Learning objectives
- •
Osteoporosis is a silent, asymptomatic disease until a fracture is sustained.
- •
Fragility fractures are diagnostic of osteoporosis, regardless of densitometric findings, but after excluding localized bone diseases.
- •
All fractures sustained, regardless of whether they are fragility or nonfragility fractures, increase the risk of subsequent fractures.
- •
Most fractures are preceded by a fall, but most falls do not result in fractures.
- •
The usefulness and limitations of hip protectors.
The case study
Reason for seeking medical help
- •
MT, 69 years old, sustained a right hip fragility fracture after tripping over her granddaughter’s toy in the bedroom and falling on the carpet. She underwent surgery and recovered well.
Past medical and surgical history
- •
No relevant past medical or surgical history, no history of fractures, falls, or renal calculi.
- •
Natural menopause at age 50 years, no hormonal replacement therapy.
- •
Menarche at age 13 years, regular menstrual periods.
- •
Three children aged 38, 36, and 29 years, all in good health.
Lifestyle
- •
Active physical lifestyle: works as a part-time dietitian in a nursing home.
- •
For most of her adult life, she has been swimming at least 1 h a day, 5 days a week.
- •
Good appetite, states that she eats a well-balanced diet, and her daily calcium intake is “good.”
- •
No cigarette smoking, no excessive sodium intake, two cups of hot black tea with milk, and one cup of coffee with milk daily. No soda drinks.
Medications
- •
None.
Family history
- •
Negative for osteoporosis, fractures, and renal calculi.
Clinical examination
- •
Weight 130 pounds, height 66″, no height loss and no kyphosis.
- •
No significant clinical findings: alert, oriented, appears cognitively intact. No clinical evidence of orthostatic hypotension: lying BP 124/72; standing BP 128/70, no arrhythmias, no carotid stenosis, no sensitive carotid sinus, no vertebrobasilar insufficiency, no arrhythmias, no involuntary movements, no evidence of localizing neurologic diseases. Good coordination of movements, cerebellar functions intact, tendon reflexes present, equal on both sides, plantar responses downgoing on both sides. No evidence of visual impairment.
Laboratory results
- •
MT recently had the following laboratory tests done as part of her annual physical examination: comprehensive metabolic panel (CMP), complete blood count (CBC), serum vitamin D, and serum thyroid stimulating hormone (TSH): all within normal limits.
DXA and/or radiologic results
- •
Plain X-ray: total right hip replacement, post right femoral neck fracture, good placement.
Multiple choice questions
- 1.
In MT’s case, the final complete diagnosis of her bone health status is:
- A.
Osteoporosis.
- B.
Status posthip fracture.
- C.
Osteoporosis, status posthip fracture.
- D.
Osteoporosis, status postfragility hip fracture.
- E.
Probable osteoporosis, status postfragility hip fracture.
Correct answer: D
Comment:
Fragility fractures are diagnostic of osteoporosis even in the absence of densitometric evidence of osteoporosis, provided other metabolic bone diseases have been excluded. MT has sustained a fragility hip fracture, i.e., a fracture that occurred in the absence of significant trauma: she tripped over her granddaughter’s toy and fell on the carpet. The magnitude of this trauma is not expected to result in a fracture in most healthy people. The final diagnosis of MT’s bone status is therefore “osteoporosis, status postfragility right hip fracture” or “established osteoporosis.” There is no need for further diagnostic tests, including a DXA scan, to confirm the diagnosis of osteoporosis. A DXA scan, however, is needed to establish the patient’s baseline bone mineral density and evaluate her response (or lack thereof) to any prescribed medication.
Once a fragility fracture has occurred the risk of subsequent fragility fractures is substantially increased, hence the importance of including the term: “fragility fracture” with the diagnosis. A study conducted on 377,561 female Medicare beneficiaries who sustained a fracture shows that the cumulative risk of subsequent fractures was 10%, 18%, and 31% at 1, 2, and 5 years postindex fracture, respectively. The risk of subsequent fractures is increased even in patients who sustain traumatic fractures.
There is, therefore, some urgency to initiate medical management for osteoporosis in these patients, especially as medications are now available to significantly reduce the risk of patients sustaining further fragility fractures. Conversely, the longer the patient is left untreated, the more likely she is to sustain another fragility or traumatic fracture.
Fragility fractures occur most commonly in the vertebrae and are also diagnostic of osteoporosis after excluding secondary causes of localized osteoporosis. There are 2 types of vertebral compression fractures:
- (a)
“Clinical vertebral compression fractures” are usually associated with severe disabling pain of sudden onset. These are discussed in a separate case.
- (b)
Silent vertebral compression fractures are also referred to as “morphometric vertebral compression fractures.” Unlike clinical vertebral compression fractures they are not associated with severe pain and are often asymptomatic, accidentally discovered while performing imaging studies for some other reason. The main clinical manifestations are loss of height, arm span exceeding body height, kyphosis, a reduced space between the lower ribs and pelvic cavity, and a protuberant abdomen. In severe cases the lower ribs lie close to and may overlap the pelvic bones. Morphologic vertebral compression fractures are discussed in a separate case.
- A.
- 2.
Match the following:
- i.
Fragility fractures.
- ii.
Pathologic fractures.
- iii.
Traumatic fractures.
- iv.
i and ii.
- v.
All of the above.
With:
- A.
Associated with a relatively good prognosis.
- B.
Associated with a poor prognosis.
- C.
Have a bimodal age distribution: common among young and older patients.
- D.
The result of trauma that would not be expected to result in a fracture.
- E.
Associated with an increased risk of further fractures
Correct answers: A. iii; B. iv; C. iii; D. iv; E. v
Comment:
There are essentially four main types of fractures:
- (a)
Posttrauma fractures .
These fractures are the result of the fractured bone having been subjected to significant mechanical trauma. The trauma is of such magnitude that it disrupts the mechanical structural integrity of the bone and results in a fracture. Any bone exposed to such trauma, even a “normal” bone, is likely to fracture. However, as mentioned earlier, once a fracture is sustained, other fractures are likely to occur subsequently.
Traumatic fractures have a bimodal distribution: more common in younger and older individuals. Whereas the prognosis is good in younger individuals, it is often poor in older patients, probably because of other underlying pathologies.
- (b)
Fragility fractures.
These fractures, also known as low trauma, atraumatic, low impact, or low energy fractures, are the result of the inherent physical mechanical weakness of osteoporotic bones. The bones are structurally impaired, mechanically weak, and unable to maintain their mechanical integrity: they fracture after sustaining minimal trauma that ordinarily would not be expected to lead to a fracture. Fragility fractures also may occur spontaneously, in the absence of trauma: atraumatic fractures.
In an attempt to standardize the definition of fragility fractures, they have been defined as fractures occurring after a fall from a height that does not exceed the body height such as occurs when the patient is walking and trips over an object that she had not seen. There is nevertheless controversy as to the impact of falling on a carpeted versus noncarpeted area, on the pavement as opposed to a wooden floor, and falling in a frozen outdoors parking spot as opposed to inside a garage.
Fragility fractures also can occur while the patient tries to get out of a chair or turns around while standing: the torque force exerted on the upper femur may be of sufficient magnitude to induce a fracture. In severe cases, they may occur while the patient is lifted out of her bed or is turned in bed by attendants.
- (c)
Pathologic fractures.
Pathologic fractures are the result of an underlying localized bone pathology such as multiple myeloma or neoplastic deposits that may interfere with the integrity of the bone and may be responsible for the fracture.
- (d)
Fissure or insufficiency fractures .
Stress fissure fractures extend from one surface into the bone, but not through it, unless displaced. They are often the result of an excessive workload on the bone as may occur when a person who has been leading a sedentary lifestyle decides—without adequate preparation—to undertake taxing physical exercises. These fractures are often referred to as stress fractures and are discussed in a separate case study.
- i.
- 3.
Factors predisposing to osteoporosis in MT’s case include:
- A.
Status postnatural menopause.
- B.
No postmenopause hormonal replacement therapy.
- C.
Caucasian ethnicity.
- D.
A and B.
- E.
A, B, and C.
Correct answer: E
Comment:
The menopause is a major factor predisposing to a reduced bone mass, increased bone fragility, and osteoporosis. The cessation of estrogen production at the menopause is associated with an increased rate of bone resorption. As the rate of bone formation is not increased, the bone mass tends to decrease, and the patient develops osteoporosis.
Osteoporosis is essentially asymptomatic until a fragility fracture occurs. Unfortunately by this time, the bone mass is significantly reduced, and once the patient develops a fragility fracture, she is more likely to sustain other fragility fractures. The National Bone Health Alliance Working Group recommends postmenopausal women and men aged 50 years and older be treated for osteoporosis if their 10-year fracture risk is or exceeds 3% for the hip or 20% (major) fracture . This issue is further discussed in a different section.
- A.
- 4.
Factors reducing the likelihood that MT has osteoporosis include:
- A.
She has been swimming about an hour, 5 days a week for most of her adult life.
- B.
Her stated daily calcium intake exceeds the minimum recommended daily allowance.
- C.
She does not smoke cigarettes.
- D.
A and C.
- E.
A, B, and C.
Correct answer: C
Comment:
Cigarette smoking increases the risk of developing osteoporosis. Unlike most physical exercises, however, swimming has not been shown to significantly increase the bone mineral density. Patients also often overestimate their daily calcium intake, and it is important to inquire in detail about the source and amount of their calcium intake. On further questioning, MT stated that her main source of calcium intake is a 4-oz cup of yogurt (150 mg) she often has for breakfast with some fresh fruit. She also has some milk with her cup of coffee mid-morning and a cup of tea, also with milk, in the afternoon. She does not like cheese. Clearly, her daily calcium intake is well below the 1200 mg daily recommended. The calcium content of select foods is listed separately.
- A.
- 5.
The following is correct:
- A.
Most fragility fractures are preceded by falls.
- B.
Most falls are followed by fractures.
- C.
Once a patient has sustained a fracture, the risk of subsequent fractures is increased.
- D.
A and C.
- E.
A, B, and C.
Correct answer: D
Comment:
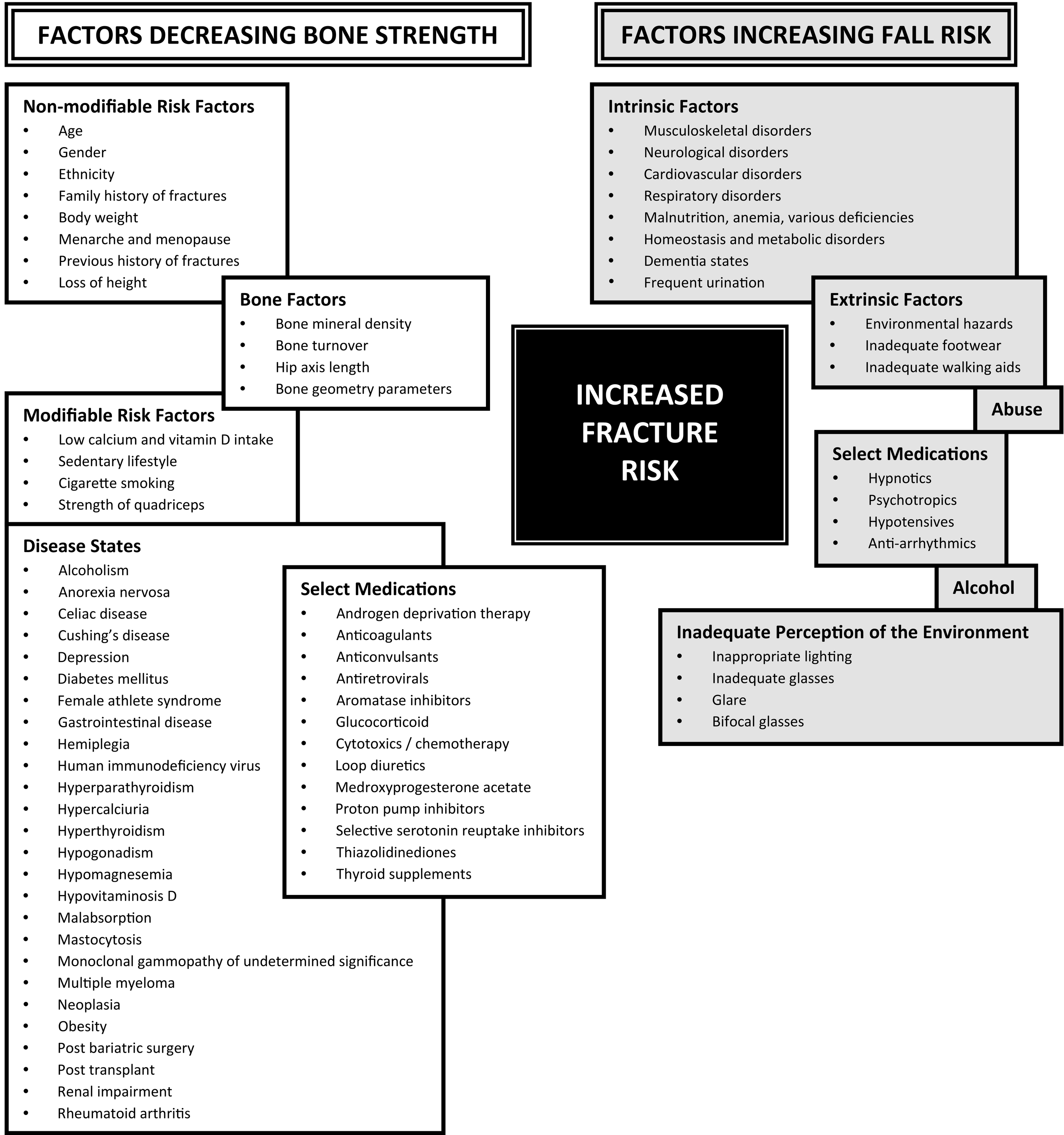
Although some fragility fractures occur spontaneously, in the absence of any type of trauma, most fractures are preceded by falls. Fortunately, most falls are not preceded by fractures. This gives clinicians a unique opportunity to reduce the risk of fractures, especially fragility fractures, by identifying patients likely to sustain falls, identifying the causes of the falls and managing them, prior to the patient sustaining another fall. Susceptibility to falls should be an integral part of the evaluation of patients for osteoporosis, especially older patients. About one-third of community-dwelling people 65 years of age and older experience repeated falls; many more experience near falls, which are precursors of falls. Falls and fractures are discussed in separate case studies.
- A.
- 6.
Causes of repeated falls in older people include:
- A.
Intrinsic causes, such as diseases interfering with posture, balance, and steadiness.
- B.
Extrinsic causes—hazardous environment.
- C.
Inadequate perception of the environment.
- D.
Impaired cognitive functions.
- E.
All of the above.
Correct answer: E
Comments:
Causes of falls can be grouped into four different groups: First, falls resulting from some pathology such as orthostatic hypotension, arrhythmias, peripheral neuropathy, Parkinson’s disease, and inappropriate foot wear. Second, falls due to a hazardous environment as is the case with the present patient who tripped on her grandchild’s toy. Visual impairment may also aggravate the hazardous environment. Third, a number of medications, and alcoholic drinks, may increase the risk of falls by inducing unsteadiness. Fourth, cognitive impairment also may cause the patient to engage in potentially hazardous activities that may result in a fall. Abuse also can be an underlying cause of falls, albeit a difficult one to address. Signs of abuse include bruises of various ages, especially on the medial aspects of the humerus. Anxiety and depression are also likely to induce unsteadiness and repeated falls.
- A.
- 7.
Intrinsic causes of falls include:
- A.
Diabetes mellitus.
- B.
Arrhythmias.
- C.
Vertebrobasilar insufficiency.
- D.
Foot problems.
- E.
All of the above.
Correct answer: E
Comments:
Several intrinsic factors increase the fall risk of patients with diabetes mellitus, including the associated polyuria, frequent trips to the toilet, peripheral neuropathy, and autonomic neuropathy which may lead to orthostatic hypotension. Visual acuity is also often impaired in older patients with diabetes mellitus. Arrhythmias, by reducing the stroke volume and cardiac output, may lead to unsteadiness and a fall. Similarly, vertebrobasilar insufficiency, as seen sometimes in patients with cervical spondylosis, increases the risk of unsteadiness and falls especially when the patient turns her head and further increases the magnitude of vertebrobasilar insufficiency and cerebellar ischemia. A number of foot problems and inappropriate footwear may interfere with balance and increase the risk of falls. Common intrinsic causes of falls are listed in a different case study.
- A.
- 8.
Extrinsic causes of repeated falls in older people include:
- A.
Inadequate lightning.
- B.
Small decorative rugs and clutter.
- C.
Bifocal eye glasses.
- D.
A and C.
- E.
A, B, and C.
Correct answer: E
Comments:
Often environmental factors, extrinsic to the patient, are responsible for falls. This may occur when the patient relocates to a new environment or spends one or more nights in an unfamiliar surrounding as often happens when the patient stays a couple of days with her son and family or is transferred to a nursing home or other living accommodation. Not being familiar with the layout, the patient may trip over trailing electric wires or various objects she had not seen, as has occurred in the present case study.
Inadequate lightning and glare can interfere with visual acuity and may lead to repeated falls. Similarly, bifocal lenses may lead to repeated falls because the lower part of the lens which is meant to sharpen near vision is the part used to visualize the area immediately around the feet and the patient may not be able to clearly visualize obstacles or irregularities in the carpet or a small rug. As a general rule, especially for older people, it is best to have two sets of eyeglasses: one for reading and near vision and another for distant vision.
Older people are often fond of keeping small decorative rugs at the foot of the bed, entrance to rooms, and on paths they use to go from one place in their living accommodation to another. Often these small rugs are frayed and the older person may trip over such obstacles. Inadequate footwear also may lead to imbalance, unsteadiness, and repeated falls.
Common extrinsic causes of falls are discussed further in different case studies.
- A.
- 9.
Main medications increasing the risk of falls include:
- A.
Hypnotics.
- B.
Anxiolytics.
- C.
Hypotensives.
- D.
A and B.
- E.
A, B, and C.
Correct answer: E
Comment:
A number of medications may lead to repeated falls especially medications that cloud the sensorium or induce drowsiness. Hypnotics, including over-the-counter hypnotics obtained without prescription, are particularly likely to induce repeated falls as they have a longer half-life than most prescription hypnotics. To complicate matters, it is not uncommon for patients to refrain from telling their treating clinician that they are taking over-the-counter hypnotics.
Anxiolytics increase the risk of falls by a similar mechanism as hypnotics. Hypotensives also may induce falls by reducing the cardiac output and cerebral blood flow, especially if the patient also has orthostasis. In older hypertensive patients the optimum blood pressure is usually higher than in the younger population. Alcoholic drinks also increase the risk of falls by interfering with the patient’s sensorium, steadiness, and executive functions.
- A.
- 10.
Hip protectors:
- A.
Significantly reduce the risk of hip fractures.
- B.
Patients often forget to wear them.
- C.
Patients do not like to wear them.
- D.
A, B, and C.
- E.
B and C.
Correct answer: D
Comments:
Hip protectors reduce the risk of hip fractures, provided the patient wears them. Nowadays most hip protectors are relatively small, nonintrusive, comfortable to wear, and not allergenic. Patients nevertheless need to be reminded that hip protectors are effective only if they are worn.
Unfortunately, most patients tend to take the hip protector off while getting ready to go to bed. When they wake up some time later, because of an urge to empty their urinary bladder, they tend to postpone getting out of bed until such a time that the urge to micturate becomes quite significant. At this stage, they quickly get up out of bed and try to reach the toilet as rapidly as possible. In the process they forget the wear the hip protector, may develop orthostatic hypotension, fall on their way to the toilet, and sustain a fragility fracture.
Patients need to be reminded to get out of bed slowly and ideally sit on the bed for a few seconds while transitioning from the supine to the standing position to ensure they do not become orthostatic before walking to the toilet. They also should allow sometime to put the hip protector. Alternatively, they may elect to wear the hip protector all day and night.
- A.
Case summary
Analysis of data
Factors predisposing to bone demineralization/osteoporosis
- •
Caucasian ethnicity.
- •
Status postmenopause, no hormonal replacement therapy.
- •
Low daily calcium intake, even though MT, a certified dietician, states that she is getting an adequate amount of calcium through her diet.
Factors reducing the risk of bone demineralization/osteoporosis
- •
Negative family history of osteoporosis.
- •
Physically active lifestyle.
- •
Well balanced diet, except for the low calcium intake.
- •
No cigarette smoking.
- •
No excessive alcohol, sodium, or caffeine intake.
Factors increasing risk of falls/fractures
- •
Objects inadvertently placed in the patient’s path: MT tripped over her granddaughter’s toy which had been inadvertently left on the carpet in her path.
Factors reducing the risk of falls/fractures
- •
Good cognitive functions.
- •
Physically active life style.
Diagnosis
- •
Osteoporosis, status postfragility hip fracture.
Management recommendations
Treatment(s)
- •
Antiresorptive or osteoanabolic medication. This is discussed in other cases.
- •
Calcium supplements if the patient is unable to get minimum recommended daily calcium intake from food: 1200 mg daily for women 50 years old and older and men 70 years old and older.
Diagnostic test(s)
- •
No laboratory tests needed at this stage. MT had a few laboratory tests done recently.
- •
Baseline DXA scan, not needed to establish the diagnosis, but needed to evaluate response to treatment.
Lifestyle
- •
Encourage the patient to walk and undertake light weight-bearing exercises at least three times a week to increase bone mass and also muscle mass. Caution must be taken not to put too much stress on the rest of the skeleton. Free weight exercises should be avoided because of the risk of self-injury.
- •
Follow-up office visit depending on the medication prescribed for osteoporosis.
Rehabilitation
- •
Physical therapy and, if need be, occupational therapy to ensure patient is physically independent.
DXA and radiological
- •
Repeat DXA scan in 2 years’ time to evaluate the bone mass and effect of prescribed therapy ( Fig. 1 ).