Learning objectives
- •
Fragility vertebral fractures are diagnostic of osteoporosis.
- •
The presentation and management of acute symptomatic (clinical) and asymptomatic (morphometric) vertebral compression fractures are different.
- •
The usefulness and limitations of vertebral augmentation procedures.
The case study
Reason for seeking medical help
- •
CD presents with sudden onset of severe constant mid-back pain, with no radiation. She ranks the pain as 8 on a scale of 1–10. It started spontaneously 4 days ago while watching TV, is resistant to acetaminophen and ibuprofen, and only partly relieved by lying down, local heat, and hydrocodone/acetaminophen tablets. She has not noticed any localized muscle weakness or sensory deficit. She is ambulant, continent of urine, and has good sphincteric control. She appears to be cognitively intact.
Past medical and surgical history
- •
Natural menopause at age 48 years, no hormonal replacement therapy.
- •
Lost about 2 in. in height since her early forties.
- •
Bilateral hip replacement because of osteoarthritis.
Lifestyle
- •
Daily dietary calcium intake about 1200 mg.
- •
No excessive sodium or caffeine intake.
- •
No cigarette smoking.
- •
No alcoholic drinks.
- •
Sedentary lifestyle.
Medication(s)
- •
Hydrocodone/acetaminophen tablets as required every 4 h, started 3 days ago. She is, however, reluctant to continue taking this medication as she is concerned about habituation and addiction.
- •
Multiple vitamins/minerals supplement.
Family history
- •
Mother sustained fragility hip fracture.
Clinical examination
- •
Cognitively intact.
- •
Moderate kyphosis.
- •
Weight 132 pounds, height 60″, during early adulthood she was about 65″.
- •
Point tenderness on the vertebral spines in the lower thoracic vertebrae region and localized adjacent paravertebral muscle spasms.
- •
Limited range of motion of lumbar vertebrae because of pain.
- •
No localizing neurological lesions.
Multiple choice questions
- 1.
In CD’s case, the clinical presentation is suggestive of:
- A.
Intervertebral disc prolapse.
- B.
Paget’s disease of bone.
- C.
Vertebral compression fracture (VCF).
- D.
All the above.
- E.
None of the above.
Correct answer: C
Comment:
The clinical presentation is characteristic of a fragility vertebral compression fracture (VCF): it occurred suddenly; in the absence of trauma; is severe, localized, and associated with point tenderness on the vertebral spines and adjacent paravertebral muscle spasm.
Sometimes osteoporotic VCFs are precipitated by trying to lift or push a heavy object and need to be differentiated from prolapsed intervertebral discs. The loss of height and kyphosis are suggestive of VCFs. The pain associated with disc prolapse often radiates to the legs, while that associated with Paget’s disease of bone is usually low grade and worse when the patient lies in a warm bed.
- A.
- 2.
Fragility vertebral compression fractures (VCF):
- A.
Most are asymptomatic.
- B.
Are diagnostic of osteoporosis regardless of the T-scores.
- C.
Are associated with significant mortality and morbidity.
- D.
B and C.
- E.
A, B, and C.
Correct answer: D
Comment:
Fragility fractures occur most commonly in the vertebrae and are also diagnostic of osteoporosis after excluding secondary causes of localized osteoporosis. There are two types of vertebral compression fractures:
- (a)
“Clinical vertebral compression fractures” are associated with sudden onset of severe, often disabling pain.
- (b)
“Silent vertebral compression fractures” are also referred to as “morphometric vertebral compression fractures.” Unlike clinical vertebral compression fractures, they are not associated with severe pain and are often totally asymptomatic, accidentally discovered while performing imaging studies for some other reason.
The main clinical manifestations are loss of height, arm span exceeding body height, kyphosis, a reduced space between the lower ribs and pelvic cavity, and a protuberant abdomen.
Diagnosing osteoporosis on the basis of discovering one (or more) vertebral compression fracture while the patient is being investigated for a different pathology is often referred to as an “opportunistic” diagnosis of osteoporosis.
- A.
- 3.
Vertebral Fracture Assessment (VFA) by bone densitometry:
- A.
Visualizes the vertebrae laterally between T8 and S1.
- B.
The lateral contour of each vertebra can be visualized.
- C.
Is useful to diagnose VCFs.
- D.
A, B, and C.
- E.
B and C.
Correct answer: E
Comment:
VFA allows visualization of the thoracolumbar vertebrae, usually from T4 to the sacrum. The contour of each vertebra can be clearly visualized by altering the brightness and contrast of the screen. VFA is useful to determine the type (wedge, biconcave, or crush) and degree (mild, moderate, and severe) of VCFs either visually or by using markers to highlight the anterior, posterior, and midpoint heights of suspected vertebrae: a difference of 20% or more between these heights is diagnostic of VCF. Osteoporosis, however, still remains underdiagnosed and undertreated even though its diagnosis now is relatively simple and effective and relatively safe medications are available. Osteoporosis is a major public health issue.
A number of guidelines are also available to help clinicians develop a therapeutic management strategy tailored to the needs and status of the individual patient.
- A.
- 4.
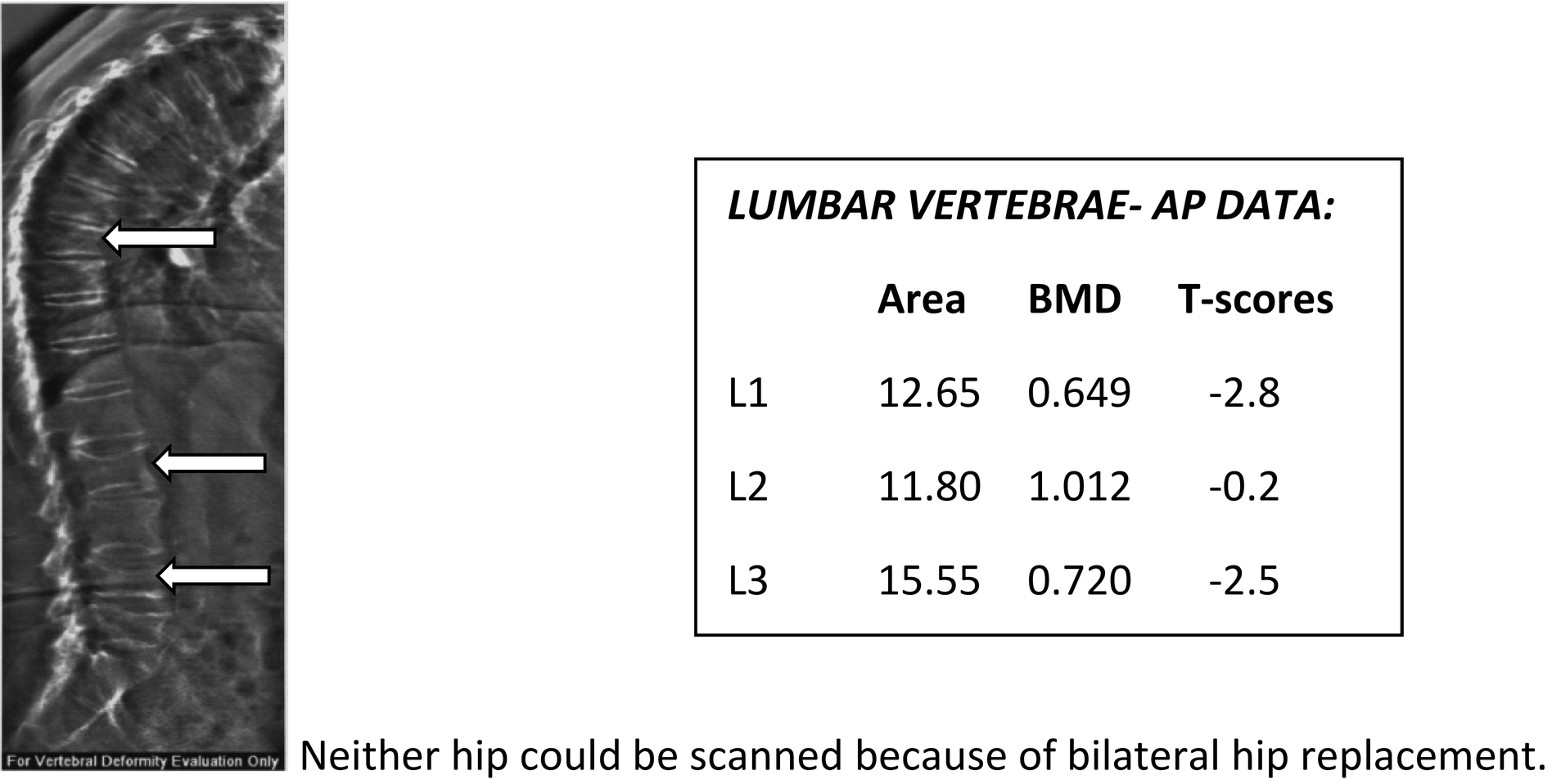
CD’s DXA and VFA scans:
- A.
L1-L4 T-score is normal.
- B.
L1-L4 T-score is artificially elevated because of VCFs.
- C.
Suggestive of L2, L4, and T9 vertebral compression fractures.
- D.
L2 and L4 should be excluded from the final analysis.
- E.
B, C, and D.
Correct answer: E
Comment:
Densitometric evidence of VCFs includes a smaller surface area of the affected vertebra compared to the vertebra immediately above, a higher BMD compared to the vertebra immediately below, and a difference in T-scores of more than 1.0 when compared to the adjacent vertebrae.
Normally the surface area and BMD of each vertebra increase from L1 to L4. When a vertebra is compressed, its surface area is reduced, and as the bone mineral content remains unchanged, its density appears to be higher than the vertebra below. Compressed vertebrae should be excluded before analyzing the scan. There nevertheless should be at least 2 evaluable vertebrae.
- A.
- 5.
The following can be useful to relieve pain associated with VCFs:
- A.
Analgesics and nonsteroidal antiinflammatory drugs.
- B.
Narcotics.
- C.
Calcitonin.
- D.
Any of the above.
- E.
None of the above.
Correct answer: D
Comment:
Pain management is the prime goal of managing patients with acute symptomatic VCFs to avoid triggering a vicious cycle: pain leading to reduced physical activity, muscle wasting, unsteadiness, and increased risk of falls and subsequently fractures. All the listed modalities are useful to reduce pain associated with VCFs. The analgesic effect of calcitonin is mediated through endorphins.
Narcotics may be indicated. There is, however, evidence to suggest that the addition of codeine to a combination of acetaminophen and ibuprofen does not increase the analgesic potency of the latter as evidenced by a randomized double-blind controlled trial on 131 subjects undergoing surgical removal of an impacted third molar tooth. Pain was assessed by a visual analogue scale. Another randomized controlled trial on 416 patients presenting to emergency departments with acute extremity pain showed neither statistically nor clinically significant differences in pain reduction 2 h after a single dose treatment with one of 4 regimens: ibuprofen and acetaminophen, oxycodone and acetaminophen, hydrocodone and acetaminophen, or codeine and acetaminophen.
Notwithstanding, as the pain associated with an acute VCF is usually, spontaneously, at least partly, relieved within 4–6 weeks of the fracture, it is seldom necessary to continue with narcotics for longer periods. The adverse effects of narcotics, especially in older people, are well known and include cognitive impairment, delirium, depression, constipation, unsteadiness, repeated falls, accidents, injuries, peripheral edema, respiratory depression, hypoventilation, apnea, hypoxia, somnolence, nausea, vomiting, dizziness, pruritus, urine retention, and urinary incontinence.
- A.
- 6.
The following are useful modalities to relieve pain associated with VCFs:
- A.
Back braces.
- B.
Transcutaneous nerve stimulation.
- C.
Gentle massage and heat application.
- D.
All the above.
- E.
None of the above.
Correct answer: D
Comment:
Back braces are often effective at alleviating the pain. However, by providing support they reduce muscle tone and may lead to muscle wasting if worn for prolonged periods. Most patients like back braces because of the support and comfort they provide.
Transcutaneous nerve stimulation is effective at reducing the pain. Gentle superficial massage (effleurage), local heat, and menthol-based or lidocaine ointments are soothing adjunct comforting measures. A number of plant-based ointments are also commercially available over the counter. Their evidence-based efficacy has not been thoroughly evaluated. Deep massage is better avoided as it may jeopardize the fragile integrity of the vertebrae.
- A.
- 7.
Match the following:
- (a)
Acetaminophen.
- (b)
Nonsteroidal antiinflammatory medications.
- (c)
Narcotics.
- (d)
All the above.
- (e)
None of the above.
- A.
Nephrotoxicity.
- B.
Hepatic toxicity.
- C.
Constipation.
- D.
Increased fall risk.
- E.
Upper GI adverse effects.
- A.
Correct answers: A (b); B (a); C (c); D (c); E (b)
Comments:
Constipation, impaired cognitive functions, drowsiness, and repeated falls are the main adverse effects of narcotics in older patients. Gastric irritation and upper gastrointestinal irritation are often seen in patients taking nonsteroidal antiinflammatory drugs. NSAIDs also should be avoided or administered in reduced doses, and for short periods of time to patients with impaired renal functions. The need for analgesia should be regularly evaluated as the pain is often limited to 4–6 weeks after the fracture is sustained.
- (a)
- 8.
Match the following:
- (a)
Kyphoplasty.
- (b)
Vertebroplasty.
- (c)
Both.
- (d)
Neither.
- A.
A cavity is created in the compressed vertebral body.
- B.
Biological cement is injected under high pressure into affected vertebra.
- C.
If successful it is usually associated with almost immediate complete pain relief.
- D.
Activities of daily living can be resumed almost immediately after the procedure.
- E.
The risks of biological cement extravasation are higher.
- A.
Correct answers: A: (a); B: (b); C: (c); D: (c); E: (b)
Comment:
Kyphoplasty and vertebroplasty are vertebral augmentation procedures during which biological cement (usually polymethylmethacrylate) is introduced in the compressed vertebral body. During vertebroplasty, the cement is introduced under high pressure. During kyphoplasty, a cavity is first created in the vertebral body by a balloon tamp and then cement is introduced under low pressure into that cavity. The pressure required to administer biological cement is lower with kyphoplasty than with vertebroplasty and therefore the risk of extravasation is less. Kyphoplasty may restore some height loss. When successful, these procedures are associated with almost immediate pain relief with the patient able to resume her daily activities.
- (a)
- 9.
The following is/are true concerning vertebral augmentation procedures:
- A.
Long-term pain relief is well established.
- B.
Success rate is higher if done soon after the fracture occurred.
- C.
Risk of adjacent VCFs is significantly higher after the procedure.
- D.
A and B.
- E.
A, B, and C.
Correct answer: B
Comments:
Whereas, when successful, the acute pain relief is almost immediate and remarkable, the long-term pain relief of vertebral augmentation procedures is still questionable. The success rate, however, is higher if the procedure is done soon after the fracture.
A concern about injecting biological cement in a compressed vertebra is the increased mechanical stress on adjacent vertebrae and increased risk of adjacent vertebral fractures and biological cement extravasation. On the other hand, the mechanical stress imposed by a compressed vertebra on the adjacent vertebrae and the inherent increased fragility of adjacent vertebrae also must be considered.
The two main indications for vertebral augmentation procedures are: first, pain relief and improvement of the patient’s functional status; and second, vertebral body stabilization. As in most patients, the pain improves spontaneously; the effects of vertebral augmentation, per se, on pain are difficult to assess.
Notwithstanding, neither vertebroplasty, nor kyphoplasty is at present recommended as first-line treatment in patients with painful vertebral compression fractures because of the unclear benefit on pain and the potential increased risk of fractures developing in adjacent vertebrae.
- A.
- 10.
The goals of vertebral augmentation procedures include:
- A.
Pain control.
- B.
Improving the patient’s functional status.
- C.
Vertebral body stabilization.
- D.
A and B.
- E.
A, B, and C.
Correct answer: E
Comments:
Vertebral augmentation is an image-guided, minimally invasive procedure during which bone cement, such as polymethylmethacrylate, is injected in the compressed vertebra to manage painful fractures not responding to conservative medical therapy. Secondary goals include stabilizing the affected vertebral body and preventing future fractures.
- A.
Case summary
Analysis of data
Factors predisposing to bone demineralization/osteoporosis in CD’s case
- •
Status postmenopause, no HRT.
- •
Positive family history: mother sustained fragility hip fracture.
- •
Sedentary lifestyle.
- •
Caucasian race.
Factors reducing risk of bone demineralization/osteoporosis in CD’s case
- •
Good daily calcium intake.
- •
No excessive sodium, caffeine, alcohol intake and no cigarette smoking.
Factors increasing risk of falls/fractures
- •
Vertebral compression fracture.
- •
Height loss and kyphosis.
- •
Intake of narcotics.
Factors reducing risk of falls/fractures
- •
None.
Diagnosis
- •
Osteoporosis, acute vertebral compression fracture.
Management recommendations
Treatment recommendation(s)
- •
Antiresorptive or osteoanabolic therapy for osteoporosis.
- •
Pain control.
Diagnostic test(s)
- •
Rule out secondary causes of osteoporosis and osteolytic deposits.
Rehabilitation
- •
Vertebral augmentation procedures may be considered in some select patients.





