Benefits
Risks
Reduced cardiovascular risk (RR approx. 0.75)
Increased risk of GI hemorrhage
(<100 mg/day 0.3 %/year vs. 1.1 % with >325 mg/day)
Reduced risk of GI cancers
Increased risk of hemorrhagic stroke
(<100 mg/day 1.1 %/year vs. 2.5 %/year with >325 mg/day)
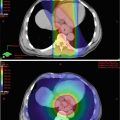
Table 5.2
AspECT trial randomization
Arm A: 20 mg esomeprazole | Arm B: 80 mg esomeprazole | No aspirin group |
Arm C: 20 mg esomeprazole + 300 mg aspirin | Arm D: 80 mg esomeprazole + 300 mg aspirin | Aspirin group |
Low-dose PPI group | High-dose PPI group |
Statins
The anti-inflammatory properties of statins confer wider benefits and have resulted in their widespread use over and above their biochemical lipid-lowering effect. This group of drugs is now being investigated as a possible candidate for cancer prevention.
A recent meta-analysis included 11 observational studies of BE patients taking statins and used adenocarcinoma as the primary outcome measure. Overall this included 317 cancers and 1999 controls and found that daily statin use had a significant negative association with incidence of adenocarcinoma (OR = 0.57; 95 % CI: 0.43–0.75) [26]. A population-based study has also reported an association between statins and a reduction in incidence of all types of esophageal cancers (i.e., combined squamous and adenocarcinoma data) (OR = 0.81; 95 % CI: 0.75–0.88) [26].
RCT data are lacking, however, and BSG guidelines advise that conclusions cannot be drawn from the current evidence base [15]. Such trials are now under way, with a long follow-up design to evaluate and quantify the potential benefits of statins in the prevention of esophageal and other gastrointestinal malignancies.
Dietary Compounds
A number of naturally occurring compounds which form part of the diet (sometimes referred to in this context as “nutraceuticals”) have been investigated for chemoprevention of gastrointestinal neoplasia [27]. In many cases prompted by epidemiological evidence from dietary studies, some such compounds are now being considered as preventive agents.
Polyphenols in green tea, in particular the catechin epigallocatechin-3-gallate (EGCG), have attracted interest for their potential anticancer properties in a wide range of tumors [28, 29]. Multiple possible mechanisms of action have been proposed for the antitumorigenic effects of EGCG, including its antioxidant potential, cell cycle arrest, induction of apoptosis, and modulation of cell signaling including COX-2 inhibition [29].
A large prospective cohort study among 69,310 Chinese women found regular consumption of tea (≥3 cups/week for 6 months) significantly reduced overall risk of digestive system cancers with mean follow-up of 11 years [30]. For stomach and esophageal cancer (all types combined), the hazard ratio associated with regular green tea consumption was 0.77 (95 % CI 0.57–1.03) [30]. An earlier case–control study, also in Shanghai, found a significant reduced risk of esophageal cancer among female regular tea drinkers, HR 0.50 (95 % CI 0.30–0.83), though tea drinking did not have a significant effect on esophageal cancer risk in males [31].
Further evidence for a protective effect of green tea extract in esophageal cancer comes from animal studies, where significant inhibitory effects have been shown in rat esophageal tumor models [32–34]. A study of human adenocarcinoma and immortalized Barrett’s cell lines showed similar inhibition of cell growth with polyphenon E, another green tea-derived catechin [35].
Flavonoids and proanthocyanidins are polyphenols found in fruit and vegetables that may contribute to the protective effect of raw fruit and vegetables in esophageal cancer [36]. In particular, soy compounds have been closely studied following the discovery that genistein, the major isoflavone in soy, is an inhibitor of epidermal growth factor receptor (EGFR) tyrosine kinase [37]. Much of the evidence for a protective effect of soy isoflavones comes from breast cancer: a number of studies have examined this association, and a meta-analysis of 14 studies concluded that soy consumption reduced risk of breast cancer in postmenopausal Asian women (RR 0.76, 95 % CI 0.65–0.86), but not among Western populations [38].
Epidemiological studies have suggested that high dietary flavonoids are associated with a reduced risk of a diverse range of solid tumors [39, 40]. A case–control study in Italy found that higher dietary intake of flavonoid compounds reduced the risk of esophageal squamous cell carcinoma (OR 0.38 for highest vs. lowest quintile (95 % CI 0.23–0.66)) [41]. However a subsequent case–control study in the United States found that higher rates of dietary anthocyanidin consumption reduced the risk of esophageal adenocarcinoma in white males and isoflavonoid consumption was associated with reduced esophageal squamous cell carcinoma in the same group, but neither association remained significant after adjusting for dietary fiber intake [36].
Supplementation with a variety of vitamins and minerals has been attempted in randomized trials: a large prospective cohort study [42] and an earlier meta-analysis [43] have shown no beneficial effect on incidence of upper gastrointestinal malignancy for multivitamins, but the cohort study found an association between iron supplementation and lower incidence of esophageal adenocarcinoma [42].
Curcumin has been investigated as a chemopreventive agent in a variety of malignancies [44], with several non-randomized trials in patients with colorectal cancer [45–47], and there is some limited evidence for a role in esophageal cancer from animal studies and cultured cell lines [48, 49].
Preclinical data for each of these compounds suggests that potential, but as yet trial, data is lacking to support the use of any of these compounds or to advocate widespread dietary change.
Conclusions
PPIs are widely recommended for patients with BE, though conclusive evidence for a chemopreventive effect against progression to adenocarcinoma is awaited. The benefits of aspirin in cancer prevention have been demonstrated in large cohorts of patients taking it for vascular prevention – its specific effects for esophageal cancer and prevention of progression of BE have not yet been shown in randomized controlled trials. The AspECT trial aims to address these issues and provide firm evidence to underpin chemoprevention in patients with BE.
Trial data on statins is awaited, and if effective in cancer prevention, this area may be a further indication for this group.
It is hoped that improved understanding of the molecular mechanisms underlying progression in BE will reveal novel therapeutic targets and help to identify whom will most benefit from chemoprevention. The shared molecular origins of many cancers provide further hope that developments in cancer prevention of one malignancy may lead to successful interventions in other tumor types.
References
1.
Bazuro GE, Torino F, Gasparini G, et al. Chemoprevention in gastrointestinal adenocarcinoma: for few but not for all? Minerva Gastroenterol Dietol. 2008;54:429–44. http://www.ncbi.nlm.nih.gov/pubmed/19047983. Accessed 15 Aug 2014.PubMed
2.
Fitzgerald RC, Omary MB, Triadafilopoulos G. Dynamic effects of acid on Barrett’s esophagus. An ex vivo proliferation and differentiation model. J Clin Invest. 1996;98:2120–8. doi:10.1172/JCI119018.PubMedCentralCrossRefPubMed
3.
Clemons NJ, McColl KEL, Fitzgerald RC. Nitric oxide and acid induce double-strand DNA breaks in Barrett’s esophagus carcinogenesis via distinct mechanisms. Gastroenterology. 2007;133:1198–209. doi:10.1053/j.gastro.2007.06.061.CrossRefPubMed
4.
Ouatu-Lascar R, Fitzgerald RC, Triadafilopoulos G. Differentiation and proliferation in Barrett’s esophagus and the effects of acid suppression. Gastroenterology. 1999;117:327–35. http://www.ncbi.nlm.nih.gov/pubmed/10419913. Accessed 26 Aug 2014.CrossRefPubMed
5.
Shirvani VN, Ouatu-Lascar R, Kaur BS, et al. Cyclooxygenase 2 expression in Barrett’s esophagus and adenocarcinoma: ex vivo induction by bile salts and acid exposure. Gastroenterology. 2000;118:487–96. http://www.ncbi.nlm.nih.gov/pubmed/10702199. Accessed 26 Aug 2014.CrossRefPubMed
6.
Abdalla SI, Lao-Sirieix P, Novelli MR, et al. Gastrin-induced cyclooxygenase-2 expression in Barrett’s carcinogenesis. Clin Cancer Res. 2004;10:4784–92. doi:10.1158/1078-0432.CCR-04-0015.CrossRefPubMed
7.
Neumann CS, Iqbal TH, Cooper BT. Long term continuous omeprazole treatment of patients with Barrett’s oesophagus. Aliment Pharmacol Ther. 1995;9:451–4. http://www.ncbi.nlm.nih.gov/pubmed/8527623. Accessed 26 Aug 2014.CrossRefPubMed
8.
Cooper BT, Neumann CS, Cox MA, et al. Continuous treatment with omeprazole 20 mg daily for up to 6 years in Barrett’s oesophagus. Aliment Pharmacol Ther. 1998;12:893–7. http://www.ncbi.nlm.nih.gov/pubmed/9768533. Accessed 26 Aug 2014.CrossRefPubMed
9.
Gore S, Healey CJ, Sutton R, et al. Regression of columnar lined (Barrett’s) oesophagus with continuous omeprazole therapy. Aliment Pharmacol Ther. 1993;7:623–8. http://www.ncbi.nlm.nih.gov/pubmed/8161668. Accessed 26 Aug 2014.CrossRefPubMed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree