Site
Total
%
Male
Female
Male/female
Pineal
73
45
68
5
14
Neurohypophyseal
52
32
26
26
1
Pineal + neurohypophyseal
17
10
15
2
7.5
Basal ganglia, thalamus
21
13
20
1
20
Total
163
–
129
34
3.8
14.3 Presenting Symptoms
Presenting symptoms depend on tumor location. In patients with pineal germinomas, Parinaud sign (upward gaze palsy and pupillary light-near dissociation) is seen when the tumor becomes large. Accordingly, patients may complain visual disturbance including diplopia. In patients with a large tumor, hydrocephalus and associated symptoms could develop. In neurohypophysial germinomas, diabetes insipidus is the most common symptom. With tumor enlargement, deficits of hormones from the anterior lobe of the pituitary gland, visual field defects, and visual disturbances could develop. In germinomas of the basal ganglia, hemiparesis, change in mental and neurocognitive status, and/or loss of higher brain functions can be presenting symptoms.
14.4 Radiographic Findings
Germinoma shows homogenous density on CT and homogenous signal intensity on T1-weighted MR images (Fujimaki et al. 1994). It is slightly hyperdense and hyperintense on CT and T1-weighted MRI, respectively. Typically, it shows homogenous and striking contrast enhancement, but slightly inhomogenous contrast enhancement does not exclude the possibility of germinoma. Inhomogeneity of the density, signal intensity, and contrast enhancement indicate the possibility of a non-germinomatous germ-cell tumor; however, germinoma often contains cysts, so the differential diagnosis is often not easy. Findings of subependymal spread and intraventricular dissemination are sometimes observed.
14.5 Workup
When germinoma is suspected on MRI, tumor markers, i.e., β-human chorionic gonadotropin (HCG), α-fetoprotein (AFP), and carcinoembryonic antigen (CEA), in the serum and/or cerebrospinal fluid (CSF) should be checked. A recent development in immunohistochemistry enables the detection of very low levels of HCG, especially its β-subunit, using an ultrasensitive kit. In one study, use of this ultrasensitive assay showed that elevation of β-HCG levels in the serum or CSF was seen in most CNS germinoma patients (Katakami et al. 2003). Elevation of β-HCG over 1000 mIU/mL or 200 ng/mL would indicate the presence of pure or mixed non-germinomatous germ-cell tumors, especially choriocarcinoma, but low levels of elevation below 10 mIU/mL or 2 ng/mL would suggest that the tumor is pure germinoma. It should be noted that elevation of β-HCG levels may be observed in craniopharyngioma (Suzuki et al. 1985). On the other hand, elevation of AFP or CEA levels indicates the presence of non-germinomatous germ-cell tumors or their component. Placental alkaline phosphatase (PLAP) is also known as a marker for germinoma (Ono et al. 1991). Although the usefulness of PLAP does not seem to be well established, the true- and false-positivity rates are reported to be about 50% and 1.6%, respectively, in testicular seminoma (Koshida et al. 1996).
Investigation of CSF dissemination is important, and CSF cytology should be performed. Germinoma frequently shows the “two-cell pattern” that was considered to be almost pathognomonic (Sano 1976), but later, it was realized that other diseases can also show similar cytological patterns. So, CNS germinoma cannot be diagnosed by the CSF cytological findings alone although it is helpful in diagnosing CSF dissemination (Shibamoto et al. 1994a, b). Whole spinal MRI should also be performed.
14.6 Acute Management
When hydrocephalus is observed, CSF drainage needs to be considered. However, one may avoid placement of a shunt tube because tumor shrinks quickly in response to treatment and hydrocephalus can soon be ameliorated. Mass effect is unusual, so debulking operation and administration of steroid are usually unnecessary.
14.7 Treatment
Until recently, the standard treatment for CNS germinoma has been radiation therapy alone. Germinoma can be cured with a total dose of 40–50 Gy. The vast majority of patients treated with radiation therapy live a normal life, but long-term adverse effects in adolescents were feared, particularly hormonal insufficiency and decline in neurocognitive function (Duffner et al. 1985; Roman and Sperduto 1995). In the late 1980s, systemic platinum-based chemotherapy was employed, and its efficacy was recognized. However, treatment with chemotherapy alone was found to be associated with a high recurrence rate of 50–60% (Farng et al. 1999; Kumabe et al. 2002; Balmaceda et al. 1996). Although germinoma recurring after primary chemotherapy can be salvaged with radiation therapy (Shibamoto et al. 1999), the high recurrence rate was considered unacceptable and the chemotherapy alone trials were regarded as a failure. Thereafter, systemic chemotherapy with reduced-dose radiation was investigated and reasonably high cure rates comparable to those obtained by standard radiotherapy have been reported. Thus, systemic chemotherapy with reduced-dose radiation appears to be gaining popularity although treatment with radiation alone remains an option for patients.
14.7.1 Surgery
Surgical resection is usually unnecessary for this tumor.. The role of surgery is limited to establishing histological diagnosis. With improvements in modern diagnostic imaging modalities and tumor marker measurements, the authors think that histological diagnosis may not be mandatory in every patient. This is rather controversial as the standard approach in North America is to have histological confirmation of the tumor. Even with the advances in neurosurgery, the authors argue that the probability of complications from a biopsy exists, and any complication associated with brain surgery becomes a serious problem for the patient. From the clinical and radiological findings, it is often not difficult to predict a diagnosis of germinoma even before any treatment. In addition, pure germinoma is known to quickly respond to radiation and chemotherapy. The lesions less than 3 cm in diameter usually disappear after 20 Gy of radiation therapy (“radiodiagnosis”). Marked shrinkage is also observed following systemic chemotherapy. With the typical clinical and radiological findings, mild elevation of β-HCG levels and quick response to treatment, the diagnosis of germinomas is usually confirmed. Therefore, the authors believe that avoiding a biopsy is an option in cases with typical clinical and radiological findings. Of course, there exist germinomas that do not possess above-mentioned characteristics, and biopsy should be considered for such patients. Some pure germinomas do not respond so quickly to treatment, and one of the reasons for this is considered to be the presence of granulomatous components (Utsuki et al. 2006).
14.7.2 Radiotherapy
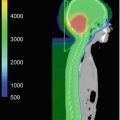
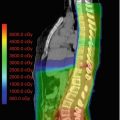
When treating germinoma with radiation alone, the treatment volume is a controversial issue. Since germinoma can develop CSF dissemination in up to 10% of patients, irradiation of the entire cerebrospinal axis was historically the recommended treatment. (Shibamoto et al. 1988, a) reported treatment results according to the irradiated volume. Depending on the era of treatment, germinoma patients were irradiated to the primary tumor site plus a margin or to the cerebrospinal axis regardless of the clinical and radiological findings. There was no significant difference in overall survival between patients receiving craniospinal irradiation and those receiving focal radiation; the 10-year survival rate was 95% for 38 patients receiving craniospinal irradiation and 88% for 33 patients receiving focal radiation therapy. In a comprehensive review of the existing literature, (Rogers et al. 2005) found that the recurrence rate was 7.6% after whole-brain or whole ventricular radiotherapy plus boost compared with 3.8% after craniospinal radiotherapy. Since the incidence of CSF dissemination beyond the ventricular system is below 10%, the routine use of craniospinal irradiation appears to be overtreatment for most patients, and hence treatment with whole ventricular irradiation followed by a boost has gained popularity. It is now recommended to treat the whole cerebrospinal axis only when CSF cytology is positive or CSF dissemination is present.
Previously, the standard dose for pure germinoma was 50 Gy in 1.8–2.0 Gy daily fractions. (Shibamoto et al. 1994a, b, 2001) conducted a prospective study to investigate dose reduction for germinoma. Using a daily dose of 1.8 Gy (focal radiation) or 1.6 Gy (craniospinal radiation), the total dose was 36 Gy after macroscopic total tumor removal, 40 Gy for tumors less than 2.5 cm, 45 Gy for tumors between 2.5 and 4 cm, and 50 Gy for larger tumors. An individualized approach was employed to determine the treatment volume. After a median follow-up of 120 months, the 10-year relapse-free survival rate for 38 patients treated with this policy was 95%; this cure rate was considered to be equivalent to that obtained using a policy of uniformly giving 50 Gy. Therefore, the dose of 40–45 Gy appeared to be sufficient to cure CNS germinoma with a diameter 4 cm or less. The German Society for Pediatric Oncology and Hematology also conducted a prospective study to reduce total radiation doses, and they found no local recurrence after a dose of 45 Gy (Bamberg et al. 1999).
The optimal dose for cerebrospinal axis prophylaxis has not yet been clarified. Considering the high radiosensitivity of germinoma, (Shibamoto et al. 1988, 1994a, 2001) used 20–24 Gy in 13–15 fractions, and obtained a favorable outcome. In the dose-reduction study stated above (Shibamoto et al. 2001), the authors used craniospinal doses around 20 Gy for patients with negative or equivocal CSF-cytology findings and 24 Gy for patients with positive CSF cytology or CSF dissemination; one patient in the latter group developed CSF dissemination. Therefore, doses of 20 and 24 Gy were recommended for CSF dissemination-negative and positive cases, respectively. The German Society for Pediatric Oncology and Hematology also attempted at reducing the craniospinal radiation dose from 36 to 30 Gy and found no difference in the outcome of patients in both groups (Bamberg et al. 1999).
14.7.3 Chemotherapy and Reduced-Dose Radiation
Systemic chemotherapy in combination with a reduced dose of radiation has been tested by several groups (Allen et al. 1994; Bouffet et al. 1999; Matsutani et al. 2001). The dose has been reduced to 24–40 Gy, and excellent results have been reported as compared with the results obtained by chemotherapy alone. (Matsutani et al. 2001; Matsutani 2009) carried out a multi-institutional study in which three courses of carboplatin (450 mg/m3) and etoposide (150 mg/m3 × 3 days) were given before 24 Gy with a focal radiation field or an extended local field encompassing the tumor site, the third and lateral ventricles, and the sellar and pineal regions. The 5-year overall survival rate in 123 patients was 98%, and the disease-free survival was 88% (Matsutani 2009). The recurrence rate was 6% in patients treated by an extended local field, whereas it was 28% in patients treated with a limited local field with a margin of less than 2 cm. Thus, it was suggested that the radiation treatment volume should involve the whole ventricular system.
The French Society for Pediatric Oncology (SFOP) conducted a study combining chemotherapy (alternating courses of etoposide/carboplatin and etoposide/ifosfamide up to four courses whenever possible) with 40-Gy focal irradiation (CNS GCT-96) (Bamberg et al. 1999; Alapetite et al. 2005). They treated 60 patients and the 8-year overall and event-free survival rates were 98% and 83%, respectively. The SFOP group also found an excess of periventricular relapses when the focal radiation field was used in the combined treatment of germinoma, and they recommended the use of ventricular field radiation (Alapetite et al. 2010).
The International Society of Paediatric Oncology (SIOP) conducted a prospective non-randomized comparison study of craniospinal irradiation (24 Gy) plus focal tumor boost (16 Gy) vs. the SFOP CNS GCT-96 chemotherapy regimen followed by focal radiation therapy to the tumor (40 Gy) (Calaminus et al. 2013). There were no differences in 5-year overall and event-free survival between patients treated with radiotherapy alone (n = 125) and those treated with combined therapy (n = 65), but there was a difference in progression-free survival in favor of the radiotherapy alone approach (97% vs. 88%, P = 0.04). Again, patterns of relapse suggested inclusion of the entire ventricles in the radiation field. The use of lower dose irradiation (24–30 Gy) was not investigated in the SFOP and SIOP studies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree