| Order | Exanthems | Agent |
|---|---|---|
| First | Rubeola or measles | Measles virus |
| Second | Scarlet fever | Streptococcal toxin |
| Third | Rubella or German measles | Rubella virus |
| Fourth | Filatov–Dukes’ disease | Unknown, possibly strep. or staph. toxin |
| Fifth | Erythema infectiosum | Parvovirus |
| Sixth | Exanthem subitum or roseola | Human herpesvirus 6 |
Rubeola (measles)
Epidemiology and virology
Global measles-related deaths have declined markedly. However, despite impressive improvements in our understanding of infectious diseases such as rubeola (measles) and the widespread availability of effective vaccine, vaccination is far from universal and outbreaks have been reported in recent years from the developing world to the suburbs of US cities. In addition, seroprevalence in newly arrived refugee children to the United States is relatively low, with only 82% having protective antibody to measles in a recent analysis, raising the possibility of transmission of wild-type virus within these populations. Investigations of recent outbreaks found that the majority of measles cases occurred in unvaccinated people, highlighting gaps in vaccine coverage as an important risk factor. Given recent outbreaks of rubeola in the United States, a high degree of vigilance and early recognition of clinical presentations is of ongoing importance among providers.
Rubeola is caused by an RNA virus with one serotype and is classified in the genus Morbillivirus in the Paramyxoviridae family. Most cases of measles occur in the late winter or spring. Humans are the only natural hosts and transmission occurs by exposure to infectious droplets. Rubeola is one of the most highly contagious of the infectious agents. Appropriate isolation of cases in hospital settings is critical to limit nosocomial transmission. A patient hospitalized with measles requires airborne precautions for 4 days after the onset of rash. However, if the patient with measles is immunosuppressed, airborne precautions are required until the illness completely resolves. The measles virus is labile and survives only a short time on fomites. The highest rates of transmission occur in the home, day-care centers, nursery schools, primary and secondary schools, colleges, and universities. School outbreaks can occur despite greater than 95% immunity among students.
Clinical and laboratory diagnosis
Clinical measles demonstrates a fairly characteristic clinical presentation. However, given a dramatically lower incidence of illness in recent years, many contemporary providers have not seen a classic measles infection, so diagnosis may not be straightforward. In addition, presentation may be atypical in immunocompromised patients.
The incubation period is 10 to 12 days. There is a prodrome of low-grade fever, malaise, and headache. This is followed or accompanied by cough, coryza, and conjunctivitis. During the prodrome, an enanthem appears on the buccal mucosa, and may spread to the hard or soft palate. The typical enanthem of measles (Koplik spots) consists of punctate white or gray lesions described as grains of sand on erythematous bases. As the infection evolves, the number of Koplik spots increases and lesions coalesce. These resolve with the onset of the rash. After about 4 days of increasing prodromal symptoms, the patient develops high fever and rash. The rash (Figure 19.1) begins as erythematous macules and papules at the hairline, on the forehead, behind the ears, and on the upper neck. This characteristic morbilliform rash occurs in the large majority of normal individuals. The rash spreads centrifugally to the trunk and extremities over the next 3 days. This erythematous rash blanches on pressure and may coalesce, and when it resolves, it may leave brownish hyperpigmentation that results from capillary hemorrhage. The rash may not occur at all, or could be severe in patients who are immunosuppressed. When present, the high fever and rash persist for 2 to 4 days. As the rash fades, the coryza and conjunctivitis clear, but the cough may persist for another 5 days. Immunocompetent patients are contagious from the onset of the prodrome until approximately 4 days after the onset of the rash.
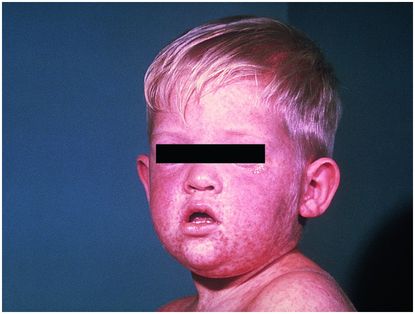
Figure 19.1 Measles in a 9-year-old child presenting as morbilliform lesions on the face, trunk, and palms.
The most common complications of measles are secondary bacterial infections, including pneumonia and otitis media. Diarrhea may also occur as a complication. The risk of complications is highest for infants younger than 1 year of age. Postinfectious encephalomyelitis occurs in approximately 1 per 1000 measles cases within a few days of rash onset. Most patients recover but many have persistent developmental sequelae. Acute disseminated encephalomyelitis (ADEM) is a demyelinating disease that occurs later, within 2 weeks of recovery. Also called postinfectious or postvaccine encephalomyelitis, ADEM may be related to an autoimmune response and carries a 10% to 20% mortality, with survivors commonly suffering neurologic sequelae. In contrast, subacute sclerosing panencephalitis (SSPE) occurs several years (classically 7–10) after natural infection, and carries a very high mortality. This complication has become exceedingly rare with the dramatic decrease in measles cases over the past few decades due to immunization.
Measles can be confirmed by viral cultures of the nasopharynx, conjunctiva, blood, or urine. However, culture is technically difficult and not readily available. Sera may be obtained for measles antibody determinations both at the onset of the rash and 2 to 4 weeks later. A significant increase of measles immunoglobulin (Ig)G antibody (acute and convalescent) is diagnostic. A measles-specific IgM antibody test is also available. This IgM antibody is detectable from about 3 to 30 days after the onset of the rash. Finally, isolation of measles virus RNA by polymerase chain reaction (PCR) from clinical specimens such as those listed above is diagnostic, but may only be available at state public health laboratories. Immunity after measles infection is lifelong, and a second attack is very rare.
Treatment and prevention
Treatment of measles is usually symptomatic; acetaminophen or a nonsteroidal anti-inflammatory drug (NSAID) is used for pain and fever. Oral vitamin A supplementation lessens morbidity and mortality in malnourished patients. For reasons that are not well defined, malnourished patients may suffer acute vitamin A deficiency when infected with measles. Vitamin A is necessary for the maintenance of epithelial integrity and for normal immune function. The World Health Organization (WHO) now recommends treatment with vitamin A supplementation once a day for 2 days for all children with acute measles; specific doses vary with age (200 000 IU for children 12 months and older; 100 000 IU for infants 6 to 11 months; 50 000 IU for infants under 6 months). Because measles may be complicated by secondary bacterial infection, prophylactic antibiotics are sometimes prescribed, although not generally recommended. The most common bacterial complication is pneumonia caused by Streptococcus pneumoniae, Haemophilus influenzae, or Staphylococcus aureus. Measles virus is susceptible in vitro to the antiviral agent ribavirin. However, ribavirin is not approved by the US Food and Drug Administration (FDA) for this indication. There are anecdotal reports of successful use of intravenous and/or aerosolized ribavirin to treat severely ill, immunosuppressed patients with measles.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





