The standard adjuvant treatment of cT3 and/or N+ rectal cancer is preoperative chemoradiation. However, there are many controversies regarding this approach. These controversies include the role of short course radiation, whether postoperative adjuvant chemotherapy is necessary for all patients, and if the type of surgery following chemoradiation should be based on the response rate. More accurate imaging techniques and/or molecular markers may help identify patients with positive pelvic nodes to reduce the chance of overtreatment with preoperative therapy. Will more effective systemic agents both improve the results of radiation, as well as modify the need for pelvic radiation? These questions and others remain active areas of clinical investigation.
The standard treatment of T3 and/or N+ rectal cancer is chemoradiation (CMT). When fluorouracil (5-FU) is used concurrently with CMT, continuous infusion (CI) is the standard. As an alternative, capecitabine can be substituted for CI 5-FU. However, if the ongoing NSABP R-04 trial, which is comparing preoperative CMT with CI 5-FU with capecitabine (with or without oxaliplatin), reveals that capecitabine is inferior this approach would need to be reevaluated.
The regimen used for the adjuvant chemotherapy alone component of treatment is different. Based on the efficacy shown in patients with stage III colon cancer, the combination of CI 5-FU plus oxaliplatin (FOLFOX) has replaced CI 5-FU as a standard postoperative regimen. Other agents such as irinotecan and bevacizumab have not improved survival in stage III colon cancer and therefore are not used in the adjuvant management of rectal cancer.
In contrast to adjuvant colon cancer in which 3-year and possibly 2-year disease-free survival predicts for 5-year survival, the INT 0114 postoperative CMT rectal adjuvant trial showed that local control and survival continue to decrease beyond 5 years. At 7 years local failure rate was 17% and the survival was 56% compared with 14% and 64%, respectively, at 5 years. Both surgeons and hospitals with higher volumes of rectal cancer surgery have improved outcomes compared with those with lower volumes.
Two randomized trials of preoperative versus postoperative CMT for clinically resectable rectal cancer have been performed; NSABP R0-3 and the German CAO/ARO/AIO 94. The German trial complete the planned accrual of more than 800 patients and randomized patients with uT3/4 and/or LN+ rectal cancers less than 16 cm from the anal verge to preoperative CMT (with CI 5-FU weeks 1 and 5) versus postoperative CMT. Patients were stratified by surgeon and all underwent total mesorectal excision (TME). Compared with postoperative CMT, patients who received preoperative therapy had a significant decrease in local failure (6% vs 15%, P = .006), acute toxicity (27% vs 40%, P = .001), chronic toxicity (14% vs 24%, P = .012), and in those 194 patients judged by the surgeon before treatment to require an abdominoperineal resection (APR), a significant increase in sphincter preservation (39% vs 20%, P = .004). With a median follow-up of 40 months there was no difference in 5-year survival (74% vs 76%). A subsequent analysis revealed that the treatment center, schedule, and gender were independent prognostic factors for local control.
The NSABP R-03 accrued only 267 of a planned 900 patients with cT3-4 rectal cancer. Patients received induction chemotherapy followed by conventional CMT and were randomized to receive it either preoperatively or postoperatively. TME was not required and some patients underwent a local excision.
Compared with postoperative therapy, patients who received preoperative therapy had a significant improvement in 5-year disease-free survival (65% vs 53%, P = .011) and a borderline significant improvement in 5-year overall survival (75% vs 66%, P = .065). There was no difference in 5-year local recurrence (11%). There was a corresponding higher incidence of grade 4+ toxicity (33% vs 23%) but the incidence of grade 3+ toxicity was lower (41% vs 50%). Based on a prospective office assessment by the operating surgeon, there was no improvement in sphincter preservation (48% vs 39%).
The NSABP results are opposite to the German trial and are likely because only 267 of the 900 planned patients were accrued, thereby limiting the statistical power to detect differences. Therefore, based on the German CAO/ARO/AIO 94 randomized trial, most patients now receive preoperative CMT.
Clinical staging of rectal cancer
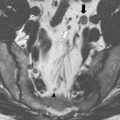
Transrectal ultrasound and high-resolution magnetic resonance imaging (MRI) are the most accurate tools in predicting T stage of rectal cancers. In the United States, ultrasound is used most commonly, whereas in many European countries high-resolution MRI is preferred. High-resolution MRI also allows for identification of patients likely to have close or positive radial margins if they underwent initial surgery and therefore are selected to receive preoperative therapy.
The overall accuracy in predicting T stage is approximately 50% to 90% with ultrasound or high-resolution MRI and 50% to 70% with computed tomography (CT) or conventional MRI. [ 18 F]Fluorodeoxyglucose (FDG)-positron emission tomography (PET) may be more accurate compared with CT for identification of metastatic disease. The use of PET to restage patients following preoperative CMT remains controversial.
Identification of positive lymph nodes is more difficult. The overall accuracy in detecting positive pelvic lymph nodes with the techniques outlined earlier is approximately 50% to 75%. The accuracy of MRI is similar to CT; however, it is improved with the use of external and/or endorectal coils. Both CT and MRI can identify lymph nodes measuring 1 cm or greater, although enlarged lymph nodes are not pathognomonic of tumor involvement. The accuracy of ultrasound for the detection of involved perirectal lymph nodes may be augmented if combined with fine needle aspiration. Despite these advances, the ability to accurately predict the pathologic stage following preoperative CMT with MRI, ultrasound, FDG-PET or physical examination remains suboptimal.
After preoperative therapy overstaging is common, especially when there is a fibrotic thickening of the rectal wall. A high level of accuracy has been observed by phased array MRI for differentiating ypT0-2 versus ypT3. Both diffusion-weighted MRI and FDG-PET have been used to monitor therapy response and to predict outcome to preoperative therapy. There is a decrease in standardized uptake value (SUV) on postradiation FDG-PET in responders when compared with nonresponders, but the clinical value of this information remains to be determined.
Approaches to preoperative therapy
There are 2 approaches to preoperative therapy. The first, used most commonly in Northern Europe and Scandinavia, is the short course (25 Gy in 5 fractions). In contrast, most other investigators recommend standard course (50.4 Gy in 28 fractions) combined with concurrent systemic chemotherapy (CMT). The primary reasons for this preference are the lack of sphincter preservation and the inability to safely combine adequate doses of systemic chemotherapy with short course radiation. CMT trials cannot be directly compared with short course radiation trials because they exclude patients with cT1-2 disease. Short course radiation trials include patients with cT1-3 disease.
Bujko and colleagues performed a randomized trial of 2 preoperative approaches. A total of 316 patients with cT3 rectal cancer were randomized to short course radiation followed by surgery versus conventional preoperative CMT followed by surgery. All tumors were above the anorectal ring, TME was performed for distal tumors, and there was no radiation quality control review. There were no significant differences in local control or survival. The incidence of positive circumferential radial margins (CRM+) was lower following CMT compared with radiation alone (4% vs 13%, P = .017). Results from a similar Australian trial are pending.
Approaches to preoperative therapy
There are 2 approaches to preoperative therapy. The first, used most commonly in Northern Europe and Scandinavia, is the short course (25 Gy in 5 fractions). In contrast, most other investigators recommend standard course (50.4 Gy in 28 fractions) combined with concurrent systemic chemotherapy (CMT). The primary reasons for this preference are the lack of sphincter preservation and the inability to safely combine adequate doses of systemic chemotherapy with short course radiation. CMT trials cannot be directly compared with short course radiation trials because they exclude patients with cT1-2 disease. Short course radiation trials include patients with cT1-3 disease.
Bujko and colleagues performed a randomized trial of 2 preoperative approaches. A total of 316 patients with cT3 rectal cancer were randomized to short course radiation followed by surgery versus conventional preoperative CMT followed by surgery. All tumors were above the anorectal ring, TME was performed for distal tumors, and there was no radiation quality control review. There were no significant differences in local control or survival. The incidence of positive circumferential radial margins (CRM+) was lower following CMT compared with radiation alone (4% vs 13%, P = .017). Results from a similar Australian trial are pending.
Is postoperative adjuvant chemotherapy necessary?
Two randomized trials question whether postoperative chemotherapy is beneficial in patients with cT3 rectal cancer who receive preoperative therapy. The EORTC 22921 was a 4-arm randomized trial of 1011 patients who received preoperative 45 Gy with or without concurrent bolus 5-FU/leucovorin followed by surgery with or without 4 cycles of postoperative 5-FU/leucovorin. Only 37% had a TME. The FFCD 9203 was a 2-arm randomized trial of 742 patients randomized to preoperative 45 Gy with or without bolus 5-FU/leucovorin. However, all patients were scheduled to receive postoperative chemotherapy and 73% did receive it.
The EORTC trial revealed a significant decrease in the local failure rate in those patients who receive CMT compared with radiation (8% to 10% vs 17%, P <.001) but no difference in 5-year survival (65%). However, only 43% received 95% or more of the planned postoperative chemotherapy, which may explain the negative results. Furthermore, a subset analysis of the EORTC trial revealed that patients who responded to preoperative CMT had a survival benefit from postoperative chemotherapy. The FFCD trial reported a similar decrease in local failure (8% vs 17%, P <.05), a corresponding increase in pathologic complete response rate (pCR) (11% vs 4%, P <.05), but no survival benefit (68% vs 67%) with preoperative CMT.
Given that most patients did not receive adequate doses of postoperative chemotherapy in the EORTC trial and the FFCD trial tested only the effect of 6 weeks of concurrent chemotherapy with preoperative radiation, preoperative CMT followed by surgery and 4 months of postoperative adjuvant chemotherapy (FOLFOX) remains the standard practice in North America. However, there remains considerable controversy in some European countries regarding its use.
Most investigators believe the treatment is reasonable and use the same adjuvant chemotherapy for adjuvant colon and rectal cancer. For patients who receive preoperative CMT, and are selected to receive postoperative adjuvant chemotherapy, 4 months (8 cycles) of mFOLFOX6 is recommended.
CMT for node-negative rectal cancer
There may be a subset of patients with pT3N0 disease who may not require adjuvant therapy. Patients who undergo a TME, have at least 12 nodes examined, and have stage pT3N0 disease likely do not need the radiation component of CMT. The approximately 3% to 4% benefit in local control with radiation may not be worth the risks, especially in women of reproductive age. However, patients with pT3N0 tumors with either adverse pathologic features, resected without a TME, or in whom fewer than 12 nodes have been examined should still receive postoperative CMT.
Neither MRI nor any other imaging modality or clinicopathologic factor can reproducibly identify patients with LN+ disease. Tumor regression grade may help predict LN+. The development of more accurate methods to identify LN+ disease, including imaging techniques and/or molecular markers, is essential because more patients are being treated with preoperative CMT.
In the German trial, 18% of patients clinically staged as cT3N0 preoperatively and who underwent initial surgery without preoperative therapy had pT1-2N0 disease. Therefore, those patients would have been overtreated if they had received preoperative therapy. Although not ideal, preoperative therapy is still preferred to performing surgery first because even after preoperative CMT (which downstages tumors) Guillem and colleagues reported that 22% have ypN+ disease at the time of surgery. In patients who undergo surgery alone this number is as high as 40%. These patients then require postoperative CMT, which, compared with preoperative CMT, has inferior local control, higher acute and chronic toxicity, and, if a low anastomosis is performed, inferior functional results. Furthermore, the incidence of positive nodes was not dependent on the distance from the anal verge. Of the 103 patients with tumors from 0 to 5 cm from the anal verge, 23% were ypN+, whereas of the 85 patients with tumors 6 to 12 cm from the anal verge the incidence was 20%. These data suggest that up to 12 cm from the anal verge, the risk of positive nodes (and likely local recurrence) is similar.
Distance from the anal verge
There are no prospective randomized data examining the effect of the distance from the anal verge on local recurrence. The available data are subset analysis from randomized trials that were not stratified by distance. Additional variables could have contributed to the differences in local failure. For example, TME was used in the Dutch CVKO and German trials and not in the Swedish trial. All 3 trials included patients with tumors more than 12 cm from the anal verge in the upper or high category. Because the peritoneal reflection varies from 12 to 16 cm some patients with tumors above the peritoneal reflection (colon cancer) were included in the 3 trials. Most investigators now limit preoperative treatment to tumors less than 12 cm from the anal verge. Distance measurements using a flexible proctoscope are less accurate than a straight proctoscope. Flexible scopes were used in the Dutch CKVO trial. The German trial used a straight scope. In the Swedish trial proctoscopic information was not mentioned. However, eligibility was limited to tumors “below the promontory as identified by barium enema.” The Polish trial is not discussed because all tumors were within reach by digital examination.
As seen in Table 1 , by univariate analysis, high tumors in both the Dutch CKVO and Swedish trial (defined as >10.1 cm and 11 cm, respectively) had a lower incidence of local recurrence compared with mid and lower tumors. Short course radiation did not significantly decrease local recurrence. By multivariate analysis, tumor location was an independent prognostic variable in the Dutch trial. Radiation did significantly decrease local recurrence for mid tumors in both trials, whereas for lower tumors it was helpful only in the Swedish trial.
| Location | Distance from the Anal Verge (cm) | Number | Surgery 5-year Local Failure (%) | Number | Preoperative Radiation Dose/Fraction Size 5-year Local Failure (%) | P |
|---|---|---|---|---|---|---|
| Dutch CKVO | ||||||
| High | ≥10.1 | 271 | 6 | 262 | 4 | Not significant |
| Middle | 5.1–10 | 350 | 14 | 372 | 4 | <0.001 |
| Low | ≤5 | 253 | 12 | 237 | 11 | Not significant |
| Swedish Rectal Cancer Trial | ||||||
| High | ≥11 | 110 | 12 | 133 | 8 | Not significant |
| Middle | 6–10 | 198 | 26 | 185 | 9 | <0.001 |
| Low | ≤5 | 146 | 27 | 136 | 10 | 0.003 |
In contrast, there was no significant difference between mid and upper tumors in the German trial. However, data were not provided. In a recent subset analysis, patients with tumors more than 6 cm had a lower local recurrence rate (Rodel, personal communication, 2009).
Given the conflicting data combined with the report from Guillem and colleagues confirming that the incidence of positive nodes (ypN0 disease following preoperative CMT) is the same from 0 to 12 cm from the anal verge, treatment decisions based on the current definitions of low versus mid versus high should not be used.
Positive radial (circumferential) margins
The radial (circumferential) margin also has a substantial effect on the local recurrence rate. In the Dutch CKVO trial, 17% had positive circumferential margins. In a subset analysis by Nagtegaal and colleagues, patients with positive circumferential margins who underwent TME alone had local recurrence rate of 17% after a low anterior resection and 30% after an APR. Few centers perform the necessary pathologic examination to detect positive circumferential margins. High-resolution MRI can help identify patients who have positive margins as well as select those who may benefit from preoperative therapy.
A positive circumferential margin following preoperative CMT is less favorable. Compared with 460 patients with negative circumferential margins, Baik and colleagues reported that the 44 patients with positive margins had a higher local recurrence (35% vs 11%) and decreased survival rates (27% vs 73%). An analysis of more than 17,500 pathologic specimens by Nagtegaal and Quirke reported inferior survival in patients with CRM+ after neoadjuvant treatment compared with immediate surgery (hazard ratio [HR] 6.3; 95% confidence interval [CI], 3.7 to 16.7 vs HR 2.0; 95% CI, 1.4 to 2.9, respectively).
As reported with preoperative therapy, postoperative treatment has limited ability to control positive circumferential margins. In the MRC CR-07 trial, patients with positive radial margins who were selected to receive postoperative CMT had an 11% local recurrence rate. Likewise, in a subset analysis of the Dutch CKVO trial, 50 Gy postoperatively did not compensate for positive margins.
Is radical surgery necessary following preoperative CMT?
One series has questioned the value of radical surgery in patients who had a biopsy-proven complete response. However, it included patients with cT1-3 disease and has not been reproduced by other investigators. In series limited to patients with cT3 disease who received preoperative CMT, radical surgery is still necessary to fully evaluate if a pathologic response has been achieved. Neither posttreatment ultrasound nor physical examination is sufficient. The use of PET scan and diffusion MRI as noninvasive measures of response is being investigated and has reported mixed results. Although Kalff and colleagues reported FDG-PET identification of residual viable tumor in 63 patients following CMT had a high positive predictive value (0.94; 95% CI 85%–99%), other groups have reported opposite results.
Glynne-Jones and colleagues reviewed 218 phase II and 28 phase III trials of preoperative radiation or CMT and confirmed that clinical and/or radiologic response does not sufficiently correlate with pathologic response, and these investigators do not recommend a wait-and-see approach to surgery following preoperative therapy.
Experience with preoperative CMT followed by local excision is more limited. Most series select patients with cT3 disease who were either medically inoperable or refused radical surgery. Local recurrence rates range from 0% to 20% and 5-year survival ranges from 78% to 90%. Borschitz and colleagues reported local recurrence rates by pathologic stage: ypT1: 2%, ypT2; 6% to 20%. Rates were as high as 43% in ypT3 tumors that did not respond to CMT. This approach is being prospectively tested in the ACOSOG 06031 trial. In this phase II trial, patients with uT2N0 disease received preoperative capecitabine + oxaliplatin (CAPOX) and radiation therapy. If following local excision they have stage ypT0-2 with negative margins they undergo observation only. If the postoperative stage is ypT3 or if the margins are positive then patients undergo radical surgery. A similar trial in France (GRECCAR 2) is designed to accrue 300 patients with cT2-3 disease.
CMT regimens
Both cytotoxic and targeted chemotherapeutic agents have been incorporated into phase I/II combined modality programs, most commonly in the preoperative setting. Selected series are seen in Table 2 . Most of the regimens reveal higher pCR rates compared with 5-FU alone (10% in the German trial). However, for some agents, with this increased pCR rate is an associated increase in acute toxicity.
| Author/Regimen | Number | Phase | RT (Gy) | pCR (%) | LF (%) | Gr 3+ Acute Toxicity a |
|---|---|---|---|---|---|---|
| Hofheinz et al, CAPIRI | 19 | I | 50.4/1.8 | 21 | — | 8% fatigue |
| Fakih et al, CAPOX | 12 | I | 50.4/1.8 | 27 | — | — |
| Allal et al, Irinotecan | 37 | I/II | 50/1.25 twice daily | 17 | 5 (3-y) | 6% heme, infection, 24% GI, 15% skin |
| Willett et al, CAPOX + bevicizumab | 32 | I/II | 50.4/1.8 | 16 | 100 (5-y) | 22% diarrhea, 9% HTN, 6% skin, 3% dehydration, abscess, pain, neuro |
| Das et al, Capecitibine CI 5-FU (match pair analysis) | 89 89 | II | 52.5/1.8 52.5/1.8 | 21 12 | 6 (3-y) 1 (3-y) | 6% 6% |
| Hospers et al, CAPOX | 21 | II | 50.4/1.8 | 10 | — | 18% diarrhea |
| Machiels et al, CAPOX | 40 | II | 45/1.8 | 14 | 0 (14 M) | 30% diarrhea, 5% vomiting, neutropenia, fever, fatigue, pain |
| Avallone et al, FOLFOX/raltitrexed | 31 | II | 45/1.5 | 42 | 0 (29 mo) | 3% stomatitis, 22% diarrhea, 39% neutropenia |
| Ryan et al, (CALGB 89901) FOLFOX | 26 | II | 50.4/1.8 | 25 | — | 38% diarrhea, 19% fatigue |
| Rodel et al, CAPOX + cetuximab | 48 | II | 50.4/1.8 | 9 | — | 19% diarrhea |
| Krishnan et al, Capecitabine | 54 | II | 52.2/1.8 | 18 | — | 9% skin, 2% diarrhea |
| Crane et al, Capecitabine + bevacizumab | 25 | II | 50.5/1.8 | 32 | 7% 2-y | 3% wound comp require surgery, 4% rash, 4% neuropathy |
| Bertolini et al, Induction cetuximab | 40 | II | 50–50.4/1.8–2 | 8 | — | 15% |
| Navarro et al, FOLFIRI | 74 | II | 45/1.8 | 14 | — | 7% neutropenia, 14% diarrhea, 9% asthenia, 16% rectal/abdominal pain |
| Chau et al, Induction CAPOX Capecitibine | 77 | II | 50.4/1.8 | 24 | — | 7% heme, 4% GI, 3% GU, 43% skin |
| Mohiuddin et al, (RTOG 0012) FOLFIRI CI 5-FU | 54 52 | II R | 50.4–54/1.8 55.2–60/1.2 Twice daily | 28 28 | — — | 57% heme and nonheme 51% heme and nonheme |
| Fernandez-Martos et al, Induction CAPOX Postoperative CAPOX | 56 52 | II R | 50.4/1.8 | 14 13 | — — | 17% ( P = .00004) 51% |
| Valentini et al, Oxaliplatin/raltitrexed 5-FU/CDDP | 81 83 | II R | 50.4/1.8 50.4/1.8 | 36 24 | — — | 16% 7% |
| Aschele et al, (STAR) CI 5-FU FOLFOX | 295 291 | III | 50.3/1.8 50.4/1.8 | 16 15 | — — | 15 ( P <.001) 24 |
| Gerard et al, (ACCORD) Capecitibine CAPEOX | 379 368 | III | 45/1.8 50/1.8 | 14 19 | — — | 11 ( P <.001) 25 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree