Case 87
Presentation
A 63-year-old man presents with a serum prostate-specific antigen (PSA) level of 5.2 ng/mL (upper limit of normal 4.0 ng/mL). Prior PSA 1 year previously was 2.1 ng/mL. A repeat PSA with a free and total fraction is performed; this demonstrates a PSA of 5.3 ng/mL with a free-to-total fraction of 9% (more than 15% suggests benign disease). The patient otherwise is in good health. He has no smoking history, and no family history of prostate malignancy. No abnormal findings were noted on physical examination. The prostate is symmetrical, not enlarged, and free of nodules or induration.
Differential Diagnosis
The main concern in a patient with an elevation of PSA relates to the possible presence of adenocarcinoma of the prostate. Elevation in PSA can be secondary to benign prostatic hyperplasia or prostatitis. Other factors such as sexual activity, exercise, and digital rectal examination typically do not have a significant impact on PSA levels.
Prostate biopsy is the only means of establishing the diagnosis of adenocarcinoma of the prostate. A normal ultrasound does not exclude the presence of carcinoma, and the study should only be used to assist in biopsy, not to determine if a biopsy should be performed. This decision is based on the presence of an elevated PSA and/or the presence of a prostate nodule. Of 12 cores obtained (6 on each side), three were positive on the right for Gleason 6 (3+3) adenocarcinoma of the prostate.
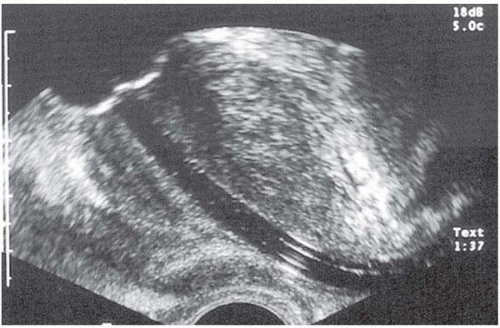
▪ Sagittal Ultrasonogram
Sagittal Ultrasonography Report
Ultrasonogram is used to assist in biopsy.
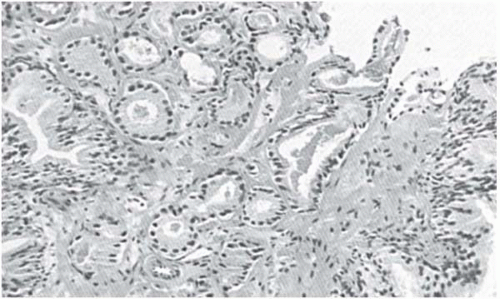
▪ Histopathologic Slide
Histopathology Report
Histology demonstrates Gleason 6 (3+3) adenocarcinoma of the prostate.
Discussion
This patient with a Gleason 6 adenocarcinoma of the prostate, which is unilateral on biopsy, and a PSA <10.0 ng/mL has a high likelihood of having disease confined to the prostate. The likelihood of lymph node metastases is unlikely. It is unusual for bone metastasis to be present in patients with PSA levels <10, and therefore this study is not indicated. Additionally, because of the low likelihood of lymph node metastases, computed tomography (CT) scan and magnetic resonance imaging (MRI) are not indicated either. There is mixed evidence for the role of ultrasonography and endorectal MRI in determining the presence of extraprostatic disease; however, these studies have not been generally accepted for making this determination.
▪ Approach
Treatment options vary and include observation, external-beam radiation therapy, brachytherapy, radical prostatectomy, and cryotherapy.
Observation with these findings would be considered in a patient with limited life expectancy, typically due to age or the existence of comorbid disease. Generally, if the patient has a life expectancy of >10 years, experience indicates that he would benefit from surgery or radiation therapy with the anticipation that his life would be extended.
Radiation therapy can be performed either with external beam or brachytherapy. Brachytherapy offers the advantage of being an outpatient procedure with no need for catherization and also avoids the need for repeated visits to the radiation therapy facility. It also appears that the side effects, particularly rectal irritation, are less than with external beam.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree