Figure 7.1
Positioning of the patient
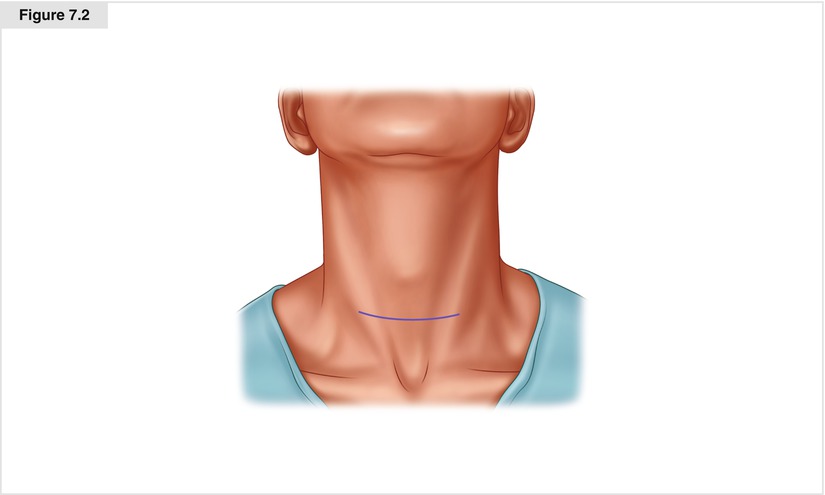
Figure 7.2
Neck incision. The length of the incision depends on whether a lateral neck dissection is also planned. If only a central neck dissection is planned, it can be done through a curvilinear low collar incision 5–10 cm in length, depending on the size and age of the patient, the extent of disease, and whether there is mediastinal extension. If possible, the incision should be place in a preexisting skin crease to achieve excellent cosmetic results
7.3.2 Initial Dissection
Subplatysmal flaps are created in the standard fashion, and a self-retaining retractor is placed (Fig. 7.3). The strap muscles are then divided in the midline (Fig. 7.4); on the side of the thyroid tumor, the sternohyoid muscle is separated from the sternothyroid muscle. The sternothyroid muscle is left attached to the underlying thyroid, and the superior and inferior attachments of this muscle are divided (at the thyroid cartilage and the sternum; Fig. 7.5).
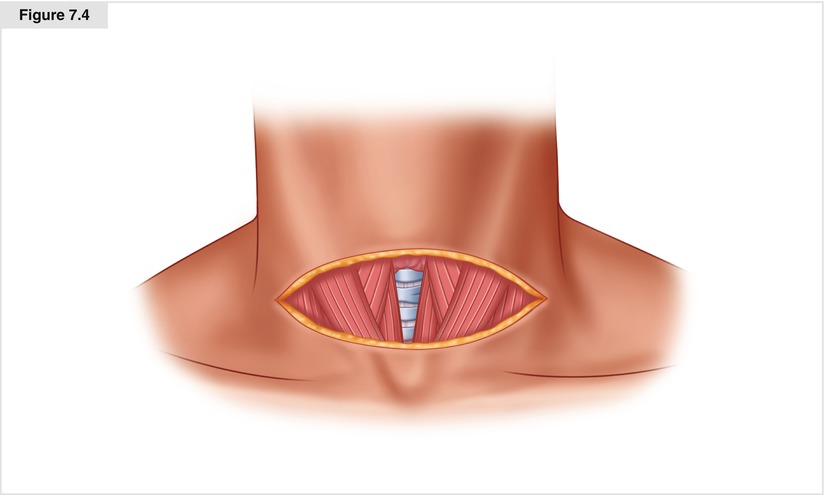
Figure 7.3
Subplatysmal flaps have been made, exposing the anterior jugular veins and the strap and sternocleidomastoid muscles. Facelift retractors are used to elevate the flaps
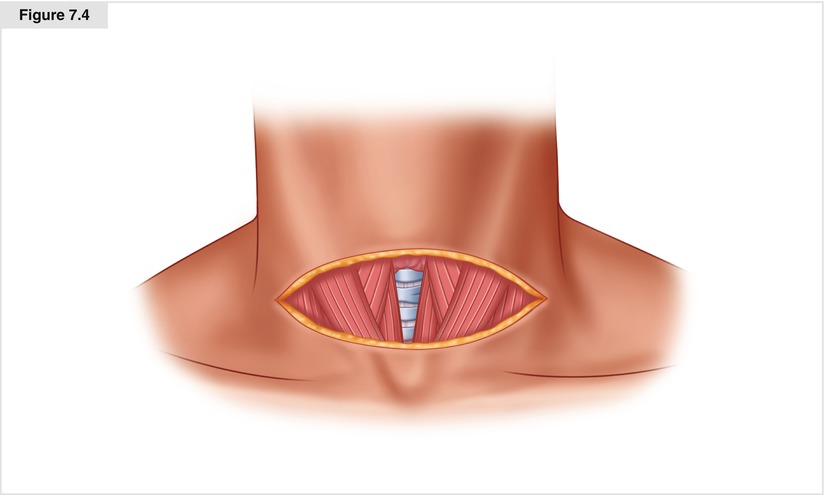
Figure 7.4
Division of the plane between the sternohyoid muscles
Figure 7.5
Resection of the sternohyoid muscle en bloc with the thyroid on the side of the tumor and location of central nodes
7.3.3 Thyroidectomy and Tumor Specimen Mobilization
Superior pole vessels are divided after mobilization medial to lateral to avoid injury to the superior laryngeal nerve, which may be visualized during this process. Once the superior pole is taken down, the thyroid is rolled medially and anteriorly. At this point, the procedure departs from what is done in a standard thyroidectomy. The objective is to sweep up the thyroid lobe with surrounding soft tissue and nodal tissue, leaving only the recurrent nerve behind. Attempts may be made to preserve the blood supply to the upper parathyroid, but I usually remove both ipsilateral parathyroids with the specimen, then dissect them out of the specimen if possible, and transplant them. Because I am not attempting to preserve the parathyroid blood supply on the side of the tumor, I divide the tissue on the anterior surface of the carotid artery and sweep everything medially (Fig. 7.6). This requires less dissection, with fewer vessels to control.
Dissection is carried out on the anterior surface of the carotid artery. If one stays directly on the anterior surface of the carotid, the dissection is quite safe, because the only structures encountered are the middle thyroid veins coming off the internal jugular vein; these veins should be divided. Inferiorly, as the carotid becomes the innominate, the surgeon encounters the thymic horns and associated veins overlying the trachea, which must be divided and swept into the specimen (Fig. 7.7). On the right, the dissection is done to the level of the innominate (brachiocephalic) artery (Fig. 7.8). On the left, the dissection is done to the level of the clavicle and left innominate (brachiocephalic) vein takeoff (Fig. 7.9) [13]. Once the central compartment contents are thus mobilized, including the thyroid, parathyroids, central neck nodes, fat, and thymus, dissection is carried out superior to inferior. For a right-handed surgeon, this dissection is generally done most easily with the surgeon on the left side, using the right hand to perform dissection from above, crossing toward the midline along the innominate artery. The thyroid is mobilized from the top down, leaving the sternothyroid muscle attached. In the process, the recurrent laryngeal nerve is identified and preserved, and the upper and lower parathyroids are identified. I generally leave the parathyroids with the specimen, remove them after removal of the specimen, place them in cold saline, and mince and transplant them as described in Chapter 4. Soft tissue and vascular attachments to the thyroid are divided, including middle veins and inferior thyroid artery and veins. The nodal packet is swept up off of the recurrent laryngeal nerve and the esophagus to the trachea. It is dissected off of the trachea, leaving only bare trachea, esophagus, and recurrent nerve centrally. Inferiorly, the specimen is swept off of the recurrent laryngeal nerve to the trachea, and the thymic horns are divided with the nodal packet at the level of the innominate artery. It is also essential to mobilize and remove the nodes that reside in the hollow behind the right recurrent laryngeal nerve.
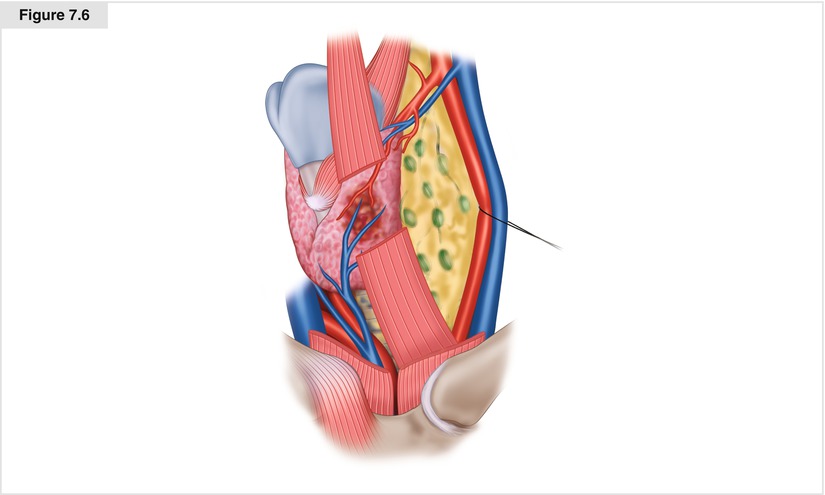
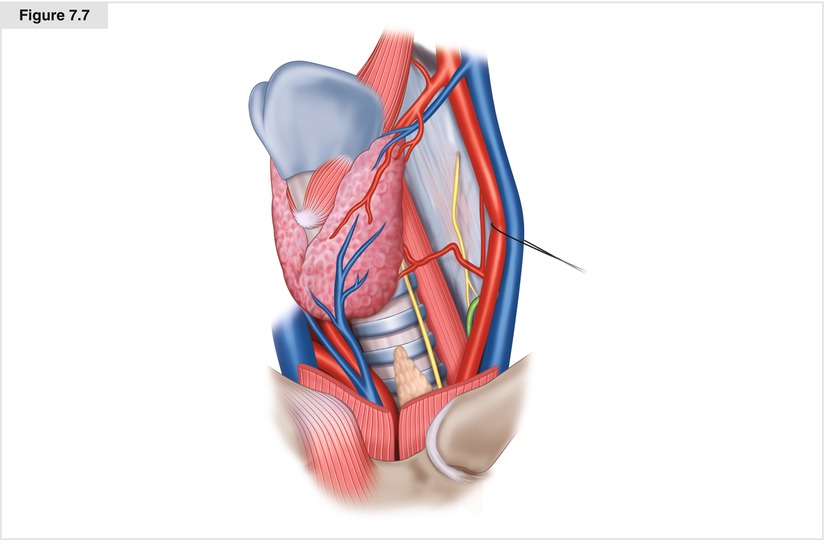
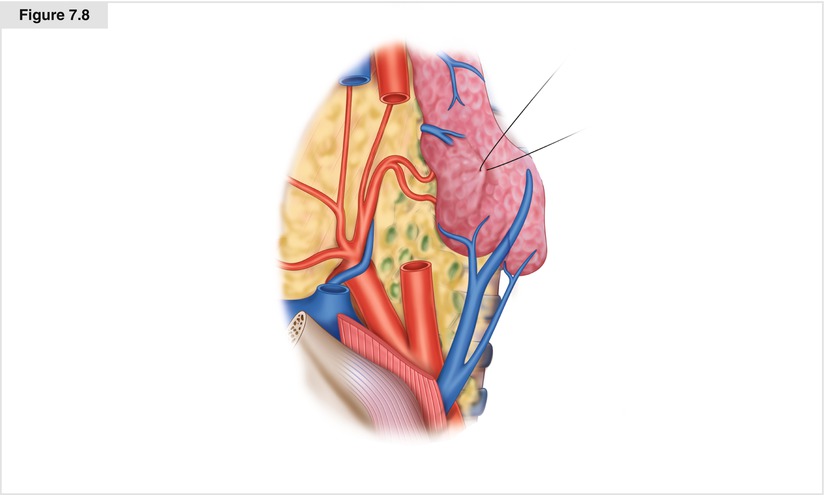
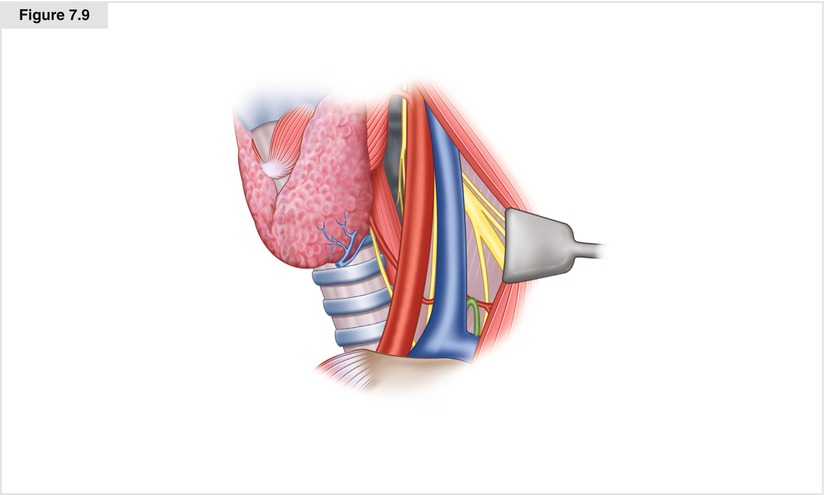
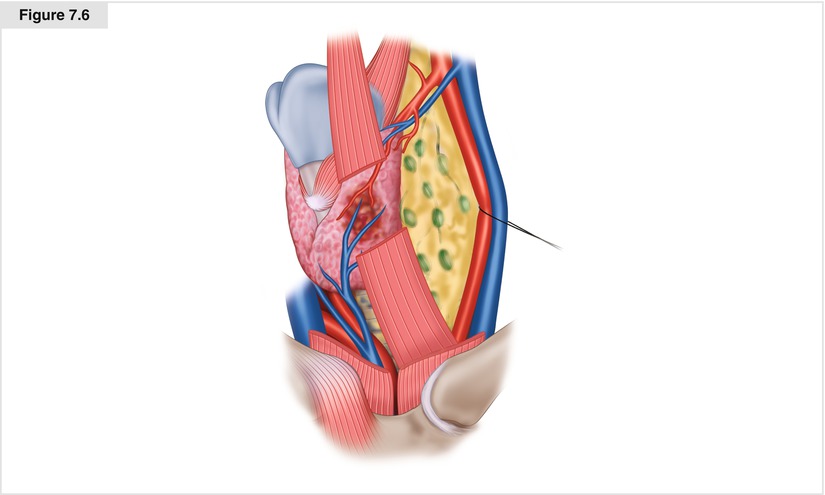
Figure 7.6
Left central node dissection (level VI). The surgeon dissects along the left carotid and frees up the fatty tissue and nodes laterally
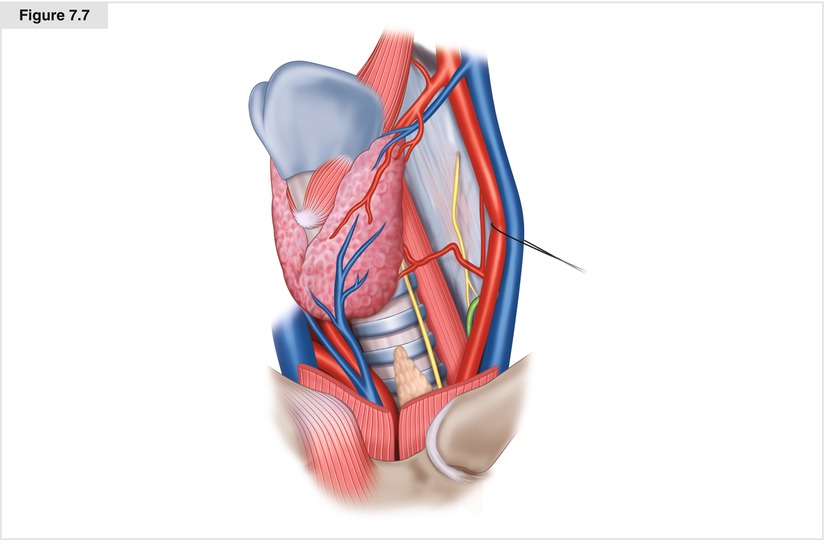
Figure 7.7
Left central node dissection (level VI). The nodes and fibrofatty tissue are dissected from the level of the hyoid bone downward along the tracheoesophageal groove to the level of the innominate vein
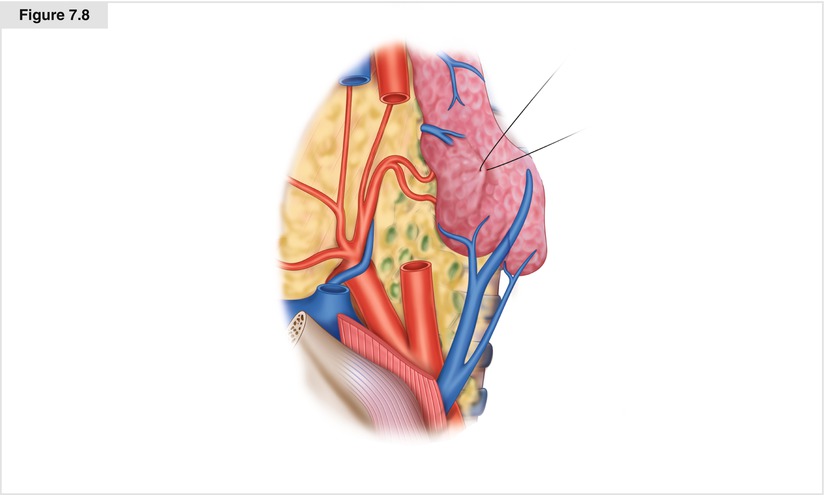
Figure 7.8
Right central neck dissection (level VI). The surgeon dissects along the anterior surface of the right carotid (shown partially removed for clarity), sweeping the right central nodal packet medially to be removed en bloc with the thyroid. The recurrent laryngeal nerve and vagus nerves are carefully protected
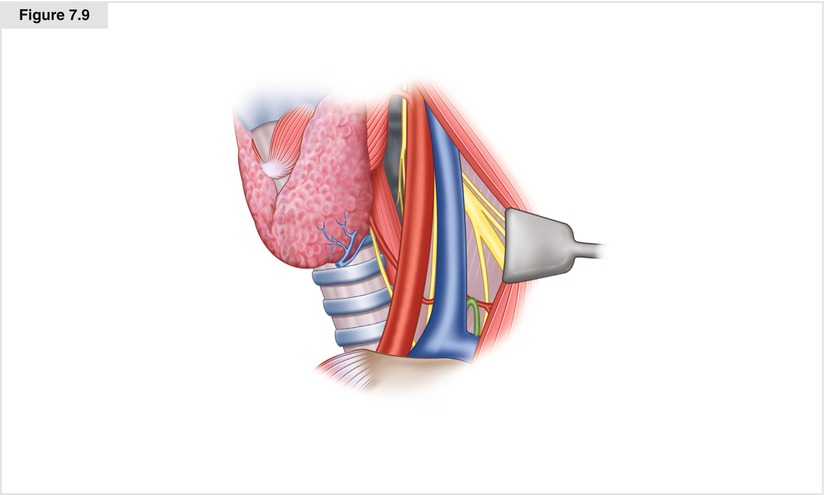
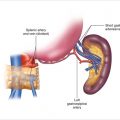
Figure 7.9
Location of the thoracic duct on the left, posterior to the carotid artery and internal jugular vein. This structure must be preserved or ligated, if injured
7.3.4 Contralateral Thyroidectomy and Node Dissection
Once the tumor side is completely mobilized, attention is turned to the contralateral side. If this side has no tumor involvement, both the sternothyroid and sternohyoid strap muscles may be mobilized off of the thyroid lobe and reflected laterally. The undersurface of the inner strap muscle is carefully cleaned off so that all fat, nodal tissue, and thymus is incorporated in the specimen. Again the thyroid superior pole is mobilized, the carotid artery is dissected on its anterior surface inferiorly, and the central compartment containing thyroid, parathyroids, nodes, and thymus is exposed (Fig. 7.8). If the surgeon prefers to preserve the parathyroids on this side, then a standard parathyroid-preserving thyroid lobectomy should be carried out, leaving the upper parathyroid on an intact vascular pedicle and the lower parathyroid on an intact pedicle in the thyrothymic ligament. Tissue medial and anterior to the thyrothymic ligament may be swept medially with the thyroid to join the contralateral dissection. The inferior extent of this packet is transected with cautery or a hemostatic device such as the harmonic scalpel, with care to ligate large veins. The entire packet including the thyroid and central neck contents is then oriented with sutures and submitted to pathology, after carefully removing any parathyroids from the tumor-bearing side of the specimen for autotransplantation.
If disease extends inferiorly into the mediastinum, it may be removed through a full or mini-sternotomy (Fig. 7.10). In the mini-sternotomy procedure, the midline sternotomy is carried down to the second or third intercostal space. Care is taken to avoid the internal mammary vessels. Dissection around the innominate vein must be done carefully. Nodal metastases are often present along the sides of the trachea as it descends deep to the innominate vein.
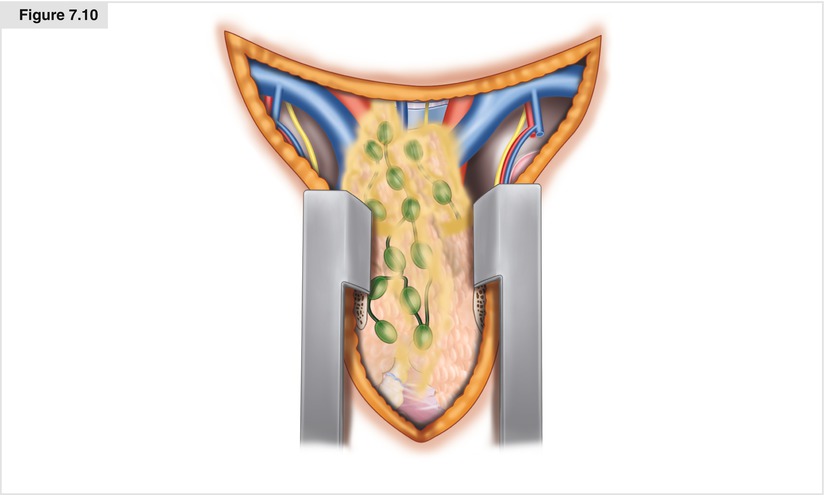
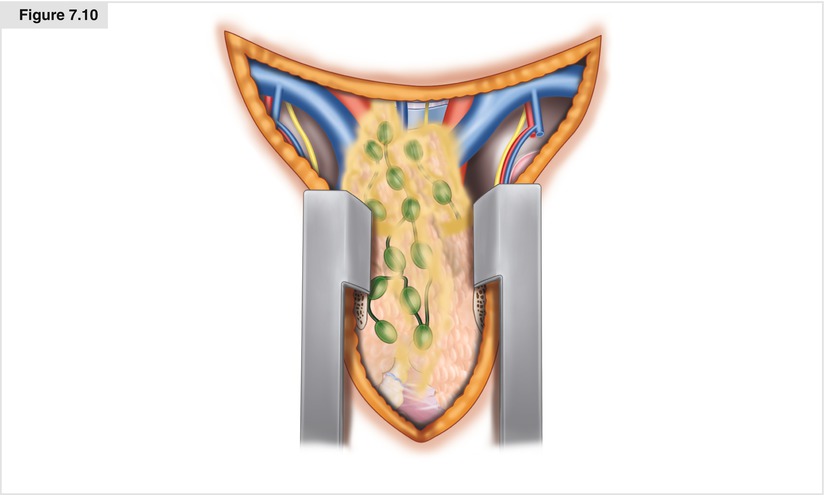
Figure 7.10
Upper mediastinal dissection (level VII) through a mini-sternotomy
7.3.5 Parathyroid Autotransplantation
The ability to identify and autotransplant parathyroid glands is critically important to any surgeon who treats thyroid cancer [5, 13, 14]. Hypoparathyroidism is a preventable complication, and its incidence should be extremely low. Parathyroids that are removed during central neck dissection should be placed in cold saline, and minced into fragments of 1 × 1 mm. These fragments are then autotransplanted into individual muscle pockets (two or three per pocket) in the sternocleidomastoid muscle (for sporadic MTC and MEN 2B), or into the muscle of the of the nondominant forearm (for selected MEN 2 cases with a risk of subsequent development of hyperparathyroidism). All removed parathyroid tissue should be transplanted. Each pocket is closed with a suture. We use absorbable suture material in sporadic cases, and permanent sutures (4-0 Prolene or silk) in MEN 2A cases, in which there is a risk that the tissue may become hyperplastic and need to be located and removed in the future.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree