Chemoradiation plays an important role in management of locally advanced gastrointestinal tumors. This article reviews data regarding chemoradiation for tumors of the upper gastrointestinal tract. For esophageal and gastroesophageal junction cancers, chemoradiation is standard of care in the preoperative setting. In gastric cancer, 2 standards have emerged: definitively treating with perioperative chemotherapy alone and using chemoradiation postoperatively. For pancreatic cancer, the benefit of radiation is less well defined. The future of treatment sites lies in trials evaluating new chemotherapy regimens, alternative systemic therapies, and different radiation fractionation schema. Because care of these patients is complex, multimodality team evaluation before treatment is encouraged.
Key points
- •
The management of localized gastrointestinal (GI) cancers with definitive intent typically includes multimodality therapy with some combination of surgery, chemotherapy, and radiation.
- •
In esophageal and gastroesophageal junction (GEJ) cancers, concurrent chemoradiation should be used both in the preoperative setting and the definitive setting.
- •
Surgery is the mainstay of treatment of gastric cancer, and adjuvant therapy with chemotherapy alone and with chemoradiation are both acceptable standards.
- •
The role of radiation in pancreatic cancer is controversial, and there are mixed data regarding the role of chemoradiation in both resectable and locally advanced cases.
- •
Patients with a newly diagnosed GI cancer should be evaluated by a multidisciplinary team to optimize treatment plan and outcomes.
Introduction
Chemoradiation plays an important role in the management of many localized GI tumors. In most situations, chemoradiation therapy (CRT) is administered adjuvantly to improve local control and, in some situations, to improve overall survival. In anal cancer, CRT alone is often curative. This review presents the current role of CRT in the multidisciplinary management of localized esophageal, gastric, and pancreatic cancers and discusses future directions for the adjuvant treatment of these selected GI malignancies.
Introduction
Chemoradiation plays an important role in the management of many localized GI tumors. In most situations, chemoradiation therapy (CRT) is administered adjuvantly to improve local control and, in some situations, to improve overall survival. In anal cancer, CRT alone is often curative. This review presents the current role of CRT in the multidisciplinary management of localized esophageal, gastric, and pancreatic cancers and discusses future directions for the adjuvant treatment of these selected GI malignancies.
Esophageal and gastroesophageal cancers
CRT for esophageal and GEJ cancers is currently used preoperatively for the surgically resectable population as well as definitively in inoperable patients.
Current State: Locally Advanced, Resectable Cancer
The rationale for preoperative therapy in locally advanced, resectable esophageal cancers, American Joint Committee on Cancer 2010 stages IB–III, stems from a high margin positivity rate in the range of 40% to 50%, which subsequently contributes to poor survival. Until recently, however, the data have been mixed regarding the efficacy of this preoperative approach.
Neoadjuvant Chemoradiation
Many studies have evaluated the role of preoperative CRT, referred to as the trimodality approach, versus surgery alone for esophageal and GEJ cancers. Walsh and colleagues originally reported a survival advantage to preoperative CRT compared with surgery alone. The study has been criticized, however, for unexpectedly poor outcomes in the surgery-alone arm (3-year overall survival rate of 6%), possibly due to lack of uniform staging with CT among all patients. Furthermore, subsequent studies failed to consistently confirm a statistically significant benefit to preoperative CRT as opposed to surgery alone ( Table 1 ).
| Study | N | Randomization | Pathologic CR | 3-Y Survival | P Value |
|---|---|---|---|---|---|
| Walsh et al, 1996 | 113 | S CRT → S | 25% | 6% 32% | P = .01 |
| Bosset et al, 1997 | 282 | S CRT → S | 26% | 37% a 39% a | P = .78 |
| Urba et al, 2001 | 100 | S CRT → S | 28% | 16% 30% | P = .15 |
| Burmeister et al, 2005 | 256 | S CRT → S | 16% | 36% a 38% a | P = .57 |
The Cancer and Leukemia Group B (CALGB) also attempted to answer the question of whether or not preoperative CRT improved outcomes and reported an improvement in 5-year overall survival rates with the use of CRT from 16% to 39% ( P = .002). This study was small, however, and closed early due to poor accrual, at only 56 patients. The interpretation of the available data on preoperative therapy in esophageal cancer thus was still considered controversial.
The recently published Chemoradiotherapy for Esophageal Cancer Followed by Surgery Study (CROSS) has provided more convincing data suggesting a benefit to preoperative therapy for locally advanced esophageal and GEJ cancers. This study, the largest randomized controlled trial in esophageal cancer to date, randomized 366 patients to CRT followed by surgery versus surgery alone. This study used weekly carboplatin and paclitaxel as the concurrent preoperative chemotherapy, as opposed to cisplatin-based and 5-fluorouracil (5-FU)–based regimens that were administered in investigations mentioned above. Radiation was prescribed at 41.4 Gy in 23 daily fractions. Of the 366 patients, the majority of patients had adenocarcinoma (266 patients, 75%), with most tumors located in the distal esophagus (58%) or at the GEJ (24%). A pathologic complete response was achieved in 29% of patients who underwent resection after CRT; however, pathologic complete response was more likely to be seen among patients with squamous cell carcinoma than adenocarcinoma (49% vs 23%, P = .008). Treatment with preoperative CRT yielded a significantly higher rate of R0 resection (92% vs 69%, P <.001) and a lower rate of nodal positivity (31% vs 75%, P <.001) compared with the surgery-alone group. With a median follow-up of 45.4 months, preoperative CRT more than doubled the median survival rate compared with surgery alone, at 49 months versus 24 months ( P = .003), and the 5-year overall survival rate also significantly improved, at 47% versus 34%. There were no differences in postoperative complications between the 2 arms.
Chemotherapy or Chemoradiation?
Study groups have also looked at the use of preoperative chemotherapy followed by surgery versus surgery alone. In a study by the Radiation Therapy Oncology Group (RTOG) and Intergroup (INT), the RTOG 8911/INT 133 trial, 467 patients with resectable disease were randomized to surgery alone versus preoperative chemotherapy with 3 cycles of cisplatin/5-FU. The pathologic complete response rate was disappointing, at 2.5%, and ultimately there was no difference in survival between the 2 groups. The Medical Research Council Esophageal Cancer Working Group also published a study looking at preoperative chemotherapy, randomizing patients to 2 cycles of cisplatin/5-FU before surgery versus surgery alone. Although preoperative chemotherapy in this trial improved the 5-year overall survival rate from 17% to 23%, 9% of patients in both arms also received preoperative radiation, thus making the results difficult to interpret.
Stahl and colleagues looked specifically at the delivery of preoperative chemotherapy versus preoperative CRT in patients with GEJ tumors. In this study, 126 patients were randomized to receive either preoperative chemotherapy with induction cisplatin/5-FU/leucovorin for 3 cycles versus the same induction chemotherapy regimen for 2 cycles followed by preoperative CRT (30 Gy in 15 fractions administered with concurrent cisplatin and etoposide). Treatment with preoperative CRT had a significantly higher probability of pathologic complete response (15.6% vs 2.0%, P = .03) and node negativity (64% vs 38%, P = .01) at the time of resection. The rate of patients without local tumor progression was also better with CRT (76.5% vs 59% at 3 years, P = .06). Although this study closed early due to poor accrual, there was a trend toward a better survival rate with CRT (47% vs 28% at 3 years, P = .07), suggesting the benefit of preoperative CRT.
With the CROSS data now available, the standard of care in patients with locally advanced esophageal or GEJ cancer who are considered surgical candidates has been established as preoperative CRT with carboplatin and paclitaxel followed by surgery. Although the CROSS delivered 41.1 Gy of radiation, in the United States 50.4 Gy has been adopted as standard preoperative dose, per the trial design of CALGB 9781. The most appropriate preoperative radiation dose for resectable disease has yet to be clearly defined.
Current State: Inoperable Cancer
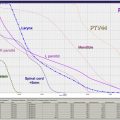
In esophageal or GEJ cancer, patients may be deemed inoperable due to either unfavorable anatomy/local extent of the tumor or medical comorbidities. The RTOG 85-01 study demonstrated that treatment with CRT was superior to radiation alone for this population, with a 5-year overall survival rate of 27% versus 0%. Once definitive CRT was established as superior, RTOG 94-05/INT 0123 examined radiation dose escalation in this setting, comparing the conventional 50.4-Gy CRT with CRT at a higher dose of 64.8 Gy. For the 218 eligible patients, there was no significant difference in median survival (13.0 vs 18.1 months), 2-year survival rate (31% vs 40%), or locoregional control (56% vs 52%) between the high-dose and standard-dose arms. This trial was closed early to accrual after interim analysis, due to unexpectedly higher mortality seen in the higher-dose treatment arm (10% in the higher-dose arm vs 2% in the standard arm). The majority of the treatment-related deaths in the higher-dose arm occurred, however, before reaching the standard dose of 50.4 Gy, calling into question whether the treatment-related toxicity was due to the higher treatment dose. Because of these results, 50.4 Gy has been adopted as the standard radiation CRT dose for medically inoperable esophageal or GEJ cancer.
When definitive CRT is delivered in the initially unresectable setting, there may be situations where this treatment converts the disease to resectable status. More recent studies, mostly restricted to squamous cell carcinoma, have shown an equivalence of CRT to CRT followed by surgery in terms of overall survival. Surgery seems to offer a local control benefit, however, albeit with a higher treatment-related death rate.
Although it is currently accepted that with inoperable esophageal or GEJ cancer definitive CRT is the treatment of choice, ongoing trials are assessing the optimal chemotherapy regimen for CRT. A recent study of CRT with leucovorin/5-FU/oxaliplatin (FOLFOX) versus CRT with cisplatin/5-FU in the inoperable population showed no difference in survival but had lower treatment-related death rates with FOLFOX. Ultimately, in light of the disappointing outcomes with CRT as definitive therapy, both the optimal chemotherapy type and radiation dose remain unanswered questions.
Future Directions
Although cure rates for esophageal and GEJ cancers have improved over the years, success rates are still modest and further improvements are warranted. As such, the role of targeted agents is under active investigation.
HER2 is a member of the HER receptor family and a transmembrane glycoprotein. It has long been established in breast cancer that, although HER2 overexpression confers a worse prognosis, treatment with trastuzumab (a humanized monoclonal antibody against HER2) yields improved survival. It has been recently shown that HER2 is also overexpressed in 20% of GEJ and gastric cancers. Based on encouraging evidence that trastuzumab improves outcomes in GEJ cancers, the RTOG has recently initiated a randomized trial, RTOG 10-10, to examine the utility of trastuzumab with CRT in patients with resectable, locally advanced, HER2-positive adenocarcinoma of the esophagus and GEJ.
Epidermal growth factor receptor (EGFR) is, like HER2, a transmembrane protein that when overexpressed portends a poor prognosis. Activation of the EGFR extracellular domain by ligand binding relays growth and division signals to the cell. Cetuximab is a monoclonal antibody directed against EGFR, blocking its signaling. There have been reports of overexpression of EGFR in 30% to 90% of esophageal and gastric cancers and several phase II studies have assessed the role of cetuximab with CRT for esophageal cancers. Although these trials have shown encouraging pathologic complete response rates of approximately 30%, there have been conflicting data on safety. The Eastern Cooperative Oncology Group (ECOG) 2205 study, which evaluated neoadjuvant CRT with cetuximab and 5-FU/oxaliplatin, closed early after an excessive number of early treatment-related deaths: 4 of 18 patients died postoperatively of acute respiratory distress syndrome. The RTOG also initiated a randomized phase III trial, RTOG 04-36, assessing the potential benefit of adding cetuximab to cisplatin/paclitaxel and 50.4 Gy of radiation in inoperable esophageal cancer. After a planned interim analysis in the spring of 2012, however, the study failed to show superiority in survival with cetuximab and was closed to further enrollment.
The role of targeted therapies with CRT for esophageal cancer continues to evolve. Although HER2 may prove an effective target for esophageal and GEJ cancers, it is overexpressed in only a minority of patients. The disappointing early data with anti-EGFR therapy makes it unlikely that this strategy will be further developed in the setting of esophageal or GEJ cancer. Alternative biologic pathways, such as HGF/MET, Hsp90, and Hedgehog, may represent promising new targets to further explore.
In addition to targeted therapy, the United States is investigating the utility of positron emission tomography scans to assess response and direct adjuvant therapy in patients with esophageal cancer and with GEJ cancer who are receiving CRT. This interest is based on data from Germany that demonstrate the usefulness of early metabolic response evaluation. The CALGB 80803 phase II trial assessing pathologic complete response rate in positron emission tomography scan nonresponders after induction CRT is currently open to accrual.
Gastric cancer
Surgery has been, and continues to be, a critical component in the treatment of locally advanced American Joint Committee on Cancer 2010 stages IB–III gastric cancer. Historically, however, despite aggressive surgery, gastric cancer is associated with high locoregional and distant metastatic failure rates. How and when to use chemotherapy or CRT remain topics of controversy for the adjuvant management of gastric cancer.
Current State
Surgery is the cornerstone of treatment of nonmetastatic gastric cancer. The extent of surgical resection for gastric cancers depends on the location of the primary tumor. In addition to removal of the primary disease, the associated lymph node dissection can range in extensiveness. The D1 dissection involves complete removal of the perigastric lymph nodes, whereas D2 dissection also removes of the nodes around the branches of the celiac trunk. Despite meticulous surgical technique and investigation into the safest and most effective type of lymph node dissection, in Western series, the overall survival rates with surgery alone are still poor, ranging from approximately 20% to 40%. These unsatisfactory outcomes have prompted studies evaluating adjuvant therapy in the management of patients with locally advanced gastric cancer.
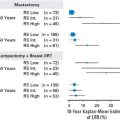
To date, research groups have examined both adjuvant chemotherapy and adjuvant CRT. In the United States, adjuvant therapy has been informed by the INT-0116 trial. In this study, 556 patients were randomized after surgery to adjuvant chemotherapy and CRT versus observation. The adjuvant arm administered 5-FU for 1 cycle, followed by CRT to 45 Gy with concurrent 5-FU, which was followed by 2 additional cycles of 5-FU. The 3-year overall survival rate was significantly improved with adjuvant CRT, at 50% versus 41% ( P = .005). This study was criticized, however, because 54% of patients had a D0 lymph node dissection (meaning not all of the perigastric nodes were removed). This raises the question of whether the adjuvant therapy was only compensating for inadequate surgery. Also, the radiation field design was deemed inadequate and necessitated modification in more than half of the patients in the adjuvant arm, highlighting the need for high-quality radiation field design.
During the same period that the INT-0116 trial was accruing patients for adjuvant CRT, the Europeans were investigating the use of perioperative chemotherapy. The results of this were published in the medical research council adjuvant gastric infusional chemotherapy (MAGIC) trial. Patients were treated either with perioperative chemotherapy using a multiagent chemotherapy regimen of epirubicin/cisplatin/5-FU (ECF) or with surgery alone. A 5-year survival benefit was achieved in the perioperative chemotherapy arm of 36% versus 23% ( P = .009).
Until recently, there were no published randomized comparisons between postoperative CRT and perioperative chemotherapy, and both the INT-0116 and the MAGIC regimens have been considered acceptable standards. More recently, the adjuvant chemoradiation therapy in stomach cancer (ARTIST) trial was published, which randomized D2-resected gastric cancers to adjuvant multiagent chemotherapy versus adjuvant chemotherapy plus CRT. The chemotherapy-alone arm consisted of capecitabine/cisplatin for 6 cycles. The CRT arm administered capecitabine/cisplatin for 2 cycles, followed by CRT with 45 Gy/capecitabine and 2 additional cycles of capecitabine/cisplatin. In this study, there was no significant difference in the disease-free survival rate at 3 years (74% with adjuvant chemotherapy vs 78% with adjuvant chemotherapy plus CRT, P = .0862). In a subgroup analysis of patients with positive lymph nodes (which included 85% and 88% of patients in each arm), however, the 3-year disease-free survival rate was improved with the addition of CRT (72% vs 78%, P = .0365). Although this result suggests that patients with more extensive locoregional disease at the time of surgery benefit from additional local therapy with radiation, locoregional recurrences were not statistically different between the 2 study arms (8% vs 5%, P = .3533). The investigators of this trial indicated they are planning a follow-up study to specifically explore the utility of CRT in node-positive gastric cancer patients.
For the postoperative adjuvant CRT approach, trials continue to examine the optimal chemotherapy regimen. Fuchs and colleagues, in the randomized phase III CALGB 80101 trial, randomized patients with resected gastric or GEJ cancers to adjuvant therapy that either included chemotherapy with 5-FU/leucovorin or ECF, administered before and after CRT with 45 Gy/5-FU. They have, thus far, found no statistically significant differences between the chemotherapy regimens in terms of median or 3-year overall survival.
Ultimately, the optimal strategy for adjuvant therapy in resected locally advanced gastric cancer is under debate. The INT-0116 trial showed that single-agent chemotherapy with radiation was better than observation, and the MAGIC study proved that perioperative multiagent chemotherapy alone was better than observation. The most recent randomized study, the capecitabine and oxaliplatin adjuvant study in stomach Cancer (CLASSIC) trial, evaluated adjuvant-only multiagent chemotherapy (with capecitabine/oxaliplatin) versus observation and also demonstrated a 3-year disease-free survival benefit to chemotherapy. The ARTIST study failed to definitely prove, however, that, in the setting of multiagent chemotherapy, adding radiation further improved outcomes. Given the ARTIST subgroup analysis that indicated radiation was beneficial in node-positive patients, the tendency, at least in the United States, is still to use both chemotherapy and radiation in the adjuvant setting.
Future Directions
Given the recent randomized controlled trials on adjuvant therapy, there remains uncertainty on the optimal adjuvant management for resected gastric cancer. Open questions include the optimal chemotherapy regimen and the role of radiation therapy in the setting of perioperative multiagent chemotherapy. The Dutch chemoradiotherapy after induction chemotherapy in cancer of the stomach (CRITICS) study is a randomized trial that is examining perioperative epirubicin/cisplatin/capecitabine (ECX) chemotherapy versus preoperative ECX and postoperative CRT. Results of this trial may help answer some of these questions. Furthermore, given that large radiation fields are necessary in the postoperative setting, there is increasing interest in using radiation preoperatively. Preoperative radiation may reduce the toxicity associated with CRT, be associated with improved compliance to the completion of therapy as prescribed, improve the complete resection rate, and, importantly, also allow for the further development of targeted therapies in gastric cancer.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree