (14.1) | 2 (4.9) | 12 (20.7) |
| Bone metastasis (%) | Presence | 29 (35.4) | 38 (38.4) | 22 (53.7) | 16 (27.6 |
| Lymph node metastasis (%) | Presence | 24 (29.3) | 46 (46.5) | 22 (53.7) | 24 (41.1) |
| Sum size of target lesions, median (mm, range) | 103 (10–265) | 66 (10–245), | 126 (38–233) | 31 (10–245) | |
| Systemic therapy (%) | Ipilimumab plus nivolumab | 99 (100) | 41 (100 | 58 (100) | |
| Avelumab plus axitinib | 24 (29.3) | ||||
| Pembrolizumab plus axitinib | 14(17.1) | ||||
| Nivolumab plus cabozantinib | 24 (29.3) | ||||
| Pembrolizumab plus lenvatinib | 20 (24.4) | ||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree