Case 90
Presentation: Case 90A
The patient is a 76-year old man who is referred by a medical oncologist for possible splenectomy. He presents with vague abdominal discomfort and thrombocytopenia. The patient denies weight loss, fever, or night sweats. Past medical history is significant for hypertension, coronary artery disease, and gastroesophageal reflux. Physical examination reveals no lymphadenopathy. The spleen is enlarged and easily palpated. It is nontender. The patient has had a complete blood cell (CBC) count, bone marrow evaluation, a computed tomography (CT) scan, and magnetic resonance imaging (MRI) of the abdomen.
CBC revealed hemoglobin of 12.7, white count of 7.3, and platelets of 65,000.
Peripheral smear is significant for normochromic normocytic red cells and absence of schistocytes, spherocytes, or poikilocytes. There is no evidence of lymphocytosis or atypical lymphocytes, monocytosis, or overt dysplastic changes. Absolute lymphocyte count is 2,000; moderate thrombocytopenia with normal size platelets is noted without platelet aggregates. Bone marrow biopsy was noncontributory to the diagnosis.
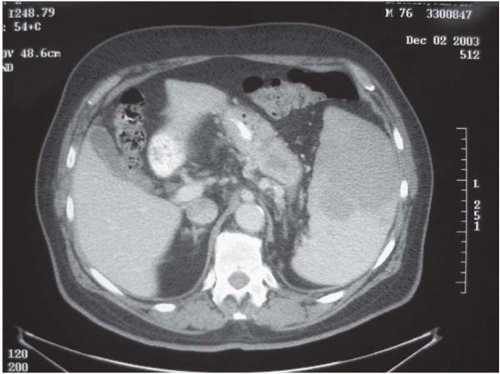
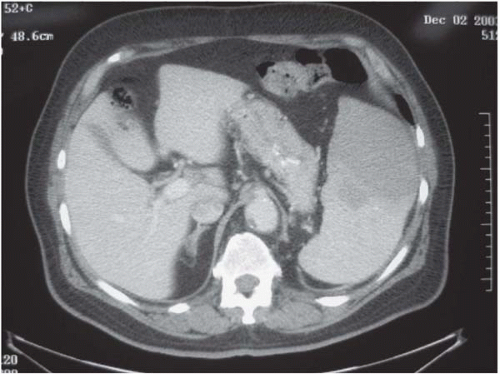
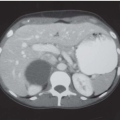
▪ CT Scan
CT Scan Report
The CT scan shows an enlarged and heterogeneous spleen. No evidence of lymphadenopathy is seen within the chest, abdomen, or pelvis. Minimal bilateral pleural effusions are shown.
Differential Diagnosis
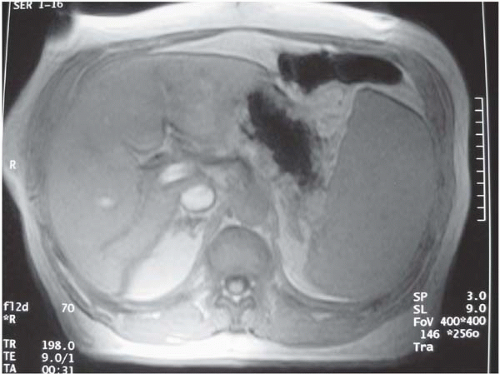
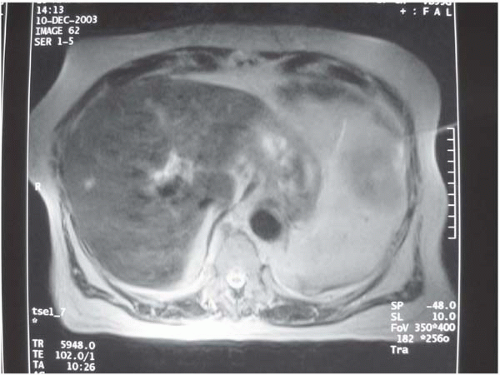
The differential diagnosis for splenomegaly, within the context of the CT and MRI findings, includes hematologic malignancy, specifically lymphoma, a splenic infiltrative or inflammatory process, and primary or metastatic splenic tumor.
Discussion
The possible etiologies of splenomegaly are extensive and can include infectious causes (viral, bacterial, parasitic), and congestive (heart failure, cirrhosis, portal or splenic venous thrombosis), malignant (lymphomas, leukemias, polycythemia vera, multiple myeloma, agnogenic myeloid metaplasia, primary and metastatic tumors), inflammatory (sarcoid, systemic lupus erythematosus, Felty syndrome), infiltrative (amyloid, Gaucher disease, Niemann-Pick disease, glycogen storage disease), and hypersplenic states (hemolytic anemias, sickle cell diseases)
Because the spleen normally participates in the filtering of senescent red blood cells (RBCs), bacteria, and debris, as well as sequestration of the normal circulating pool of platelets (up to one third), any increase in function (hypersplenism) may be manifested by varying degrees of anemia, thrombocytopenia, or pancytopenia.
This patient presents with clinical, laboratory, and imaging data that suggest a disease process attributed to the spleen, with secondary thrombocytopenia as a result of splenomegaly. The heterogeneous attenuation suggests differential splenic perfusion, which could be due to ischemia, an infarct, or a space-occupying lesion in the spleen. Lack of systemic complaints makes an infectious etiology less likely. There is no clinical evidence of cirrhosis or congestive heart failure. A hematologic malignancy must be suspected.
Recommendation
Indications for splenectomy can be characterized as diagnostic, therapeutic, or both. Therapeutic splenectomy is performed for refractory cytopenias or to relieve bulk symptoms from the enlarged spleen. The latter include abdominal pain and early satiety. The primary indication for splenectomy in this patient is diagnostic, with a suspicion of hematologic
malignancy. Secondary benefits are likely to include relief of the abdominal discomfort and resolution of the thrombocytopenia. The patient was advised to undergo splenectomy via a left subcostal incision. Procedure-specific risks were discussed, including postoperative hemorrhage, pancreatic or gastric injury, subphrenic abscess, and wound infection. Also discussed was the increased susceptibility to certain bacterial infections in the asplenic state and the use of prophylactic vaccinations.
malignancy. Secondary benefits are likely to include relief of the abdominal discomfort and resolution of the thrombocytopenia. The patient was advised to undergo splenectomy via a left subcostal incision. Procedure-specific risks were discussed, including postoperative hemorrhage, pancreatic or gastric injury, subphrenic abscess, and wound infection. Also discussed was the increased susceptibility to certain bacterial infections in the asplenic state and the use of prophylactic vaccinations.
▪ Surgical Approach
An open approach to splenectomy was undertaken due to splenic size and the potential malignant process. A left subcostal incision was created and abdominal exploration revealed bulky splenomegaly with enlarged pathologic hilar lymph nodes. A mass was palpable within the spleen and corresponded to the abnormality noted on MRI. The lesser sac was entered below the gastroepiploic arcade to expose the pancreatic body. The splenic artery was identified at the superior border of the pancreas, encircled, and ligated without division. The gastrosplenic ligament was divided up to the short gastric vessels. The spleen and pancreas were then fully mobilized to the midline. The short gastric vessels were divided. The splenic hilar vessels were then clamped and divided, with care to avoid injury to the tail of the pancreas. After specimen removal, the operative field was carefully inspected for hemostasis.
Case Continued
The patient tolerated the procedure well, was transferred to the floor postoperatively, and discharged in stable condition on postoperative day 4. Outpatient follow-up was scheduled with the hematology/oncology service. The pathology report returned as non-Hodgkin B-cell lymphoma, follicular small cleaved cell type (grade 1) involving spleen and splenic hilar lymph nodes.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree