html xmlns=”http://www.w3.org/1999/xhtml” xmlns:mml=”http://www.w3.org/1998/Math/MathML” xmlns:epub=”http://www.idpf.org/2007/ops”>
Précis
Definition of terms
Blood–brain barrier: highly selective permeability barrier that separates the circulating blood from the brain extracellular fluid in the central nervous system
Radiation therapy: therapy using ionizing radiation to control or kill malignant cells
Chemotherapy: drug treatment that uses powerful chemicals to kill fast-growing cells. Chemotherapy is most often used to treat cancer, since cancer cells grow and multiply much more quickly than most cells in the body
Angiogenesis: formation of new blood vessels. This process is a normal part of growth and healing, but it is also connected to the development of cancer. Once a tumor grows to a certain size, it requires nutrients and oxygen found in the blood to help it grow, invade nearby tissues, and spread. The tumor sends chemical signals out that stimulate the growth of new blood vessels. As a result, each part of the angiogenesis process is a potential target for new cancer treatments (“starving the tumor to death”)
Tyrosine kinase inhibitors: class of medications that inhibit, or block, the enzyme tyrosine kinase. They were created following a better understanding of DNA, the cell cycle, and molecular signaling pathways and thus represent a molecular method of cancer treatment. They allow for targeted treatment of specific cancers, which could potentially lessen the risk of damage to healthy cells and increase treatment success.
Key points to be covered
Carmustine wafers are indicated in patients with newly diagnosed high-grade malignant glioma as an adjunct to surgery and radiation therapy.
Carmustine wafers are also indicated in patients with recurrent GBM as an adjunct to surgery.
On March 15, 2005, the US FDA approved temozolomide for the treatment of adult patients with newly diagnosed GBM concomitantly with radiation therapy and then as maintenance treatment. Temozolomide previously received accelerated approval in 1999 for the treatment of adult patients with refractory anaplastic astrocytoma. This treatment indication was also converted to full approval based on the results of the GBM study.
Patients with newly diagnosed GBM and MGMT gene methylation benefit the most from the addition of temozolomide to radiation therapy.
On May 5, 2009, the FDA granted accelerated approval to bevacizumab as a single agent for patients with GBM, with progressive disease following prior therapy. The approval was based on demonstration of durable objective response rates observed in two single-arm trials, AVF3708g and NCI 06-C-0064E.
Despite its limitations, bevacizumab remains the single most important therapeutic agent for GBM since temozolomide.
Introduction
Historical perspective
Compared to oncology in general, the field of neuro-oncology lagged behind for decades. Almost 100 years separate the first described successful glioma resection by A. H. Bennett and Richman Godlee in 18841 and the 1978 landmark trial demonstrating a clear improvement in survival from 14 to 36 weeks in anaplastic glioma patients treated with radiation therapy versus controls.2 It would take more than two decades for the next milestone to be reached, that being the report in 1998 that 1p/19q co-deletion in anaplastic oligodendroglioma patients increased the efficacy of chemotherapy.3 Since then, after a very slow start, continuous improvements in the fields of radiology, radiation therapy, and cancer therapeutics have led to considerable development in the field of neuro-oncology, and bring hope for a tremendous potential for advance over the coming years.4
Primary central nervous system (CNS) tumors represent only 1.35% of all cancers and 2.2% of all cancer-related deaths.5 Glial neoplasms represent about 40% of all primary CNS tumors and over three-quarters are malignant.6,7 Despite the current standard treatments for malignant glioma, including surgical resection, radiation therapy, and chemotherapy, the survival of patients with malignant glioma remains dismal, with a median survival of 3–4 years for patients with anaplastic astrocytoma8 and around 15–18 months for glioblastoma patients.9–11
Glioblastoma (GBM), the most common malignant primary brain tumor,12 has an incidence of 5 per 100,000 individuals. Despite hundreds of clinical trials worldwide since the 1960s, few therapies have been approved by the US Food and Drug Administration (FDA) for the treatment of GBM. In the last decade two therapies were approved, temozolomide for newly diagnosed GBM and bevacizumab for recurrent GBM. These two agents only extend median survival a few months, and less than half of treated patients show objective responses to either agent. Thus, median survival of newly diagnosed GBM remains around 15–18 months,11,13,14 and for recurrent GBM, only 6–9 months.15–17 There are only a very few long-term survivors, and virtually all GBMs recur.18
In addition to the fatal prognosis, malignant gliomas affect many patients in their 40s and 50s, frequently terminating promising lives prematurely and depriving young families of parents and spouses.
The reasons for the poor outcome of GBM are several. First, despite decades of epidemiological research, the only proven cause of GBM, ionizing radiation, accounts for far less than 1% of cases. Up to 5% of GBM cases arise in situations of inherited genetic abnormalities, such as the Li–Fraumeni syndrome, characterized by germline mutations in the TP53 gene 1. Thus, with no knowledge of the etiology in at least 95% of cases, prevention by avoiding cause cannot be instituted.
Second, the blood–brain barrier (BBB) markedly impedes the delivery of drugs or macromolecule. Although there is some breakdown of the BBB in parts of GBM, many of the cells, particularly the invading cells, reside behind a completely normal BBB. Only very small molecules, lipid-soluble molecules, or those transported by the limited number of transport systems, such as the large amino acid transport system, can reach most GBM cells. Large water-soluble molecules, such as antibodies, cannot reach the majority of GBM cells by intravenous or even intracarotid artery delivery methods.19 Unfortunately, the CNS can be seen as a pharmacologic sanctuary because drug delivery to the brain via systemic administration is often difficult and incomplete secondary to the BBB. It is recognized that the BBB is disrupted in many malignant brain tumors. In these tumors, blood vessels have abnormal tight junctions and disrupted endothelial surface, which allow water-soluble contrast agents to cross into the tumor and hence appear enhancing on magnetic resonance imaging (MRI). This brain–tumor barrier tends to be more permeable than normal brain tissue; however, the breakdown of the BBB in the area of tumor is variable, and large areas exist where the BBB remains intact. In those areas, the amount of drug reaching the tumor continues to be severely restricted.20,21 In addition, the brain adjacent to tumor is the area around the tumor that contains infiltrating tumor cells. These sites may be associated with an intact BBB, and drug delivery to this area is difficult. Finally, although most brain tumors tend to be highly vascular, the aberrant tumor-induced angiogenic process tends to create abnormal vessels such as blind loops and arteriolar-venule shunts, making parenchymal drug delivery even more inefficient. In fact, the passage of substances across the BBB depends on their size, lipid solubility, and ionization state.22 Most hydrophilic substances and large lipophilic substances (which include many chemotherapeutic compounds) are restricted from entering the CNS.
Third, the immense diversity of GBM23 and its genetic amplification, mutation, deletion, expression, and epigenetic abnormalities, such as gene promoter methylation, as well as its multiple and redundant signaling pathways, have been described in great detail by The Cancer Genome Atlas (TCGA) GBM effort,24 and the Vogelstein/Hopkins and Bigner/Duke whole-genome sequencing GBM studies.25,26 With over 2,000 somatic mutations identified25,26 in GBM, targeted therapy with small-molecule inhibitors is plagued by escape mechanisms.
Clearly, more effective therapies are desperately needed for patients afflicted with these tumors. Below is a review of the therapies currently approved or considered part of the “standard of care” for malignant gliomas.
Summary
In this chapter, we will review currently approved therapies by the US FDA for the treatment of primary malignant gliomas in adult patients, including nitrosoureas (carmustine and lomustine), carmustine wafers, temozolomide, and bevacizumab. We will review the trials leading to the approval and the follow-up trials supporting the approval of these therapies.
Clinical evidence-based practice
Chemotherapy
Chemotherapies are treatment modalities that are being used to control and ideally eradicate infiltrative tumor cells.
Nitrosoureas
Nitrosoureas were the first agents used in monotherapy to treat gliomas as they readily cross the BBB due to their small size, non-ionized state, and high lipid solubility.27 Bis-chloroethylnitrosourea (BCNU or carmustine) became the most commonly used single-agent chemotherapy for recurrent disease and was moved to the adjuvant setting after a randomized trial (BTSG 69-01) demonstrated BCNU and radiation therapy superior to radiation therapy alone.28 Similar results were obtained in studies using lomustine (CCNU).29,30
Given the significant hematologic toxicity observed with nitrosoureas and the ease of use of newer chemotherapies, like temozolomide, nitrosoureas had fallen out of favor. However, a renewed interest has occurred over the last few years, after two randomized clinical trials using lomustine as their control arm failed to meet efficacy endpoints. A recently conducted phase III open-label trial comparing the efficacy and safety of enzastaurin, an oral small-molecule serine/threonine kinase inhibitor of the PKC beta and AKT pathways, versus lomustine in patients with recurrent GBM was terminated early after futility analyses demonstrated a median progression-free survival (PFS) of 1.5 months for enzastaurin versus 1.6 months for lomustine, and a median overall survival (OS) of 6.6 months versus 7.1 months, respectively.16 A second randomized, phase III, placebo-controlled, partially blinded clinical trial conducted to determine the efficacy of cediranib, an oral pan-vascular endothelial growth factor (VEGF) receptor (VEGFR) tyrosine kinase inhibitor, either as monotherapy or in combination with lomustine versus lomustine monotherapy in patients with recurrent GBM, reported a median PFS for the cediranib (30 mg) monotherapy arm, the cediranib (20 mg) plus lomustine arm, and the lomustine arm of 92 days, 125 days, and 82 days, respectively. Furthermore, median OS was 8.0 months, 9.4 months, and 9.8 months, respectively.17
Carmustine wafers (Gliadel)
Locoregional therapies are promising approaches because they allow one to circumvent the BBB, minimize systemic toxicity, and concentrate therapy at the primary tumor site – the site of tumor recurrence in most malignant glioma patients.31,32 Carmustine wafers, controlled-release, biodegradable polymers releasing BCNU, were the first approved locoregional therapy for newly diagnosed malignant gliomas and recurrent GBMs.33 Double-blind, randomized, placebo-controlled studies using carmustine wafer implantation in surgically resectable cases provided an 8-week survival benefit and a 2.3-month survival benefit in recurrent GBM and newly diagnosed malignant glioma patients, respectively.34,35
Temozolomide (Temodar)
Temozolomide, an oral agent that crosses the BBB, is an imidazotetrazine derivative of dacarbazine, which spontaneously hydrolyzes to its biologically active form, 3-methyl-(triazen-1-yl)imidazole-4-carboxamide (MTIC). The mechanism of antitumor action is the disruption of DNA replication via methylation at specific residues, including the O6 position of guanine, N7 position of guanine, and N3 position of adenine.
One of the first studies demonstrating the antiglioma activity of temozolomide was a large multicenter phase II trial involving 162 patients with grade 3 anaplastic astrocytoma or anaplastic oligoastrocytomas. Patients were treated with temozolomide at first relapse, following surgery and radiation therapy.36 Objective responses were observed in 35% of patients (8% complete remission and 27% partial remission). An additional 26% of patients had stable disease. Overall, 46% of patients achieved the primary endpoint of 6-month PFS and 24% remained progression-free at 12 months. Median OS was 13.6 months and 12-month survival was 56%. Importantly, there was no significant difference between 6-month PFS in patients who had received prior chemotherapy (nitrosourea-based) versus chemotherapy-naive patients (44% vs. 50%).
Clinical trial results of temozolomide for recurrent GBMs were equally promising. A large randomized phase II study completed by the Temodal Brain Tumor Group compared temozolomide to procarbazine in glioblastoma at first relapse.37 In total, 225 patients were treated, 112 with temozolomide and 113 with procarbazine. PFS at 6 months and 6-month OS were significantly better in temozolomide-treated patients than procarbazine (21% vs. 8%, p < 0.008, and 60% vs. 44%, p < 0.019, respectively).
Temozolomide was also demonstrated to be effective for patients with newly diagnosed malignant glioma.38 Among 33 patients with GBM, complete responses occurred in three patients, partial responses occurred in 14 patients, stable disease was seen in four patients, and 12 patients developed progressive disease. Toxicity included infrequent grade 3 and 4 myelosuppression, constipation, nausea, and headache.
Those promising results were confirmed in a phase III trial conducted by the European Organization for Research and Treatment of Cancer (EORTC) Brain Tumor and Radiotherapy Groups and the National Cancer Institute of Canada (NCIC) Clinical Trials Group, comparing radiation therapy with concomitant and adjuvant temozolomide for newly diagnosed GBM patients versus radiation therapy alone, also known as the “Stupp regimen.”13 Five hundred and seventy-three newly diagnosed GBM patients, between 18 and 70 years, were enrolled on the study. In all, 286 patients received a standard radiation therapy dose of 60 Gy over 6 weeks, and 287 patients received the same radiation therapy regimen in conjunction with 75 mg/m2 of temozolomide orally daily (7 days a week) during radiation therapy, followed by up to six cycles of adjuvant temozolomide (150–200 mg/m2 on days 1–5 of a 28-day cycle). Patients receiving temozolomide received prophylactic treatment against Pneumocystis jiroveci pneumonia during the concomitant radiation therapy and temozolomide period. Patients in the radiation therapy-alone group were allowed to receive temozolomide at the time of disease progression. A median OS of 14.6 months was observed in patients treated with concurrent radiation therapy and temozolomide followed by six cycles of temozolomide, compared to 12.1 months for patients treated with radiation therapy alone. Also, the 2-year survival rate improved from 10.4% for radiation therapy alone to 26.5% in the radiation therapy–temozolomide group.13 No grade 3 or 4 hematologic toxicities were observed in the radiation therapy-alone group. In comparison, in the radiation therapy–temozolomide group, 12 patients (4%) experienced grade 3 or 4 neutropenia and nine patients (3%) had grade 3 or 4 thrombocytopenia. In the adjuvant temozolomide period of the radiation therapy–temozolomide group, 14% of patients had grade 3 or 4 hematologic toxicities (4% grade 3 or 4 neutropenia, 11% grade 3 or 4 thrombocytopenia). In the radiation therapy period, severe infections occurred in six patients (2%) in the radiation therapy-alone group and in nine patients (3%) in the radiation therapy–temozolomide group, while in the adjuvant temozolomide portion, 12 patients (5%) experienced severe infections. Other common non-hematologic toxicities included: moderate to severe fatigue (26% radiation therapy-alone group, 33% radiation therapy–temozolomide group), thromboembolic events (6% radiation therapy-alone group, 4% radiation therapy–temozolomide), pneumonia (2% radiation therapy-alone group, 1% radiation therapy–temozolomide group), and opportunistic infections (one patient in each group). Finally, two patients in the radiation therapy–temozolomide group died of cerebral hemorrhage in the absence of a coagulation disorder or thrombocytopenia.
The group also published the 5-year survival information and reported a 5-year OS of 9.8% for patients treated on the combination arm of radiation therapy with temozolomide versus 1.9% for the radiation therapy arm. They concluded that the benefit of adjuvant temozolomide with radiation therapy lasted throughout 5 years of follow-up.18
Gene methylation is an important cellular mechanism of transcription suppression. O6-methylguanine-DNA-methyltransferase (MGMT) is a critical DNA repair protein, which removes chloroethylation, or methylation damage from the O6 position of DNA guanines, protecting the tumor cells against alkylating and methylating chemotherapeutic agents.39 The presence of MGMT gene methylation predicts for lack of MGMT expression and subsequent temozolomide sensitivity, whereas the absence of MGMT gene methylation (unmethylated MGMT) predicts MGMT expression and potential temozolomide resistance. Analyses of tumor specimens from patients treated on the Stupp trial13 were performed to determine the methylation status of MGMT and its correlation with survival. Patients with MGMT gene methylation who received radiation therapy and temozolomide achieved a median PFS of 10.3 months and a 2-year survival rate of 46%, compared to 5.9-month median PFS and 22.7% 2-year survival rate for the patients having MGMT gene methylation but treated with radiation therapy alone. In comparison, patients with unmethylated MGMT achieved a median PFS of 5.3 months and a 2-year survival rate of 14% for the radiation therapy–temozolomide group and 4.4 months and <2%, respectively, for the group receiving only radiation therapy.40 It was concluded that patients with newly diagnosed GBM and MGMT gene methylation benefited the most from the addition of temozolomide to radiation therapy.40
The promising results of this study have been interpreted by most neuro-oncologists as establishing a new, albeit modestly improved, standard of care for patients with newly diagnosed GBM. However, the “Stupp regimen” has been modified over the years. Most US centers will continue temozolomide beyond the six cycles of adjuvant temozolomide administered in the Stupp trial,13 with most recommending at least 12 cycles of adjuvant temozolomide. Furthermore, most have limited the prophylactic treatment against Pneumocystis jiroveci pneumonia with trimethoprim-sulfamethoxazole (TMP-SMX) to patients necessitating continued high-dose corticosteroids during the concomitant radiation therapy and temozolomide period, given the added hematologic toxicity experienced with TMP-SMX. Finally, it is agreed that the supplemental benefit of the addition of temozolomide to radiation therapy in newly diagnosed GBM patients with MGMT gene methylation40 should not be interpreted as a need to withhold temozolomide from patients with unmethylated MGMT. However, patients with unmethylated MGMT should be encouraged to enroll on clinical trials for newly diagnosed GBMs.
The use of protracted daily temozolomide has been evaluated as a potential way to overcome an unmethylated MGMT. Depletion of MGMT activity in peripheral blood mononuclear cells, but not in actual tumor cells, has been shown with protracted temozolomide,41 suggesting the possibility of reversing temozolomide resistance and restoring chemosensitivity, resulting in cytotoxic damage in previously resistant GBM. Also, smaller daily doses of chemotherapeutic agents have been shown to inhibit endothelial cell recovery and to restrict the mobilization and activity of bone marrow-derived circulating endothelial precursors, thus suggesting that low-dose chemotherapy delivered on a continuous basis may also induce an antiangiogenic effect.42,43 A final argument for the use of protracted daily temozolomide is the dose intensity obtained. The conventional adjuvant 5-day temozolomide regimen delivers 750 mg/m2 to 1000 mg/m2 of temozolomide per 28-day cycle. In contrast, protracted daily temozolomide at 50 mg/m2/day offers a dose of 1400 mg/m2 per 28-day period, which represents 1.4–1.9 more temozolomide than is obtained with the conventional 5-day temozolomide regimen. In a trial of recurrent GBM patients who progressed after 5-day temozolomide, 15% of the patients benefitted from the transition to daily temozolomide at 50 mg/m2/day.44 In comparison, in newly diagnosed GBM patients, the use of dose-dense temozolomide at 75–100 mg/m2 on days 1–21 of a 28-day cycle failed to show improved efficacy when compared to the standard temozolomide dosing in the adjuvant setting of 150–200 mg/m2 on days 1–5 of a 28-day cycle.45
Temozolomide is continually being evaluated, in the newly diagnosed and recurrent setting, in multiple clinical trials in combination with a wide variety of therapeutic agents, including other chemotherapeutic agents, cell signaling inhibitors, antiangiogenic agents, immunotherapies, and therapeutics designed to overcome mediators of chemotherapy resistance. Results of a vaccine directed to the epidermal growth factor variant III mutation in combination with temozolomide in newly diagnosed GBM patients are reviewed in Chapter 5.
Antiangiogenic therapy
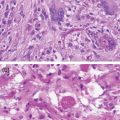
Vascular proliferation, or neoangiogenesis, is a histopathological characteristic of malignant gliomas.46 One attractive therapeutic target for many neoplasms is VEGF, the principal mediator of tumor angiogenesis. Malignant gliomas overexpress VEGF, the levels of which correlate directly with tumor vascularity and grade, and inversely with prognosis.47–50 Tumor-associated endothelial cells express VEGFR2, creating a paracrine loop of angiogenic activation, indicating that VEGF and its receptors are important therapeutic targets.49,51
Bevacizumab (Avastin)
Bevacizumab, a humanized murine monoclonal antibody, binds VEGF-A52,53 and prevents interaction and activation of VEGFR tyrosine kinases VEGFR1 and VEGFR2.54 Given in combination with conventional chemotherapy, bevacizumab significantly improves the survival of patients with metastatic colorectal and lung cancer55,56 and PFS in patients with breast cancer.57 Bevacizumab, with irinotecan, has been approved by the FDA for colorectal cancer, and as a first-line treatment for non-small cell lung cancer in combination with carboplatin and paclitaxel. Encouraging radiographic responses and PFS were observed in malignant glioma patients exposed to bevacizumab when used in combination with irinotecan,58 which led to the first FDA-approved phase II trial, led by the Duke team.59 We observed a radiographic response rate of 63% (14/23 World Health Organization [WHO] grade IV malignant glioma and 6/9 WHO grade III malignant glioma) and a 6-month PFS of 32% in all patients.59 Due to the encouraging radiographic response observed, the initial trial was expanded to include a total of 68 patients with recurrent malignant glioma. Among the 68 patients enrolled, 35 patients had a pathological diagnosis of WHO grade IV malignant glioma, while 33 were WHO grade III malignant glioma patients. For the 35 recurrent WHO grade IV malignant glioma patients, 6-month PFS was 46% (95% confidence interval [CI], 32–66%) and 6-month OS was 77% (95% CI, 64–92%). Twenty of the 35 patients (57%; 95% CI, 39–74%) had at least a partial response. One patient developed a CNS hemorrhage and four patients developed thromboembolic complications (deep venous thrombosis and/or pulmonary emboli).60 Similarly, among 33 recurrent anaplastic glioma patients, 6-month PFS was 55% (95% CI, 36–70%), 6-month OS was 79% (95% CI, 61–89%), and 20 patients (61%) had at least a partial response. Significant adverse events were infrequent and included one patient with symptomatic CNS hemorrhage and one patient who developed thrombotic thrombocytopenic purpura. The patient with CNS hemorrhage required hospitalization and high-dose dexamethasone, but made a full recovery following rehabilitative therapy. The patient who developed thrombotic thrombocytopenic purpura remains on peritoneal dialysis without sign of disease progression more than 8 years later.61
Those encouraging results were followed by a phase II, randomized, multicenter, non-comparative clinical trial of bevacizumab alone or in combination with irinotecan for GBM patients at first or second recurrence, the BRAIN trial.15 Eighty-five patients were randomized to the bevacizumab-alone group and 82 to the combination of bevacizumab plus irinotecan group. Patients in the bevacizumab-alone group were allowed to receive the combination of bevacizumab and irinotecan at the time of disease progression at the discretion of the investigator. Median OS were comparable with 9.2 months (95% CI, 8.2–10.7 months) for the bevacizumab-alone group and 8.7 months (95% CI, 7.8–10.9 months) for the combination group. However, the 6-month PFS was higher in the combination group (50.3%; 95% CI, 36.8–63.9%) compared to the bevacizumab-alone group (42.6%; 95% CI, 29.6–55.5%). Grade 3 and higher toxicities were greater in the combination group (65.8% vs. 46.4% for the bevacizumab-alone group), but grade 5 adverse events happened more frequently in the bevacizumab-alone group (2.4% vs. 1.3% for the combination group).15 The group also reported a median OS at 30 months of 11% for the bevacizumab-alone group versus 16% for the bevacizumab plus irinotecan group.62
Following review of the radiographic response rates and quality-of-life data reported by the BRAIN trial15 and a phase II trial of single-agent bevacizumab followed by bevacizumab and irinotecan in recurrent GBM patients conducted by the National Institutes of Health,63 bevacizumab as a single agent was granted accelerated approval by the FDA in May of 2009 for GBM patients at the time of disease progression or recurrence.
Following the accelerated approval of bevacizumab for recurrent GBM patients and given preliminary studies showing the potentiation of radiation therapy by the inhibition of VEGFR signaling in GBM models,64,65 several single-institution as well as multicenter studies have been completed to evaluate the addition of bevacizumab to radiation therapy and temozolomide for newly diagnosed GBM patients. Two phase III randomized multicenter studies were published in 2014.66
The Avastin in Glioblastoma (AVAglio) study (BO21990) was a randomized, double-blind, placebo-controlled trial sponsored by F. Hoffmann–La Roche and designed by the AVAglio steering committee.66 The study had dual primary objectives: PFS and OS. Patients were enrolled in two arms, the first arm being the standard of care, also known as the “Stupp regimen,” whereas the second arm included the standard of care plus bevacizumab at 10 mg/kg intravenously every 2 weeks during radiation therapy and temozolomide and the six cycles of adjuvant temozolomide, followed afterward by bevacizumab at 15 mg/kg every 3 weeks. There was no crossover planned on this study. A total of 458 patients were enrolled on the treatment arm and 463 patients were enrolled on the standard-of-care arm. A median PFS of 10.6 months was observed for the treatment arm versus 6.2 months for the standard-of-care arm, with a hazard ratio of 0.64. The median OS was similar in both arms at 16.8 months for the bevacizumab arm and 16.7 months in the placebo arm (stratified hazard ratio for death with bevacizumab, 0.88; 95% CI, 0.76–1.02; p = 0.10). However, the improvement in quality of life remained stable or improved on the treatment arm for 8 months versus 4 months for the control group and the ability to maintain a Karnofsky performance scale ≥ 70 for 9 months versus 6 months, respectively, which was statistically significant. It is also important to note that, in malignant glioma patients, one of the major impacts on their quality of life is the significant side effects due to the chronic use of corticosteroids. On the study, it was shown that 66% of patients on the treatment arm were able to discontinue steroids versus 47% for the control arm. Once patients came off steroids, patients on the treatment arm remained off steroids for a median of 12.3 months versus 3.7 months only for the control arm. Toxicities were acceptable, with 4.5% of grade 5 adverse events on the treatment arm versus 2.7% on the control arm. The risk of intracranial hemorrhage was similar, at 2.6% versus 2.2%, and the risk of deep venous thrombosis was in fact lower, at 7.8% versus 9.6%, respectively.
One of the other difficulties in neuro-oncology is the occurrence of pseudoprogression, meaning an increase in vasogenic edema and degree of contrast enhancement following radiation therapy, making it difficult to differentiate between disease progression and radiation therapy effect.67 Furthermore, it has been demonstrated that, for patients with MGMT methylation, the presence of an increase in contrast enhancement following radiation therapy, or pseudoprogression, is suggestive of an improvement in prognosis.68 It is thus important to determine if the changes suggestive of disease progression following radiation therapy are true or only due to treatment effect. If pseudoprogression is misdiagnosed as true disease progression, patients could be enrolled on a trial for recurrent disease and falsely improve the results of that trial.67,68 In the AVAglio trial,66 it was shown that the risk of pseudoprogression decreased from 10% to 2% with the addition of bevacizumab to the “Stupp regimen.” In conclusion, the addition of bevacizumab to the “Stupp regimen” did not improve OS in the AVAglio trial, but improved PFS and allowed maintenance of baseline quality of life and performance status. It should be noted that, despite the fact that no crossover was planned for this trial and that the trial had been statistically designed to allow a crossover of up to 20%, a total of 144 patients (31.1%) on the placebo arm received bevacizumab at the time of progression.66
The second trial11 was completed by the Radiation Therapy Oncology Group (RTOG), the North Central Cancer Treatment Group (NCCTG), and the Eastern Cooperative Oncology Group (ECOG). They conducted a randomized, placebo-controlled, double-blind, phase III trial, RTOG 0825. In this trial, newly diagnosed GBM patients initiated radiation therapy (60 Gy) and daily temozolomide 75 mg/m2/day. Patients able to continue radiation therapy and temozolomide at week 4 of radiation therapy were randomized to either the bevacizumab arm or the placebo arm, which began on week 4 of radiation therapy and continued in combination with temozolomide for up to 12 cycles of adjuvant chemotherapy. At disease progression, the study was unblinded and bevacizumab therapy could be initiated or continued. The trial had PFS and OS as co-primary endpoints. A total of 978 patients were registered into the trial and 637 patients underwent randomization. There was no significant difference in the duration of OS between the bevacizumab arm and the placebo arm, with a median OS of 15.7 months and 16.1 months, respectively (hazard ratio for death in the bevacizumab arm of 1.13). PFS was longer in the bevacizumab arm at 10.7 months versus 7.3 months for the placebo arm (hazard ratio for progression or death was 0.79). Side effects, with a modest increase in frequency in the bevacizumab arm, included hypertension, thromboembolic events, intestinal perforation, and neutropenia. In contradiction with the AVAglio trial,66 an increase in symptom burden, a worse quality of life, and a decline in neurocognitive function were more frequent in the bevacizumab arm. The group concluded that first-line use of bevacizumab did not improve OS in patients with newly diagnosed GBM. The PFS was prolonged similarly to what was observed in the AVAglio trial,66 but in this case, did not reach statistical significance. In conclusion, it is to note that at the time of disease progression on the RTOG 0825 trial,11 39 patients (25.2%) on the bevacizumab arm continued on bevacizumab and 86 patients (48.3%) on the placebo arm initiated bevacizumab.
The lack of survival advantage, similar increase in PFS (which did not meet statistical significance for the RTOG 082511) and discrepancy in quality of life and neurocognitive data of the two phase III trials11,66 evaluating the addition of bevacizumab to the standard of care for newly diagnosed GBM patients brought much publicity and controversy. Unfortunately, both trials are afflicted by a high crossover rate, among other limitations. Despite those results, the neuro-oncology field continues to agree that, as stated by Dr. Fine69: “despite its limitations, bevacizumab remains the single most important therapeutic agent for GBM since temozolomide. Ongoing and future trials will better define how and when it should be used in this population of patients for whom so few treatment options currently exist.”
Multiple chemotherapies and tyrosine kinase inhibitors were studied in combination with bevacizumab in recurrent glioblastoma patients (for example, temozolomide, etoposide, carboplatin, erlotinib, vorinostat). Unfortunately, none of them showed a significant improvement in PFS, OS, or radiographic response rate comparatively to bevacizumab monotherapy or bevacizumab in combination with irinotecan.62 However, those combinations remain possible treatment options depending on the side-effect profile experienced by patients with different therapies. Furthermore, some data suggest that these combination regimens could, up to a certain point, salvage patients who have previously experienced disease progression on bevacizumab.70 More recently, the BELOB trial,71 an open-label, multicenter, randomized three-arm phase II trial of adult glioblastoma patients at the time of first recurrence, demonstrated a median OS of 8 months for the bevacizumab monotherapy arm, 8 months for the lomustine monotherapy arm, and 12 months for the bevacizumab plus lomustine arm. Due to hematologic toxicity on the combination arm of bevacizumab and lomustine, the lomustine had to be dose-reduced from 110 mg/m2 to 90 mg/m2 in that arm.71 Furthermore, the BELOB trial demonstrated that bevacizumab, whether it was administered or not with lomustine, did not negatively impact the health-related quality of life of recurrent glioblastoma patients.72 A phase III trial of bevacizumab plus lomustine versus lomustine monotherapy is currently enrolling (EORTC 26101: NCT01290939).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree