Case 77
Presentation
The patient is a 45-year-old woman who has been found to be occasionally unarousable by her husband in the early morning hours. She will become coherent if he gives her orange juice to drink. She had a seizure spell that lasted for several minutes when she missed lunch while shopping at the mall one Saturday afternoon. She has gained 20 pounds recently and would like to lose weight. She works as a nurse at a home health agency.
Differential Diagnosis
The differential diagnosis includes insulinoma, fasting hypoglycemia, surreptitious hypoglycemia, and seizure disorder.
The initial diagnostic test is measurement of fasting morning levels of glucose and insulin. The glucose level is 50 mg/dL and the insulin level is 10 microIU/mL. These levels are suggestive of an insulinoma, and the patient is admitted to the hospital to undergo a supervised 72-hour fast. She is placed in the intensive care unit (ICU), where she can be carefully observed. The observation is important to be certain that during the fast she does not develop severe symptoms of neuroglycopenia and that she does not administer any medications or insulin that may induce hypoglycemia. A 24-hour urine for sulfonylurea levels is obtained to rule out the use of oral hypoglycemic drugs. At the start of the fast, a venous catheter is placed to allow administration of dextrose-50 if hypoglycemic symptoms occur. Further, an arterial line is placed to obtain blood samples for insulin and glucose determination. As the test continues, serum levels of glucose and insulin are measured every 6 hours. If the patient develops confusion, slurred speech, altered mental status, or inability to answer simple questions, then serum levels of glucose, insulin, C-peptide, and proinsulin are measured and an ampoule of D-50 is administered to see if the neuroglycopenic symptoms resolve. Patients with insulinoma will develop neuroglycopenic symptoms at approximately 12 to 24 hours during the fast. At that time of symptoms, glucose levels should be <45 mg/dL and insulin levels will be inappropriately elevated to >5 IU/mL in patients with insulinoma. Patients with insulinoma will also have elevated levels of proinsulin and C-peptide. The nurse administers the dextrose intravenously and the neuroglycopenic symptoms should rapidly resolve. Patients with surreptitious hypoglycemia will have normal levels of C-peptide and proinsulin. Whipple’s triad includes neuroglycopenic symptoms, hypoglycemia, and relief of symptoms with glucose administration. These findings are consistent with the diagnosis of insulinoma. Patients with surreptitious hypoglycemia are typically female health care workers who have access to insulin or oral hypoglycemic drugs. They are excluded by careful supervision during the fast, and by measuring C-peptide, proinsulin, and urinary sulfonylurea levels.
Case Continued
At 12 hours into the fast, the patient developed confusion and tremulousness. Serum glucose levels were 35 mg/dL and serum insulin levels were 7 microIU/mL. C-peptide and proinsulin levels were also elevated.
Diagnosis and Recommendation
The findings are diagnostic of insulinoma. Management of the hypoglycemia and localization of the tumor are the next two priorities.
▪ Approach
The next step is to maintain normal blood glucose levels by asking the patient to set the alarm clock at night to awaken from sleep and eat a snack. It is best to mix cornstarch with some of the food so that slower absorption of carbohydrates will allow less
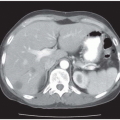
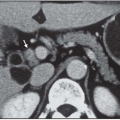
frequent feeding. These two maneuvers will usually keep the blood glucose level in the normal range and avoid neuroglycopenic symptoms. Insulinomas are generally small (<2 cm), benign, and located within the pancreas. The final step is to try to localize the insulinoma. The initial study is a high-resolution computed tomography (CT) scan of the pancreas with intravenous contrast.
frequent feeding. These two maneuvers will usually keep the blood glucose level in the normal range and avoid neuroglycopenic symptoms. Insulinomas are generally small (<2 cm), benign, and located within the pancreas. The final step is to try to localize the insulinoma. The initial study is a high-resolution computed tomography (CT) scan of the pancreas with intravenous contrast.
▪ CT Scan
 Figure 77.1A
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|