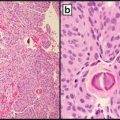
Fig 21.1
Successful reimbursement depends on accurate coding of the service, insurance coverage of the service, and adequate pricing of the service
The standard for coding medical services in the USA is Current Procedural Terminology (CPT®), fourth edition [3], which is owned and managed by the American Medical Association (AMA). Individuals, professional associations, vendors, or any other group wishing to change or add to the current code set first submits a Code Change Proposal (CCP) to the AMA [4]. The CCP is referred for comments and recommendations to the AMA’s CPT Advisory Committee, which consists of members and alternates from 87 physician organizations that have seats in the AMA House of Delegates. All pathology and laboratory-related CCPs are also referred to the Pathology Coding Caucus (PCC), which is composed of AMA CPT Advisors from pathology and clinical laboratory-related organizations as well as several additional members from other national clinical laboratory organizations that are not members of the AMA CPT Advisory Committee (Table 21.1). The PCC is jointly managed by the standing members, the AMA, and the College of American Pathologists (CAP). The CCP and the comments and recommendations from the CPT Advisors and the PCC are considered at the meetings of the CPT Editorial Panel (Table 21.2), and are accepted (with or without modifications) or rejected for inclusion into the formal CPT code set. Among the criteria used by the CPT Editorial Panel to create a new CPT code for a specific procedure are the following. Has the procedure received Food and Drug Administration (FDA) approval (if applicable)? Does the procedure represent a distinct service that is not a part of an already existing CPT code? Is the procedure widely performed in many medical settings? Has the efficacy of the procedure been well documented in the peer-reviewed literature? Is the new code being proposed only to describe performance in an extraordinary circumstance of a procedure that already has a CPT code? A procedure fulfilling all of these criteria may be eligible for a Category I CPT code. For procedures not fulfilling the Category I criteria, a Category III code may be considered, as long as the procedure is currently or recently performed in humans and it meets at least one of the following additional criteria: at least one CPT or Health Care Professionals Advisory Committee member supports the CCP, clinical efficacy is supported by peer-reviewed literature (in English), there is at least one Institutional Review Board (IRB)-approved protocol to study the procedure, there is a description of an existing US clinical trial, or other evidence of evolving clinical utilization.
Table 21.1
Pathology coding caucus
Standing members | American Medical Associationa |
College of American Pathologistsa | |
Core members | American Society for Clinical Pathologya |
American Society of Cytopathologya | |
United States and Canadian Academy of Pathologya | |
National Association of Medical Examinersa | |
American Association for Clinical Chemistry | |
Advanced Medical Technology Association | |
American Clinical Laboratory Association | |
Rotating members | American Association of Bioanalysts |
Association for Molecular Pathology | |
American Society for Microbiology | |
Clinical Laboratory Management Association |
Table 21.2
AMA CPT editorial panel composition
Category of membership | Nominating organization |
|---|---|
Regular Physician (7 members) | AMA Medical Specialty Societies |
Rotating Physician (4 members) | AMA Medical Specialty Societies |
Physician | Blue Cross Blue Shield Association |
Physician | America’s Health Insurance Plans |
Physician | American Hospital Association |
Physician | CMS |
Non-Physician Member (2 members) | AMA Health Care Professionals Advisory Committee |
Once a new procedure has been assigned a CPT code, it must be assigned a value for payment. For clinical laboratory tests that are paid under the Medicare’s Clinical Laboratory Fee Schedule (CLFS) [5], the Centers for Medicare and Medicaid Services (CMS) establishes the payment ceiling (the National Limitation Amount, or NLA) with input from professional societies, and assigns the new values to CLFS. CMS uses two methodologies to establish fees for new services. If the new service uses methodology and resources in a manner similar to that for a pre-existing procedure, or some combination of pre-existing procedures already on the CLFS, CMS will “crosswalk” the new code to the existing code(s). Medicare payment is the lower of the actual charge, the local Medicare contractor payment, or the NLA.
If no appropriate crosswalk can be identified for a new code, CMS will use the “gap-fill” methodology, whereby they will rely on local Medicare contractors to establish a price during the first quarter of a new calendar year. Medicare payment will be the lower of the actual charge or the local contractor price until CMS establishes an NLA. CMS will then use these contractor set prices to determine the NLA for the following year. Currently, CMS sets the NLA at 100 % of the contractor median [6].
For new procedures that will be paid under the Medicare Physician Fee Schedule (PFS), the AMA’s Relative Value Scale Update Committee (RVS Update Committee, or RUC) determines the relative value units [7]. For many pathology services, there is both a technical component (TC), which may be provided by technical laboratory personnel, and a professional component (PC), which is provided by a physician or other qualified healthcare professionals. The RUC recommendations are submitted to CMS, and more than 90 % of the time are accepted by CMS. Medicare payment for physician services is calculated by multiplying the current Medicare conversion factor by the relative value unit (RVU). The RUC membership is shown in Table 21.3.
Table 21.3
Relative Value Scale Update Committee (RUC)
Category of membership | Nominating organization |
|---|---|
Chair | AMA |
Permanent | AMA |
Permanent | AMA CPT Editorial Panel |
Permanent | American Osteopathic Association |
Permanent | Health Care Professionals Advisory Committee |
Permanent | AMA Practice Expense Advisory Committee |
Permanent (21 members) | AMA Specialty Societies |
Rotating (4 members) | AMA Specialty Societies |
Private insurers often base their own coverage and payment decisions on Medicare decisions, and often set their payment rate at some percentage of the Medicare payment. Hence, the role of Medicare payment policy cannot be overestimated. In the early phases of new procedure introduction, insurers may make case-by-case determinations. Later, as the use of the procedure becomes more widespread, Medicare and other insurers will develop a national coverage policy. Medicare local coverage determinations are developed by the local Medicare contractors, with input from their Contractor Advisory Committees (CAC). It is in the best interests of providers to either serve on or have close working relationships with their CAC and the Medicare Contractor Medical Director in order to insure input into this process. As the procedure becomes more widespread, CMS may make a national coverage determination (NCD) [8]. The Medicare Evidence Development & Coverage Advisory Committee may provide input for the NCD, but the final decision on all coverage decisions is made by CMS staff. Private insurers may have their own technology assessment panels [9]. The terms of each contract may address coverage for particular procedures, as determined by employers or other large purchasing groups. The coverage criteria are similar to those used by the CPT Editorial Panel to grant a new CPT code, and are shown in Table 21.4.
Table 21.4




Blue Cross and Blue Shield Association technology evaluation center criteria
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree