Clinical Implications of the Aging Process: Introduction
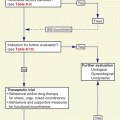
Gerontology (both basic and applied)
Chronic disease management, especially multimorbidities
End-of-life care
Principles of gerontology can help to explain insights of geriatric care. For example, the presentation of disease is often different in older persons because the response to stress is different. A hallmark of aging is a decreased ability to respond to stress. The body’s stress response is what typically generates the symptoms of an illness. Older people fail to respond as actively. Hence, they may not have spiking fevers or elevated white blood cell counts in the face of an infection. Heart disease may be silent.
Chronic disease management is difficult on its own. It is much more difficult when an older patient suffers from multiple simultaneous diseases. Basic care guidelines may not work. Indeed, they may pose a threat (Boyd et al., 2005).
Much of the emphasis in care planning is directed at containing disease and maintaining function and improving quality of life. Death is a part of old age. Geriatrics must deal with that reality and help patients and families deal with end of life, helping them to make informed decisions that reflect their goals and priorities. But geriatrics cannot focus exclusively on end-of-life care. One compromise has been the evolution of palliative care (discussed in Chapter 18). To this triad, some might also add a role for advocating reasonable preventive actions (see Chapter 5).
The care of older patients differs from that of younger patients for a number of reasons. While there continues to be a debate about the cause of these differences, it is likely that they are a combination of biological changes that occur during the course of aging, associated diseases, and attitudes and beliefs of older adults and their caregivers. Aging is defined as the time-sequential deterioration that occurs in most living beings, including weakness, increased susceptibility to disease and adverse environmental conditions, loss of mobility and agility, and age-related physiological changes (Goldsmith, 2006). At least in vitro, it is clear that the “aging clock” can be reset (reviewed in Rando and Chang, 2012). Somatic cell nuclear transfer of the nucleus of a mature somatic cell into an enucleated oocyte can give rise to mature, fertile animals.
It is important to distinguish life expectancy from life span. The former refers to what proportion of the possible maximum age a person may live. The latter suggests a biological limit to how many years a species can expect to survive. In general, geriatrics has the most to contribute to improving life expectancy, but new genetic breakthroughs may ultimately affect life span as well. Another helpful distinction is between chronological aging and gerontological aging. The latter is calculated on the basis of the risk of dying, the so-called force of mortality. Thus, two people of the same chronological age may have biologically very different ages depending on their health state. Some of that propensity for death is malleable; some is simply predictable.
Perhaps one of the most intriguing challenges in medicine is to unravel the process of aging. From a medical perspective, the question continues to haunt us as to whether aging is a feature of an organism’s design that has evolved over time and is beneficial to the survival of species, or aging is a disease or defect that confers no survival benefit. Even more important to medical management of aging is the question of whether there are medically treatable factors that are common to the various manifestations of aging we see. Could aging treatments delay the signs and symptoms of aging such as sensory changes, musculoskeletal problems, or skin-related changes?
Nonetheless, the distinction between so-called normal aging and pathologic changes is critical to the care of older people. We wish to avoid both dismissing treatable pathology as simply a concomitant of old age and treating natural aging processes as though they were diseases. The latter is particularly dangerous because older adults are so vulnerable to iatrogenic effects.
There is growing appreciation that everyone does not age in the same way or at the same rate. The changing composition of today’s older adults compared with that of a generation ago may actually reflect a bimodal shift wherein there are both more disabled people and more healthy older people. We continue to learn more and more about healthy or successful aging through hearing the stories of the growing number of centenarians. Generally the consensus is that moderation in all areas (eg, food intake, alcohol intake), regular physical activity, and an engaging social life are critical to successful aging. A recent large actuarial study (Gavrilova and Gavrilov, 2005) further suggested that environmental factors may also be relevant. Social factors can also play a strong role (Banks et al., 2006). The challenge is to recognize and appreciate aging changes while using resources to prevent or halt further changes and overcome aging challenges.
Changes Associated with “Normal” Aging
Clinicians often face a major challenge in attributing a finding to either the expected course of aging or the result of pathologic changes. This distinction perplexes the researcher as well. We currently lack precise knowledge of what constitutes normal aging. Much of our information comes from cross-sectional studies, which compare findings from a group of younger persons with those from a group of older individuals. Such data may reflect differences other than simply the effects of age, such as those associated with lifestyle behaviors (physical activity, alcohol intake, smoking, and diet), as well as prophylactic medication management. For example, older adults in the coming century may present with less evidence of osteoporosis because of prophylactic lifelong intake of high calcium and vitamin D diets, regular physical activity, and early interventions with biphosphanates and potentially future treatments for osteoporosis. Statins can drastically affect the course of cardiovascular disease.
Many of the changes associated with aging result from a gradual loss of homeostatic mechanisms. (Jack Rowe termed this “homeostenosis.”) These losses may often begin in early adulthood, but—thanks to the redundancy of most organ systems—the decrement does not become functionally significant until the loss is fairly extensive.
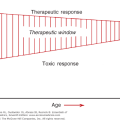
The concept of aging, or at least what constitutes old age, has changed as life expectancy has increased, although the biology has not. Based on cross-sectional comparisons of groups at different ages, most organ systems seem to lose function at about 1% a year beginning around age 30 years. Other data suggest that the changes in people followed longitudinally are much less dramatic and certainly begin well after age 70 years. In some organ systems, such as the kidney, a subgroup of persons appears to experience gradually declining function over time, whereas others’ function remains constant. These findings suggest that the earlier theory of gradual loss must be reassessed as reflecting disease rather than aging. Given a pattern of gradual deterioration—whether from aging or disease or both—we are best advised to think in terms of thresholds.
The loss of function does not become significant until it crosses a given level. Thus, the functional performance of an organ in an older person depends on two principal factors: (1) the rate of deterioration and (2) the level of performance needed. It is not surprising then to learn that most older persons will have normal laboratory values. The critical difference—in fact, the hallmark of aging—lies not in the resting level of performance but in how the organ (or organism) adapts to external stress. For example, an older person may have a normal fasting blood sugar but be unable to handle a glucose load within the normal parameters for younger subjects.
This failure to respond to stress explains the atypical presentation of many diseases in older patients. Many of the signs and symptoms of disease are actually the body’s response to those assaults. A depressed response will mean not having a high white blood cell count with an infection or even pain with a heart attack. For example, although currently not recommended for screening of asymptomatic patients, cardiac magnetic resonance imaging reveals unrecognized myocardial infarctions in asymptomatic older adults that are associated with increased mortality (Schelbert et al., 2012).
The same pattern of decreased response to stress can be seen in the performance of other endocrine systems or the cardiovascular system. An older individual may have a normal resting pulse and cardiac output but be unable to achieve an adequate increase in either with exercise.
Sometimes the changes of aging work together to produce apparently normal resting values in other ways. For example, although both glomerular filtration and renal blood flow decrease with age, many elderly persons have normal serum creatinine levels because of the concomitant decreases in lean muscle mass and creatinine production. Thus serum creatinine is not as good an indicator of renal function in older adults as in younger persons. Knowledge of kidney function is critical in drug therapy. Therefore, it is important to get an accurate measure of kidney function. A useful formula for estimating creatinine clearance on the basis of serum creatinine values in the elderly was developed (Cockcroft and Gault, 1976). (The actual formula is provided in Chapter 14.) Table 1–1 (Schmidt, 1999) summarizes some of the pertinent changes that occur with aging. For many items, the changes begin in adulthood and proceed gradually; others may not manifest themselves until well into seniority.
System | Common age changes | Implications of changes |
|---|---|---|
Cardiovascular | Atrophy of muscle fibers that line the endocardium Atherosclerosis of vessels Increased systolic blood pressure Decreased compliance of the left ventricle Decreased number of pacemaker cells Decreased sensitivity of baroreceptors | Increased blood pressure Increased emphasis on atrial contraction with an S4 heard Increased arrhythmias Increased risk of hypotension with position change Valsalva maneuver may cause a drop in blood pressure Decreased exercise tolerance |
Neurological | Decreased number of neurons and increase in size and number of neuroglial cells Decline in nerves and nerve fibers Atrophy of the brain and increase in cranial dead space Thickened leptomeninges in spinal cord | Increased risk for neurological problems: cerebrovascular accident Parkinsonism Slower conduction of fibers across the synapses Modest decline in short-term memory Alterations in gait pattern: wide based, shorter stepped, and flexed forward Increased risk of hemorrhage before symptoms are apparent |
Respiratory | Decreased lung tissue elasticity Thoracic wall calcification Cilia atrophy Decreased respiratory muscle strength Decreased partial pressure of arterial oxygen (Pao2) | Decreased efficiency of ventilatory exchange Increased susceptibility to infection and atelectasis Increased risk of aspiration Decreased ventilatory response to hypoxia and hypercapnia Increased sensitivity to narcotics |
Integumentary | Loss of dermal and epidermal thickness Flattening of papillae Atrophy of sweat glands Decreased vascularity Collagen cross-linking Elastin regression Loss of subcutaneous fat Decreased melanocytes Decline in fibroblast proliferation | Thinning of skin and increased susceptibility to tearing Dryness and pruritus Decreased sweating and ability to regulate body heat Increased wrinkling and laxity of the skin Loss of fatty pads protecting bone and resulting in pain Increased need for protection from the sun Increased time for healing of wounds |
Gastrointestinal | Decreased liver size Less efficient cholesterol stabilization and absorption Fibrosis and atrophy of salivary glands Decreased muscle tone in bowel Atrophy of and decrease in number of taste buds Slowing in esophageal emptying Decreased hydrochloric acid secretion Decreased gastric acid secretion Atrophy of the mucosal lining Decreased absorption of calcium | Change in intake caused by decreased appetite Discomfort after eating related to slowed passage of food Decreased absorption of calcium and iron Alteration of drug effectiveness Increased risk of constipation, esophageal spasm, and diverticular disease |
Urinary | Reduced renal mass Loss of glomeruli Decline in number of functioning nephrons Changes in small vessel walls Decreased bladder muscle tone | Decreased GFR Decreased sodium-conserving ability Decreased creatinine clearance Increased BUN Decreased renal blood flow Altered drug clearance Decreased ability to dilute urine Decreased bladder capacity and increased residual urine Increased urgency |
Reproductive | Atrophy and fibrosis of cervical and uterine walls Decreased vaginal elasticity and lubrication Decreased hormones and reduced oocytes Decreased seminiferous tubules Proliferation of stromal and glandular tissue Involution of mammary gland tissue | Vaginal dryness and burning and pain with intercourse Decreased seminal fluid volume and force of ejaculation Reduced elevation of the testes Prostatic hypertrophy Connective breast tissue is replaced by adipose tissue, making breast examinations easier |
Musculoskeletal | Decreased muscle mass Decreased myosin adenosine triphosphatase activity Deterioration and drying of joint cartilage Decreased bone mass and osteoblastic activity | Decreased muscle strength Decreased bone density Loss of height Joint pain and stiffness Increased risk of fracture Alterations in gait and posture |
Sensory: Vision | Decreased rod and cone function Pigment accumulation Decreased speed of eye movements Increased intraocular pressure Ciliary muscle atrophy Increased lens size and yellowing of the lens Decreased tear secretion | Decreased visual acuity, visual fields, and light/dark adaptation Increased sensitivity to glare Increased incidence of glaucoma Distorted depth perception with increased falls Less able to differentiate blues, greens, and violets Increased eye dryness and irritation |
Sensory: Hearing | Loss of auditory neurons Loss of hearing from high to low frequency Increased cerumen Angiosclerosis of ear | Decreased hearing acuity and isolation (specifically, decreased ability to hear consonants) Difficulty hearing, especially when there is background noise, or when speech is rapid Cerumen impaction may cause hearing loss |
Sensory: Smell, taste, and touch | Decreased number of olfactory nerve fibers Altered ability to taste sweet and salty foods; bitter and sour tastes remain Decreased sensation | Inability to smell noxious odors Decreased food intake Safety risk with regard to recognizing dangers in the environment: hot water, fire alarms, or small objects that result in tripping |
Endocrine | Decreased testosterone, GH, insulin, adrenal androgens, aldosterone, and thyroid hormone Decreased thermoregulation Decreased febrile response Increased nodularity and fibrosis of thyroid Decreased basal metabolic rate | Decreased ability to tolerate stressors such as surgery Decreased sweating and shivering and temperature regulation Lower baseline temperature; infection may not cause an elevation in temperature Decreased insulin response, glucose tolerance Decreased sensitivity of renal tubules to antidiuretic hormone Weight gain Increased incidence of thyroid disease |
Theories of Aging
It is helpful to be familiar with the many theories of aging, as these theories help direct the philosophy of care that is provided. If we believe that there is no way to intervene in the aging process, we will likely help our older patients accept and adjust to these changes and focus on disease management. Conversely, if we believe in the potential of antiaging medicine and treatments and protocols that slow or eliminate many manifestations of aging (eg, statins and aspirin), we will likely approach these individuals differently.