Fig. 40.1
Neck ultrasound of the left paratracheal lesion in April 1999, before the surgical excision, the histology of which demonstrated a medullary thyroid cancer local recurrence. (Panel a) Standard neck ultrasound transverse section with the anteroposterior (28.0 mm) and latero-lateral (19.1 mm) diameters of the paratracheal lesion. (Panel b) Color-Doppler imaging of the paratracheal lesion showing the intralesion irregular hypervascularity (sagittal section, 32 mm)
Fig. 40.2
Serum Ct and CEA variations during the follow-up of the patient: a correlation between the two markers is evident as well as a correlation with therapeutic interventions
In 2001, basal Ct was still <14 pg/ml but a pentagastrin stimulation test showed a peak Ct of 88 pg/ml. At this time, both neck ultrasound and total body CT scan were still negative.
From 2001 to 2005, the patient, by her choice, did not undergo any biochemical or radiological assessment. In February 2005, she returned to our center, and at that time, serum Ct was 21 pg/ml; neck ultrasound and neck CT scan showed subcentimeter lymph nodes that were not clearly metastatic. No distant metastases were present, and a total body bone scan was negative. We continued to follow our patient with clinical, biochemical, and imaging assessment every 12 months, and from 2005 to 2009, the disease was stable.
In June 2009, the total body CT scan showed the persistence of small lymph nodes in the neck, the appearance of micronodules in the lung, and three new hepatic lesions (largest was 12 mm) with radiographic characteristics suspicious for metastatic lesions. Serum Ct levels had slowly increased up to 69 pg/ml while serum CEA was in the normal range (<5 ng/ml). We decided to not recommend active therapies but to follow the strategy of “wait and see.”
During the following 3 years, radiological assessments showed the progression of the hepatic metastases; in particular, the one that had been 12 mm in 2009 grew to 14 mm in 2010, 15 mm in 2011, and 17 mm in September 2012 (Fig. 40.3, Panel a) with a mean size increase of 20% per year. In parallel, serum Ct increased from 69 pg/ml on June 2009 to 314 pg/ml on September 2012 and CEA levels from 3.12 ng/ml on June 2009 to 15.6 ng/ml on September 2012 (Fig. 40.2). At this moment, the doubling time of both Ct and CEA was 1.5 years.
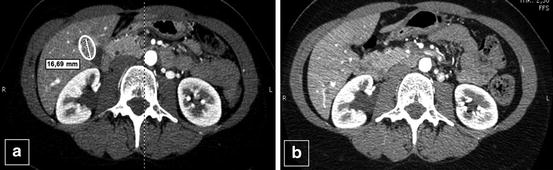
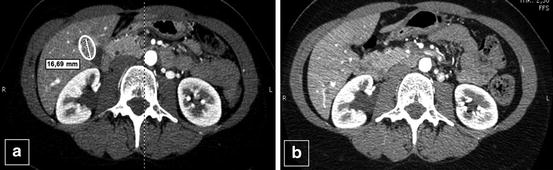
Fig. 40.3
(Panel a) CT scan of the hepatic metastases, with the largest one located very close to the gallbladder and measuring 17 mm in September 2012. (Panel b) Patient’s liver CT scan 12 months after metastasectomy in 2014: no recurrence of the largest lesion was visible
In January 2013, the total body CT scan confirmed that the only growing lesion was the hepatic one which was now 19 mm. At this point, we explored the possibility of performing locoregional percutaneous thermoablation, but because of its close relationship with the gallbladder and the risk for unsuccessful treatment, we agreed on a surgical approach and the patient underwent hepatic metastasectomy.
One year later, at the last visit in February 2014, serum Ct was greatly reduced (25 pg/ml, normal range <11.5 pg/ml) as well as the CEA (1.7 ng/ml, normal range <5 ng/ml), and radiological assessments confirmed the stability of small cervical lymph nodes, small lung nodules, and the other two subcentimeter hepatic lesions, in the absence of new metastatic or suspicious lesions (Fig. 40.3, Panel b). The patient is now 42 years old; her general health is good as is her quality of life.
Diagnosis/Assessment
This case offers the opportunity to discuss several still controversial issues related to the diagnosis and the assessment of metastatic disease in MTC patients.
MTC is a rare thyroid tumor representing only 5–7 % of all thyroid malignancies. It can be sporadic (80%) or familial (20%). Its pathogenesis is related to a molecular alteration of RET oncogene that can be present at the germline level in familial cases or at somatic level in sporadic cases [1]. MTC prognosis is strongly related to the presence of metastatic disease outside the neck, with a survival rate of about 30–35 % at 10 years when distant metastases are present at the time of diagnosis [2]. Also the presence of a somatic RET mutation has been demonstrated to be correlated to an advanced stage and a lower survival [3–5]. The detection of a somatic RET mutation in the paratracheal tissue of the patient is suggestive of a more aggressive phenotype, with a higher risk of disease-related mortality even though the absence of distant metastases at the time of diagnosis likely reduces this risk [3].
This is a typical case in which the presurgical diagnosis of MTC was missed since the serum Ct was not measured and the cytological diagnosis of the nodule was indeterminate, as it can sometimes happen in MTC. An international and multicenter study recently demonstrated that the FNAC was able to identify only 46 % of 245 sporadic MTCs evaluated in 12 centers across 7 nations in 4 continents [6]. In this case, the measurement of serum Ct could have helped to avoid this mistake and allowed the appropriate surgical procedure to have been performed, which would possibly have changed the long-term outcome.
The measurement of Ct in the washout of the needle used for aspiration is of great help in the diagnosis of both primary MTC and lymph node metastases [7]. This procedure is particularly useful when the cytology is unclear or undefined and the serum Ct is borderline. Sometimes, if the serum Ct levels are very high, blood contamination can lead to a false-positive result, but the identification of a cutoff above which metastatic disease is likely can solve this problem [8].
At a certain point during the follow-up of this patient, she could have been considered to be “cured” since the serum Ct was undetectable (<14 pg/ml) from 1999 to 2001. However, the pentagastrin stimulation test demonstrated a peak Ct of 88 pg/ml suggesting that residual disease was still present. It is still a matter of discussion if postsurgical Ct stimulation testing is worthwhile when the postsurgical basal serum Ct is undetectable or in the normal range. There are studies showing that MTC patients with a basal Ct lower than the upper limit of the reference range have a risk of recurrence of 10 %, and therefore they can be considered to be cured, and their follow-up can be less intensive [9]. However, this percentage is reduced to 3 % in patients with negative Ct stimulation test [10], and thus, we believe that at least one stimulation Ct test after surgery can be useful to better identify patients who have a higher probability of being free of disease [11].
Management
Newly diagnosed patients with MTC are usually 45–50 years old at the time of the diagnosis, and thus our patient was rather young. However, age at presentation is not a risk factor neither for the progression of the disease nor survival. However, younger age can impact on the choice of therapy. For example, after the third surgery, external radiotherapy (ERT) might have been considered, but the patient was only 25 years old, and her young age was a relative contraindication to ERT [12]. Nevertheless, no further recurrence in the neck has been observed thus far, after 15 years from the last surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





