Case 76
Presentation
The patient is a 52-year-old man who has severe epigastric pain and diarrhea. He is treated with 20 mg omeprazole daily without resolution of the pain. He has lost 10 pounds. Upper gastrointestinal endoscopy shows a duodenal ulcer and a question of a tumor in the duodenum. He is Helicobacter pylori negative.
Differential Diagnosis
The differential diagnosis includes peptic ulcer, food poisoning, Zollinger-Ellison syndrome (ZES), antral G-cell hyperplasia, and gastric outlet obstruction. Multiple endocrine neoplasia type 1 (MEN-1) should be considered.
Medications that inhibit gastric acid secretion, like omeprazole, should be discontinued for at least 7 days prior to testing. These medications cause achlorhydria and can cause a false elevation in the serum level of gastrin. Similarly, if the patient has evidence of gastric outlet obstruction from ulcer disease or scarring, a nasogastric tube should be inserted to reduce gastric antral distension that can also result in hypergastrinemia. A fasting serum level of gastrin and gastric acid output are measured. Patients with ZES have an elevated fasting serum concentration of gastrin (>100 pg/mL) and an elevated basal acid output (>15 mEq/h). This combination is diagnostic for ZES. A secretin test may also be done, in which 2 U/kg of secretin is administered intravenously and serum levels of gastrin are obtained prior to secretin and at 1, 5, 10, and 15 minutes later. An increase >200 pg/mL in the serum level of gastrin following secretin is consistent with ZES. However, this is not an absolute criterion for the diagnosis, as only 85% of patients with ZES will have a positive secretin stimulation test. Antral G-cell hyperplasia should be excluded by measuring serum levels of gastrin before and after a protein meal. Patients with ZES do not have the gastrin level changed by dietary manipulation. Once the diagnosis of ZES is obtained, the presence of MEN-1 should be excluded. Approximately 20% of patients with ZES have MEN-1. MEN-1 is diagnosed by obtaining a careful family history for the clinical manifestations of MEN-1, examining for lipomas (which are common in MEN-1), and measuring serum levels of prolactin, pancreatic polypeptide, chromogranin A, ionized calcium, and intact parathyroid hormone. Most (95%) patients with MEN-1/ZES have primary hyperparathyroidism at the time of the diagnosis of ZES.
Case Continued
The patient has an elevated serum level of gastrin (950 pg/mL), an elevated basal acid output (100 mEq/h), and an abnormal secretin test (>600 pg/mL incremental increase in gastrin following secretin). There is no family history of endocrine tumors and there are normal serum levels of calcium, parathyroid hormone, prolactin, and pancreatic polypeptide
such that MEN-1 is excluded. Serum levels of chromogranin A are elevated, and this is consistent with ZES.
such that MEN-1 is excluded. Serum levels of chromogranin A are elevated, and this is consistent with ZES.
Diagnosis and Recommendation
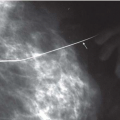
The diagnosis of sporadic Zollinger-Ellison syndrome means that there is a gastrin-secreting neuroendocrine tumor that is causing the severe peptic ulcer disease, diarrhea, and weight loss. The next step in management is to control the acid hypersecretion with medication and to perform localizing studies to try to image the tumor. The key to controlling the symptoms of ZES is to measure the acid output and administer a proton-pump inhibitor at doses that normalize the acid secretion. This typically requires omeprazole at 60 to 80 mg every 12 hours. The acid output should be <10 mEq/h prior to the dose of omeprazole. If the patient has gastroesophageal reflux disease (GERD), the acid output should be kept lower than 5 mEq/h. If the acid output is controlled in this manner, the peptic ulcer disease will heal, the diarrhea will stop, and the patient will gain weight. The next step is to try to image the tumor. High-resolution pancreatic protocol computed tomography (CT) should be performed to try to image the primary tumor and possible liver metastases. Tumors larger than 1 cm are imaged. However, primary gastrinomas may be small and not identified. Somatostatin receptor scintigraphy (SRS), also known as octreotide scan, should also be done. It is a whole-body scan that images the tumor based on the density of type 2 somatostatin receptors. Approximately 90% of gastrinomas will be imaged, and SRS is more sensitive than CT and MRI combined. However, in this particular patient, both CT and SRS failed to identify any gastrinoma.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree