Primary tumor (T)
Tx
Primary tumor cannot be assessed
T0
No evidence of primary tumor
Tis
Carcinoma in situ
T1
Tumor ≤ 2 cm in greatest dimension
T2
Tumor >2 cm but ≤4 cm
T3
Tumor > 4 cm
T4a
Moderately advanced local disease: invades through cortical bone, inferior alveolar nerve, floor of mouth, or skin of face
T4b
Very advanced local disease: invades masticator space, pterygoid plates, skull base, or encases internal carotid artery
Regional lymph nodes (N)
NX
Cannot be assessed
N0
No regional LN metastasis
N1
Metastasis in single ipsilateral lymph node ≤3 cm in greatest dimension
N2
N2a
Single ipsilateral LN >3 cm but <6 cm
N2b
Multiple ipsilateral LN, none > 6 cm
N2c
Bilateral or contralateral LN, none >6 cm
N3
Metastasis in a LN >6 cm
Distant metastasis (M)
M0
No distant metastasis
M1
Distant metastasis
Stage
T
N
M
0
Tis
N0
M0
I
T1
N0
M0
II
T2
N0
M0
III
T3
N0
M0
IVA
T4a
N0–N1
M0
T1, T2, T3, T4a
N2
M0
IVB
Any T
N3
M0
T4b
Any N
M0
IVC
Any T
Any N
M1
7.2 Role of Chemotherapy
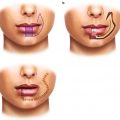
Treatment of lip cancers usually involves locoregional resection since they are frequently detected and treated early. However, with large or recurrent cancers, there is an increased risk of local and distant spread. As there are fewer cases specific to lip cancer, most of the data is extrapolated from the data in squamous cell carcinomas of the head and neck. The mainstay of treatment is first surgical resection of the primary tumor (including a neck dissection if indicated). Adjuvant radiation therapy and chemotherapy can often be incorporated if high-risk features are present [5].
7.2.1 Stage I and II
For Stage I and II disease (T1–T2, N0): the initial step is surgical resection. For those with positive margins and/or high-risk features, adjuvant radiation with or without concurrent chemotherapy can be considered. The two sentinel trials conducted in the USA (Radiation Therapy Oncology Group; RTOG 9501) and in Europe (European Organization Research and Treatment of Cancer; EORTC 22931) established level I evidence for postoperative treatment and outlined high-risk features as perineural involvement, extracapsular spread, vascular tumor embolism, and the involvement of ≥2 regional lymph nodes [5, 10]. Additional subgroup analysis of these data suggests that positive margins and extracapsular spread are the most significant factors in predicting poor outcome [11]. Patients with these high-risk features gained an additional benefit from the addition of adjuvant chemotherapy to radiation both in terms of locoregional control and disease-free survival. There is also no established consensus on the definition of a positive margin; an Australian study evaluating only lip cancers used 3 mm surgical margins as the cutoff for adjuvant radiation. The study also noted tumor depth ≥4 mm as a poor prognostic sign to having nodal spread [12]. In general, 0.5 cm margins around the tumor is considered mainstay. In the neoadjuvant setting, case reports of using intralesional methotrexate before surgery to reduce the size of the lesion for improved surgical and cosmetic outcomes suggest possible utility of this strategy. However, there are no current randomized, controlled trials to evaluate this against control of directly undergoing resection [13]. In these patients, the role of neoadjuvant chemotherapy remains to be further investigated.
7.2.2 Stage III and IV
Surgery is still preferred for the initial treatment of stage III and IV (T3–T4, N0, or any T with N1–3) disease. Neck dissections depending on the level of lymph node spread should also be considered, especially for lower lip cancer. In the presence of high-risk features such as extracapsular nodal spread, positive margins, multiple positive lymph nodes, and perineural/vascular/lymphatic invasion, adjuvant chemotherapy and radiation improves both locoregional control and disease-free survival [5, 10].
The EORTC 99231 study evaluated adjuvant concurrent chemotherapy with radiation compared to radiation alone in patients with stage III/IV head and neck squamous cell carcinoma or those with stage I/II with the aforementioned high-risk features using cisplatin 100 mg/m2 IV Day 1, 22, and 43 with total 66 Gy radiotherapy over 5½ weeks. Results noted a longer progression-free survival of 55 months in concurrent chemotherapy-RT group versus 32 months in radiotherapy alone (p = 0.04) and improved overall survival in combined group as well of 72 months versus 32 months (p = 0.02) [10]. The RTOG 9501 trial evaluated the same regimen of cisplatin 100 mg/m2 on days 1, 22, and 43 with concurrent radiation compared to radiation alone in the adjuvant setting. This study noted longer disease-free survival in combined group (p = 0.04) but no significant improvement in overall survival compared to the former study [5].
Data from these two studies along with subsequent subgroup analyses demonstrate improved outcomes with the use of concomitant cisplatin to postoperative radiation for those carefully selected patients who can tolerate chemotherapy [5, 10, 11].
As mentioned before, the role of induction chemotherapy remains unclear in lip cancer. However, extrapolating from the Department of Veterans Association Laryngeal Cancer Study Group data, the use of induction chemotherapy of cisplatin and 5-fluorouracil and radiation followed by total laryngectomy versus surgery followed by radiation alone in larynx cancers did not show a significant difference in overall survival in stage III and IV laryngeal squamous cell carcinomas. It did, however, note less distant metastasis in the chemotherapy arm [14]. This led to RTOG 91-11 in advanced squamous cell laryngeal cancer which evaluated three arms: (1) induction cisplatin plus 5-fluorouracil followed by radiation, (2) concurrent cisplatin and radiation, or (3) radiation alone. The group that received concurrent chemotherapy and radiation had better locoregional control and organ preservation, but both chemotherapy arms had less distant metastasis versus radiotherapy alone [15]. These laryngeal squamous cell carcinoma studies established concurrent chemotherapy and radiation as a standard of care with improved locoregional control compared to radiation alone. Because the chemotherapy groups demonstrated a decreased rate of distant metastases, other studies further evaluating the role of induction chemotherapy were subsequently conducted.
In the setting of unresectable disease, the 5-year survival with radiation alone was <20 % leaving much to be further improved upon. Two studies evaluated the role of induction chemotherapy (TAX 323 and TAX 324) published in NEJM in 2007. They evaluated induction chemotherapy with docetaxel (T), cisplatin (P), and 5-fluorouracil (F) compared to cisplatin/5-fluorouracil followed by radiation or concurrent chemo-RT. TAX 323 evaluated TPF vs PF as induction chemotherapy in locoregional or metastatic head and neck squamous cell carcinoma. The chemotherapy regimen consisted of docetaxel 75 mg/m2 IV Day 1, cisplatin 75 mg/m2 IV Day 1, and 5-FU 750 mg/m2 continuous IV Days 1–5 every 3 weeks for four cycles total followed by radiation therapy. The study showed a 28 % decrease in risk of disease progression or death. The docetaxel-containing arm also had a significant improvement in progression-free survival of 2.8 months and an improvement in overall survival of 4.3 months over the PF-containing arm(p = 0.02) [16]. TAX 324 evaluated two induction chemotherapy regimens: (1) TPF (docetaxel 75 mg/m2 IV Day 1, cisplatin 100 mg/m2 IV Day 1, and 5-FU 1,000 mg/m2 continuous IV Days 1–4 q3 weeks for three cycles) versus (2) PF (intravenous cisplatin 100 mg/m2, followed by fluorouracil 1,000 mg/m2 per day as a continuous 24 h infusion for 5 days). Both induction chemotherapy arms were followed by 7 weeks of radiation therapy with weekly concurrent carboplatin. The study noted a 30 % decrease in the risk of death in the TPF group as well as longer median survival (71 months versus 30 months), increase in 3-year survival (62 % versus 48 %), and longer progression-free survival (36 months versus 13 months) – all of which were statistically significant [17].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree