Neil D. Gillespie, Miles D. Witham, Allan D. Struthers
Chronic Cardiac Failure
Cardiac failure increases in prevalence and incidence with age. It is a disease of middle and old age, although the underlying causes differ considerably with age. In younger patients with cardiac failure, the cause is frequently coronary artery disease or a cardiomyopathy of uncertain cause, whereas in the older patient, valvular disease and hypertension are more often implicated. Heart failure remains a severely debilitating condition for many older adults, but advances continue to be made in diagnosis, treatment, and organization of care. The challenge is to ensure that these advances can be translated to older adults with multiple comorbid diseases and to understand how best to deliver high-quality heart failure care to the frailest older adults.
The pool of patients at risk of heart failure continues to rise as more patients survive myocardial infarction as a result of percutaneous coronary intervention, thrombolytic therapy, and adjunctive drug treatment. In addition, patients with hypertension are surviving longer as a result of continued improvements in treatment, which includes the prevention of strokes. Fortunately, it appears that the effective treatment of hypertension may in fact prevent the onset of heart failure, even in the very old.1 However, as more older adults live to extremes of age, it is almost inevitable that if they survive long enough, they will develop some degree of heart failure, even if it is not diagnosed until they are very frail.2
When considering the epidemiology of heart failure, it is important to note that it is defined as the presence of symptoms and signs of cardiac decompensation, together with objective evidence of underlying structural heart disease. These are the definitions used by the European Society of Cardiology3 and the American Heart Association,4 who have similar consensus statements on the diagnosis and management of heart failure. These agreements are important because they have resulted in a more focused approach when considering precisely which disease entity is being treated in individual patients. In the United Kingdom, the National Institute for Healthcare Excellence (NICE) guidelines give additional advice about treatment and, in Scotland, the Scottish Intercollegiate Guideline Network (SIGN) provides evidence-based advice. In this chapter, however, we will also consider issues particularly relevant to older adults and consider some of the very real challenges faced when managing older adults who are frail and often have many additional medical problems, as well as heart failure.
Heart failure is of major economic significance; in the United Kingdom, it accounts for up to 5% of hospital admissions, and across the world hospitalization for heart failure is a significant financial burden.5 Many older adults with heart failure also have multiple pathologies and coexistent diseases, including cognitive impairment, which can make the diagnosis more difficult.6
Epidemiology
The prevalence of heart failure rises with age, with this phenomenon seen in multiple cohorts, including the Framingham cohort,7 Scandinavian cohorts,8,9 and community-based screening cohorts.10 In the Framingham study, the prevalence of heart failure reached 10% in those older than 80 years; similar prevalence figures have been obtained from other cohorts.11 Echocardiographic screening studies suggest that as many of the population have asymptomatic left ventricular systolic dysfunction as have clinically overt heart failure.11 Many but not all cohort studies have suggested that the age-adjusted incidence of new heart failure diagnoses is rising over time12,13; this may reflect improved survival from ischemic heart disease and stroke, leading to a larger pool of at-risk individuals who then go on to develop clinically overt heart failure.
The proportion of heart failure patients with heart failure with reduced ejection fraction (HFREF) compared with those suffering from heart failure with reduced ejection fraction (HFPEF) changes with age.14 Younger patients (i.e., those < 65 years) suffer predominantly from HFREF and are predominantly men. In those older than 80 years, however, the number of women affected is similar to the number of men affected, driven in part by their greater longevity in most populations. In parallel, numbers with HFPEF are similar to numbers with HFREF in those older than 80 years.
Because frailty is linked to age, it can be expected that frailty and heart failure will often coexist, and this appears to be the case. In addition, frailty has been demonstrated to be a risk factor for heart failure15; it also seems likely, given elements of shared pathophysiology, that heart failure will make frailty worse.16
Disease Course and Prognosis
Heart failure has a variable prognosis, but despite improvements in survival with pharmacologic and device therapy, the prognosis remains worse than that of many major cancers.17 Key determinants of prognosis that are useful in clinical practice include ejection fraction, exercise capacity (as measured by maximal oxygen uptake or simpler tests such as the 6-minute walk test), symptoms (e.g., New York Heart Association [NYHA] class), renal impairment, and high natriuretic peptide levels.4 Patients admitted to hospital with acute decompensation of heart failure have a particularly poor prognosis, with high death rates in the 3 to 6 months after admission. Among older adults hospitalized with heart failure, mean survival is about 2.5 years.9 However, there is considerable heterogeneity in survival. The degree to which heart failure itself contributes to poor prognosis, rather than frailty or comorbid disease, can be difficult to discern, but the presence of chronic heart failure in older adults may result in an approximately 50% reduction in life expectancy.
Heart failure is a leading cause of hospitalization for older adults. Although there are data suggesting that heart failure as a primary cause of hospitalization is static or declining (possibly due to improved therapy), all-cause hospitalization for patients with heart failure continues to rise.12 Data from North America suggest that there is a high rate of readmission in heart failure patients, and it is noteworthy that readmissions are often not due to heart failure exacerbation.18 Evidence suggests that a multidisciplinary approach to the treatment of heart failure may reduce the need for hospitalization in older adult patients with the condition.19 Assessing factors that go beyond heart function is therefore critical in older adult patients, suggesting that elements of frailty assessment should inform heart failure management.20,21 Such an approach is crucial in the older adult patient for whom issues such as adherence to treatment plans, cognition, and continence figure prominently in the clinical decision making process.
The prognosis for heart failure, although improved in recent years by drug treatment, is nevertheless still poor. Most patients with NYHA Class IV disease (Table 39-1) will be unlikely to survive 1 year.
TABLE 39-1
New York Heart Association Classification of Heart Failure (HF)
| Class | Features |
| I | No symptoms |
| II | Symptoms with ordinary activity |
| III | Symptoms with less than ordinary activity |
| IV | Symptoms at rest |
A study of older men admitted as inpatients with heart failure revealed that the 1-year mortality was about 50%,22 although the mortality rate is reduced in those who survive for the first few months after hospitalization. Given this poor prognosis, alleviation of symptoms and improving daily function are as important as any potential mortality benefits for many older adult patients.23
Causes of Heart Failure
Heart failure has been described as a syndrome rather than a diagnosis or disease, and the underlying cause must always be sought in patients having the syndrome. HFREF is most frequently caused by ischemic heart disease, particularly previous myocardial infarction, although hypertension and diabetes also contribute to the cause. However, in older adult patients, valvular heart disease may cause left ventricular (LV) systolic dysfunction or exacerbate HFREF caused primarily by ischemic heart disease. Less frequently, HFREF in the older adult patient may be caused by one of the cardiomyopathies (e.g., viral or idiopathic), amyloidosis, storage diseases (e.g., hemochromatosis), secondary to chemotherapy (e.g., doxorubicin, trastuzumab [Herceptin]), or vitamin B deficiencies.
Furthermore, many patients have symptoms associated with heart failure in the presence of normal systolic function and no evident valvular disease. HFPEF may be responsible for as much as 50% of heart failure in the older adult population. Hypertension is a key driver of HFPEF, often through the development of left ventricular hypertrophy, which leads to stiffening of the ventricle, but other factors, including microvascular endothelial dysfunction,24 mild degrees of valvular dysfunction, and atrial fibrillation, with the loss of atrial kick to assist with filling a stiff ventricle, may also contribute. Recent data have suggested that obesity is also an important causative factor in HFPEF, in part by alteration of hemodynamics and respiratory function, but also via the effects or, or resistance to, adipocytokine secretion (e.g., adiponectin, leptin).25 Not infrequently, heart failure will be precipitated by anemia, alcohol, and a number of other factors.26 Obstructive sleep apnea is frequently underdiagnosed, often coexists with obesity, and is itself a risk factor for cardiovascular disease, as well as a precipitant for heart failure (Box 39-1).
Pathophysiology
It is now clear than heart failure is a systemic disease, affecting not just the heart and vasculature, but involving most organ systems, including lung, skeletal muscle, brain, kidneys, gut, and adipose tissue. The relationships among these involved organs are mediated by derangements of inflammation and immunologic signaling, neurohormonal axes, and other circulating factors, several of which are also implicated in relation to frailty.16 As previously noted, heart failure may occur with reduced ejection fraction (HFREF) or preserved ejection fraction (HFPEF); these entities share some common risk factors but have important differences in pathophysiology.
The pathophysiology of heart failure is multifactorial, especially in older adult patients in whom hypertensive heart disease and valvular heart disease are more common. There may be structural abnormalities within the heart, together with overcompensatory mechanisms in the renin-angiotensin-aldosterone system (RAAS), sympathetic nervous system, and peripheral vasculature. Although there are specific changes in the cardiovascular system with age (see Chapter 14) such as increased calcification, increased myocardial fibrosis, and reduced ventricular compliance, most older adult patients with heart failure have additional pathology to explain their symptoms. In patients with heart failure due to ischemia, remodeling can result in alterations in the shape and morphology of the left ventricle,27 ultimately with left ventricular dilation and a large end-diastolic volume. In addition to changes in the structure of the left ventricle, many older adult patients have associated calcific degeneration of the aortic and mitral valves, with functional and hemodynamically significant consequences. The cardiomyopathies are also a small but significant cause of heart failure in older adult patients, although the widely seen asymmetric septal hypertrophy itself is not of great significance.28 In hypertensive patients with left ventricular hypertrophy, the increase in collagen content of the ventricular wall and associated myocardial fibrosis may lead to diastolic filling abnormalities, which may contribute to the symptoms of heart failure, and represent a pathophysiologic substrate for HFPEF. In addition, loss of atrial contraction can result in significant hemodynamic deteriorations because atrial systole has an increased importance in older adult patients when left ventricular wall stiffness is increased.29,30
In a healthy person, cardiac output is influenced directly by stroke volume and heart rate. In the failing heart, stroke volume is maintained by increasing the left ventricular end-diastolic pressure and volume, which is the basis of the Starling law of the heart. However, eventually, at very high left ventricular end-diastolic volumes, there will be no subsequent compensatory increase in cardiac output. One of the aims of heart failure treatment is to minimize increases in left ventricular end-diastolic pressure so that cardiac output can be maintained and subsequent tissue oxygenation will be adequate for perfusion of the vital organs.
In older adults, heart failure with preserved systolic function (HFPEF) becomes increasingly more common. Although this entity shares risk factors (e.g., hypertension, diabetes) with HFREF, it appears to be pathophysiologically distinct. A history of myocardial infarction is less common, obesity is more common, and derangements of adipokine levels and function appear to play a role. Although subtle derangements of systolic function are seen in HFPEF, impaired relaxation and ventricular filling are important. Left ventricular dilation is not a feature, and cardiac output remains well matched to the degree of peripheral vasodilation.31 Similar systemic derangements, including those of neurohormonal systems, cytokines, and skeletal muscle function, are seen in HFPEF and HFREF, but the reasons why some patients develop HFPEF and some develop HFREF are poorly understood.
The autonomic nervous and neuroendocrine systems initially support the failing heart, but ultimately the compensatory mechanisms may themselves prove harmful. Activation of the RAAS can result in increased levels of angiotensin and aldosterone in the heart, kidney, brain, and vascular system, with undesirable consequences.32 Furthermore, the associated high levels of plasma adrenaline and noradrenaline (epinephrine and norepinephrine) are associated with a poor prognosis due to deleterious effects on myocardial function, autonomic balance, and peripheral vascular function.
In both HFREF and HFPEF, changes in the morphology of skeletal muscle may explain the fatigability seen in heart failure patients over and above that expected with reduced tissue blood supply.33,34 Disruption of the microvasculature is also seen with impaired endothelial function. These changes are usually consequences of the disease process and not merely related to age, although in extremely old patients with mild symptoms of cardiac failure, true pathologic processes and age-related processes may be difficult to differentiate. Such age-related changes include a reduction of cardiac output on exercise, increase in end-systolic volume, decrease in ejection fraction with exercise, and reduced heart rate with exercise. It is important to note, however, that heart failure is a disease with systemic effects—derangements of immune function cause a proinflammatory response35 that may in itself be cardiotoxic and contributes to the development of anemia; circulating cytokines may also help drive the prominent skeletal myopathy that accompanies heart failure and is the major cause of tiredness and breathlessness in heart failure patients. This skeletal myopathy in turn causes abnormalities of ergoreceptor function36 that drive further sympathetic nervous system activation. Disturbance of lung architecture and gas exchange are seen in the lungs of heart failure patients, even in the absence of overt fluid overload, a further contributor to the symptoms of heart failure.
Diagnosis of Heart Failure
It is often straightforward to recognize heart failure when the patient has pronounced symptoms and signs accompanied by echocardiographic evidence of left ventricular dysfunction. The diagnosis is often more difficult when symptoms are mild; signs may be absent in the early stages of the disease and, even later, might chiefly be due to frailty syndrome or functional decline without overt dyspnea. Differentiating HFPEF from other causes of exercise intolerance and breathlessness may be particularly difficult.
The European Society of Cardiology (ESC) has developed guidelines for the diagnosis of heart failure3 (Table 39-2). The American College of Cardiology (ACC) and American Heart Association (AHA) guidelines4 approach diagnosis in a similar way. For the clinician who is faced with an older adult patient with suspected heart failure, two questions should be considered before further assessment:
1. Are the patient’s symptoms at least partly cardiac in origin?
2. If so, what type of cardiac disease is producing these symptoms?
TABLE 39-2
Diagnosis of Heart Failure (HF)
| HFREF: All Three Present | HFPEF All Four Present |
| Symptoms typical of HF | Symptoms typical of HF |
| Signs typical of HF | Signs typical of HF |
| Reduced LVEF | Normal or only mildly reduced LVEF; left ventricle not dilated |
| Relevant structural heart disease (LVH, enlarged left atrium, diastolic dysfunction) |
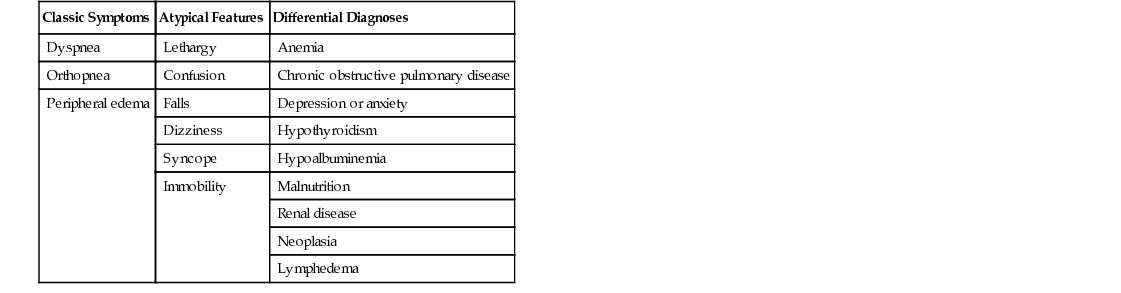
Table 39-3 lists the typical and atypical symptoms in the older adult patient with suspected heart failure and potential differential diagnoses.
The diagnosis of heart failure is especially difficult because it is not defined by an absolute level of any one parameter, as is the case with a number of other diseases. Consequently the diagnosis is a judgment based on a careful history and examination, chest radiology, electrocardiography, echocardiography, and other routine baseline investigations, such as complete blood count, serum biochemistry, and thyroid function.
Clinical History
The most classic symptom of heart failure is exertional breathlessness. However, this is a common symptom and is often a result of chronic obstructive pulmonary disease (COPD), deconditioning, obesity, or interstitial lung disease. Most people will experience some breathlessness with moderate exertion and, during exercise, the stage at which breathlessness is experienced depends on the overall level of fitness.
Anemia and obesity are confounding factors that make exertional dyspnea a very nonspecific symptom. Orthopnea is a more specific symptom that does not occur in normal patients and is not usually a feature in respiratory disease. However, the disease process has to be relatively advanced before orthopnea occurs and, even if it is present, diuretics have often been instituted by the patient’s general practitioner to relieve this symptom. Likewise, paroxysmal dyspnea (PND) is a more extreme version of dyspnea and is a result of fluid redistribution, which increases the left ventricular end-diastolic pressure. Again, PND is specific but is an insensitive symptom because it signifies significant fluid overload, which should have been noted and previously treated.
Fatigue and lethargy are other common problems in heart failure, but they are even harder to define and assess than dyspnea, particularly in older adult patients. Fatigue is common in people who are ill and more common still in older adults who are frail; indeed, it forms one of the components of Fried and colleagues’ phenotypic definition of frailty.38
Ankle edema is a common presenting feature but, again, there are many alternative causes, such as cor pulmonale, deep venous thrombosis, dependent edema, or hypoalbuminemia.
Risk factors for heart failure may also assist the diagnosis. In particular, myocardial infarction is a key risk factor for future HFREF.39 Although hypertension is an important risk factor for both HFREF and HFPEF, the prevalence of hypertension is so high in older adults that it becomes less useful as a diagnostic discriminator. Additional features that may suggest the diagnosis of heart failure include excessive alcohol intake, history of rheumatic fever, or presence of atrial fibrillation. Note too, however, that heart failure is associated with cognitive impairment, including memory impairment and frontal lobe dysfunction, which often manifests with slowness and decreased initiative.6 In consequence, it is easy in a busy clinical practice to be misled by incomplete or seemingly vague answers; both false-positive and false-negative responses can put the history off track.
Physical Signs
Many of the physical signs of heart failure are nonspecific and of relatively low predictive value. These include tachycardia, pulmonary crepitations, and peripheral edema. Equally, many of the physical signs that are specific to heart failure are insensitive because they occur only once the heart failure has become severe. These include elevation of the jugular venous pressure, a gallop rhythm, and displacement of the cardiac apex beat. The situation is further compounded by the variable ability of physicians to detect these clinical signs.40 As a result, diagnosis may be difficult, especially in older adults who may be less likely to present with typical signs. Signs are less likely to manifest in mild heart failure, and diuretic therapy often leads to rapid resolution of signs of fluid overload. Such a response to diuretic therapy can be used to assist with the diagnosis. The probability of the diagnosis of heart failure thus requires signs and symptoms to be considered by the individual clinician, making full use of clinical judgment.
Investigations
Investigations in patients with suspected heart failure are aimed at the following: (1) confirming the diagnosis; (2) searching for other diseases likely to contribute to the symptom complex (such diseases often coexist with heart failure); and (3) defining the cause and subtype of heart failure.
Chest X-Ray
Chest x-ray should be performed routinely. Cardiac enlargement (cardiothoracic ratio > 50%) implies cardiomegaly and, if present, suggests a higher probability of HFREF.41 However, many heart failure patients do not exhibit cardiomegaly, so it is a specific but insensitive test. Other helpful chest x-ray findings are pulmonary edema, upper lobe diversion, fluid in the horizontal fissure, and Kerly B lines in the costophrenic angles. In severe cases, pleural effusions may be present, although there may be alternative explanations for them, such as bronchial carcinoma, pneumonia, or pulmonary emboli.
A chest x-ray can reveal other clues about noncardiac disease that might be causing breathlessness. A lung tumor might be obvious, and evidence of COPD or pulmonary fibrosis may also be present. Nevertheless, the chest x-ray should be seen as a whole. For example, the finding of cardiomegaly plus bilateral pleural effusions, with no other parenchymal lung disease, makes heart failure likely—although the presence of structural heart disease should still be confirmed by echocardiography.
Electrocardiography
The 12-lead electrocardiogram (ECG) should be obtained routinely. Left ventricular systolic dysfunction is rare in the presence of a completely normal 12-lead ECG, making it a useful rule-out test. For HFREF, an abnormal resting ECG is sensitive (94%), with excellent negative predictive value (98%), but is much less specific (61%) and has a poor positive predictive value (35%).42 Most studies suggest that this is the case; where there is doubt, an echocardiogram should be obtained.
Other abnormalities on the ECG may be useful in the assessment of patients. For example, the presence of atrial fibrillation may be useful in concluding whether the patient should receive additional anticoagulation.
Echocardiography
The optimum investigation in the older adult patient with suspected heart failure is echocardiography. Measurement of the left ventricular ejection fraction is the preferred index of systolic function43 because it is simple and less prone to error from regional wall motion abnormalities than alternatives. Regional wall motion indices are an alternative approach, but these are less widely used in practice. Echocardiography can clearly distinguish whether the left ventricle is dilated; this approach for assessing left ventricular dimensions is superior to chest x-ray.
Echocardiography can also identify patients with mitral valve disease or aortic stenosis, which may both contribute to the syndrome of heart failure and indicate who may benefit from surgery. It can also assess left ventricular wall thickness, and hence hypertrophy, and left atrial size, both important for making a diagnosis of HFPEF. Finally, echocardiography can be used to assess diastolic dysfunction. Debate continues about the optimum way to assess this, and an array of indices should be measured and reported. Key measurements include the mitral inflow pattern and tissue Doppler measures of longitudinal shortening of the ventricle.
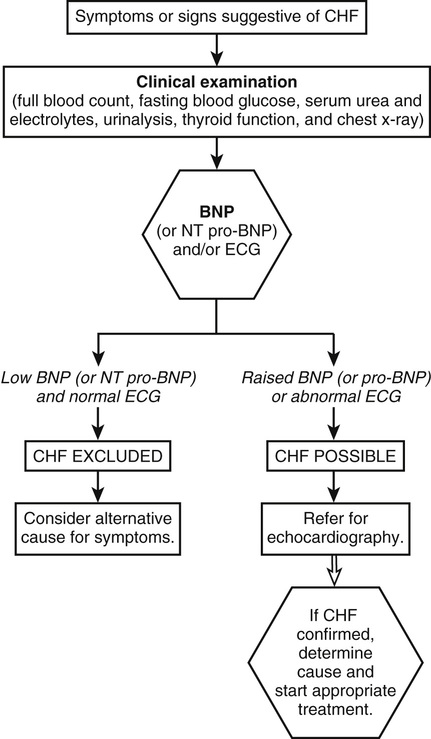
When echocardiography proves to be technically difficult, objective assessments of left ventricular function may be made by radionuclide ventriculography or by cardiac magnetic resonance (MRI) scanning. Figure 39-1 suggests an approach for diagnosing heart failure in practice.
Natriuretic Peptides
The natriuretic peptides (NPs) released from the atrium and ventricles have a variety of cellular effects, act as vasodilators, and cause a natriuresis. They have been shown to reflect left ventricular wall stress. Natriuretic peptide levels (usually B-type natriuretic peptide [BNP] or its cleavage product, N-terminal [NT] pro-BNP) are useful in excluding heart failure in acute and chronic situations. Low levels (<35 pg/mL of BNP or <125 pg/mL of NT pro-BNP) are thresholds recommended by the ESC3 in the chronic situation to rule out heart failure and should prompt a search for alternative diagnoses, especially if the ECG is also normal. Higher levels do not make the diagnosis of heart failure, because any cardiac abnormality (e.g., myocardial ischemia, atrial fibrillation, left ventricular hypertrophy) can lead to elevated BNP levels. However, elevated levels should prompt further investigations, including echocardiography.
In summary, the diagnosis of heart failure is a sequential one that relies on a clear clinical history and examination followed by electrocardiography, chest radiology, or echocardiography. Echocardiography is desirable in all cases, although it may not be readily available in the community or in small hospitals. Nevertheless, it is probably more important to obtain an echocardiogram for the older adult patient before initiating treatment because structural abnormalities are more common, and optimum treatment requires as accurate a diagnosis as possible so that adverse effects may be kept to a minimum.
Treatment of Heart Failure
General Issues
Since the 1960s, when loop diuretics were introduced, treatments for heart failure have diversified. As the pathophysiology of heart failure has become clearer, treatment options have broadened and a number of agents, including angiotensin-converting enzyme (ACE) inhibitors, β-blockers, and aldosterone antagonists, have now been shown to improve prognosis. It is now known that the impairments in left ventricular function and the peripheral circulation can be treated, with consequent hemodynamic improvement. Neurohumoral activation can be blocked and left ventricular remodeling reduced. These adverse consequences of heart failure are the targets of drug treatment. As a result, patients may require multidrug treatment, and priorities need to be established. It is important that patients and their caregivers understand the implications of their treatment.
In the frail older adult patient, quality of life and alleviation of symptoms are especially important. The major clinical trials of heart failure have generally excluded older patients, so that most patients enrolled in studies are in the age range of 50 to 70 years, favoring single-system and single-cause disease. Although the mean age of patients enrolled in heart failure trials is rising, it still lags behind the age of most heart failure patients.44 Typical heart failure patients are not only old but are often frail, with many active comorbid illnesses that may require management.
Such complex patients require multidimensional evaluation and management in the hospital and in the community. This ensures that a full picture of the patient’s abilities, needs, and wishes is obtained, so that the goals of treatment are fully aligned with what the patient requires. It is clearly of little use to treat heart failure with all the recommended therapies but to impair function and quality of life further through the development of intolerable side effects.
As with all medication use in older adults, a drug should be started at a low dose and titrated in relation to the response, especially because patients may be taking over-the-counter preparations, and the potential for drug interactions is considerable.45 Each of the aforementioned drug classes will be considered in more detail but, in addition to the main therapeutic options, drugs that have less proven efficacy will be discussed (Table 39-4).
TABLE 39-4
Summary of Treatment Options for Heart Failure in Older People
| HFREF | HFPEF | |
| Recommended | Diuretics; ACE inhibitor or ARB β-blocker, aldosterone antagonist | Diuretics |
| Adjunctive therapy | Nitrates or hydralazine (if ACE inhibitor– or ARB-intolerant), digoxin, biventricular pacing (if dyssynchrony), intravenous iron | Intravenous iron |
| Possible benefit | Exercise training | ACE inhibitor or ARB, exercise training |
Pharmacologic Agents
Diuretics
Diuretics are fundamental to the treatment of chronic heart failure. The loop diuretics introduced in the 1960s were shown to be very effective in reducing symptoms associated with fluid retention, and they had a clear hemodynamic benefit. Studies have shown deterioration in symptomatic heart failure when diuretics are withdrawn,46 and diuretics have been shown to reduce mortality and hospitalization in chronic heart failure.47
The loop diuretics, which include furosemide and bumetanide, block the sodium-potassium-chloride transport exchange in the ascending limb of the loop of Henle. Thiazides have a different site of action and work in the distal convoluted tubule. Spironolactone has a different mode of action, antagonizing the aldosterone-mediated sodium exchange with potassium and hydrogen in the collecting ducts. In older adult patients with heart failure, the rate of absorption of loop diuretics and time to peak plasma concentration are reduced because renal function is often impaired. High doses of diuretics may need to be used to produce a diuresis because the coexisting relative acidosis results in increased competition for the organic acid transport pathway at the proximal tubule. The bioavailability of furosemide can be vary considerably, from 20% to 80%, but is more consistent with bumetanide.48 Most of the loop diuretics have a fairly short half-life, about 1 to 2 hours. In contrast, the thiazide and potassium-sparing diuretics have longer half-lives, which allow once-daily doses to be given. Tolerance can occur to diuretics, and this has clinical relevance. The natriuretic response diminishes after the first dose, but this can be reversed by restoring intravascular volume. Long-term administration of a loop diuretic can also result in tolerance, which can be addressed by combining loop and thiazide diuretics together.
When furosemide is given to patients with severe acutely decompensating heart failure, high doses should be used until symptoms and signs of fluid overload have been controlled. An intravenous dose of 40 to 50 mg is often sufficient to control the symptoms; but when resistance to loop diuretics occurs, up to 250 to 500 mg/day may be required. In resistant cases, furosemide can be given by a continuous infusion, up to 4 g/day.
Thiazides (e.g., metolazone, high-dose bendroflumethiazide) can be used for resistant edema and heart failure. They block sodium reabsorption in the proximal convoluted tubule, along with having effects on the distal convoluted tubule. They can result in a profound diuresis, and postural hypotension may be significant if intravascular volume depletion is too extreme. Close monitoring of electrolytes is essential.
When patients with heart failure are being treated with a diuretic, it is essential to monitor plasma biochemistry regularly. Particular electrolyte disturbances include the following: hypokalemia, which may precipitate cardiac arrhythmias; hyponatremia, which may cause drowsiness and fits; and hypomagnesemia, which may cause a number of cellular effects, including muscle weakness and arrhythmias. Hypokalemia may be alleviated by the concomitant use of potassium-sparing diuretics such as spironolactone or by using an ACE inhibitor (see later discussion). Diuretic treatment can also result in disturbances of lipid metabolism, glucose intolerance, and hyperuricemia.
In addition to these diuretic side effects, older adult patients are prone to difficulties with urinary incontinence, immobility, postural hypotension, dehydration, and confusion. These problems should be prominent in the prescriber’s mind when initiating treatment in an individual patient. It is also important not to administer intravenous furosemide rapidly because this may precipitate an irreversible hearing loss.
A study of older adults49 assessed the impact of discontinuing diuretic therapy for those with relatively mild symptoms of heart failure; patients with severe symptoms and acute heart failure and those requiring intravenous diuretics were excluded. In the follow-up period, diuretic therapy had to be reintroduced in half of the patients in whom it had been withdrawn because of symptomatic deterioration. Even though the patients in whom diuretic therapy had to be restarted were relatively well, this study highlights the likelihood of a recurrence of symptoms if diuretics are discontinued in an older adult population.
Angiotensin-Converting Enzyme Inhibitors
ACE inhibitors block overactivity of the RAAS and sympathetic nervous system. In addition to these effects, ACE inhibitors enhance the bradykinin–nitric oxide system in the vascular endothelium.50 They may also have an influence outside the circulation in various tissues, including skeletal muscle.51 ACE inhibitors are now known to reduce morbidity and mortality in patients with left ventricular systolic dysfunction, regardless of symptom severity,52–54 and are also effective at improving exercise capacity and symptoms, even in very old heart failure patients.55,56 Mechanistically, ACE inhibitors are vasodilators with subsequent reduction in cardiac preload and afterload, resulting in hemodynamic and symptomatic improvement for patients with heart failure. In addition to reducing the pathologic overactivity of the RAAS, ACE inhibitors have beneficial effects on the endothelium and may also have antiischemic effects.57 ACE inhibitors inhibit adverse remodeling of the myocardium after infarction and lead to reductions in ventricle size and improvements in ejection fraction in patients with LV systolic dysfunction.
The main contraindications to treatment with ACE inhibitors are severe aortic stenosis and renal impairment. Patients who are volume-depleted are more likely to experience hypotension with the initial dose, so ACE inhibitors should be introduced when patients are euvolemic or fluid-overloaded. Treatment should be started at a low dose and gradually uptitrated until the maximum achievable dose is obtained. In general terms, the optimal benefit is obtained at the top end of the dosage range. The ATLAS study58 compared low and high doses of lisinopril in heart failure, and patients with higher dosages fared better. However, a low dose of ACE inhibitor is likely to be of more benefit than none. Renal function and electrolytes should be monitored at regular intervals, initially every few days or weekly and then every 3 to 6 months. It may be possible to reduce the dose of maintenance diuretic therapy once the patient has been established on ACE inhibition. Although aortic stenosis has traditionally been thought of as a contraindication to ACE inhibitor therapy, patients with mild to moderate aortic stenosis started on an ACE inhibitor appear to have a lower mortality than controls in observational studies.59 Severe aortic stenosis, however, remains a contraindication to ACE inhibitor therapy.
The effects of ACE inhibitors on heart failure appear to be a class effect, and there is little to choose among the once-daily ACE inhibitors in current use. The main side effects of ACE inhibitors include cough, hypotension, hyperkalemia and, rarely, angioneurotic edema. The occurrence of a cough with ACE inhibitors should prompt a switch to an angiotensin receptor blocker (ARB). Although orthostatic hypotension can occur in patients treated with an ACE inhibitor, this is much less common with once-daily agents and is often precipitated by hypovolemia due to overdiuresis or by underlying vascular disease, rather than the treatment itself. Rather than stopping the ACE inhibitor, the first response should be to reduce the diuretic dose.
The clear benefit of ACE inhibitors in HFREF is not mirrored in patients with HFPEF. The PEP-CHF study60 compared perindopril with a placebo in older adult patients with preserved systolic function heart failure. There was no significant reduction in mortality, but symptoms and hospitalization were improved in the perindopril group. A recent meta-analysis has confirmed the lack of benefit of ACE inhibitors on mortality in HFPEF61 and also does not suggest benefit in hospitalization or symptoms. In practice, however, many older adults with HFPEF will require an ACE inhibitor for another indication, such as myocardial infarction, hypertension, or stroke disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree