Case 71
Presentation
A 58-year-old white man, human immunodeficiency virus (HIV)-positive since 1989, is referred for evaluation of squamous cell carcinomas of the right forehead, scalp vertex, and left lower eyelid. In the previous 4 years, the patient has been treated for seven cutaneous squamous cell cancers and three recurrences on the scalp, face, and trunk. Past treatment modalities include electrodesiccation and curettage, cryosurgery, surgical excision, Mohs micrographic surgery, and local radiation therapy. He has also started treatment with oral isotretinoin (80 mg/day).
▪ Clinical Photographs
Physical Examination Report
Skin examination on the day of presentation reveals two contiguous erythematous nodules with central keratotic plugs, measuring 6.4 × 3.2 cm in total size, located on the right forehead. The tumors were ulcerated prior to surgery. There is a 1.7 × 1.7-cm erythematous nodule on the left lower lateral canthus and a 3.2 × 2.5-cm nodule on the scalp vertex. Innumerable erythematous patches and plaques on the scalp and forehead are also noted. There were healed scars on the left lower forehead, right upper lip, left shoulder, and central chest. The right forehead tumor was treated 1 year previously with local radiation, but recurred a few months prior to presentation. The left lower eyelid lesion had been treated previously with cryosurgery.
Case Continued
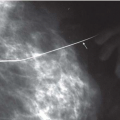
As part of the evaluation, a contrast magnetic resonance imaging (MRI) study of the head shows an ill-defined enhancing process of the anterior scalp extending from the midline to the right and reaching the soft tissue of the face. No bone or intracranial involvement is appreciated.
Differential Diagnosis
Clinically, the differential diagnosis of squamous cell carcinoma (SCC) is broad. Lesions can present with any of various morphologies, most commonly as verrucous, scaly, or ulcerated papules, plaques, or nodules. The clinician may need to differentiate SCC from verruca vulgaris, seborrheic keratosis, actinic keratosis, melanocytic nevus, subcutaneous fungal infection, basal cell carcinoma, melanoma, keratoacanthoma, trauma, herpes virus infection, and primary syphilis, among others. The need for a diagnostic biopsy should be guided by the clinical suspicion for malignancy.
The histology of SCC usually consists of downwardly proliferating masses of epithelial cells that contain atypical squamous cells and horn pearls. These features may vary depending on the tumor subtype and the degree of tumor differentiation. Other commonly recognized histologic subtypes of SCC include spindle-cell, acantholytic (adenoid), mucin-producing, and verrucous carcinomas.
Discussion
Skin cancer is the most common malignancy in humans. More than 1 million new cases of nonmelanoma
skin cancer are diagnosed each year. SCCs account for about 20% of all nonmelanoma skin cancers in whites. In the United States, SCC is estimated to cause between 1,500 and 2,500 deaths per year. The most important etiologic factor for SCC is exposure to ultraviolet radiation, especially during childhood. Exposure to ionizing radiation and chemical carcinogens like arsenic and tar, certain genodermatoses such as xeroderma pigmentosum, human papillomavirus infection, immunosuppression, and chronic skin injury also increase the risk of developing SCC. Fair skin, light hair, and blue eyes are other risk factors for SCC development.
skin cancer are diagnosed each year. SCCs account for about 20% of all nonmelanoma skin cancers in whites. In the United States, SCC is estimated to cause between 1,500 and 2,500 deaths per year. The most important etiologic factor for SCC is exposure to ultraviolet radiation, especially during childhood. Exposure to ionizing radiation and chemical carcinogens like arsenic and tar, certain genodermatoses such as xeroderma pigmentosum, human papillomavirus infection, immunosuppression, and chronic skin injury also increase the risk of developing SCC. Fair skin, light hair, and blue eyes are other risk factors for SCC development.
Actinic keratoses (AK) are considered precursor lesions of cutaneous SCC, and some authors even describe them as a type of carcinoma in situ. Persons with multiple AKs have a 6% to 10% lifetime risk of developing an invasive SCC. Bowenoid papulosis and epidermodysplasia verruciformis are two other conditions that may evolve into invasive SCC and should be followed closely. Squamous cell carcinoma in situ, such as Bowen’s disease (sun-exposed areas) and erythroplasia of Queyrat (glans penis), may also progress to invasive disease if not treated completely.
Although SCC can exhibit a variety of clinical behaviors, including local tissue destruction and metastatic spread, the overall rate of local recurrence and metastasis is <10%. However, a subset of these tumors behaves even more aggressively. This high-risk subset can have rates of recurrence and metastasis up to 47%. Features that correlate with higher risk include diameter >2 cm, rapid tumor growth, location such as the ear or lip, local recurrence, host immunosuppression, poor histologic differentiation, depth of 4 mm or greater, and evidence of perineural invasion.
It is well established that organ transplant recipients, especially those who are fair skinned, have a much higher risk of developing skin cancer than the general population. Basal cell carcinoma (BCC) and SCC account for >90% of all posttransplant skin cancers. The SCC:BCC ratio (1:4 in non-transplant patients) is reversed in organ transplant recipients. SCCs in transplant recipients occur at a younger age and are more likely to be multiple tumors and behave more aggressively. The risk of developing posttransplant SCC is directly proportional to the degree and duration of immunosuppression.
In contrast to posttransplant immunosuppression, the relationship of SCC to HIV is not clear. The major risk factors for developing SCC in HIV patients are similar to those of non-HIV patients and include fair skin type and sun exposure. An increase in the SCC:BCC ratio of the HIV population has not been demonstrated. The number of tumors, local recurrences, metastasis, and survival do not correlate with more advanced disease or lower CD4+ cell counts. However, SCCs in patients with HIV have occurred at a younger age and have been associated with significant morbidity and mortality. Management of high-risk tumors in HIV patients should be analogous to that of organ transplant recipients.
Diagnosis
High-risk invasive squamous cell carcinoma.
Recommendation
Consider options of Mohs micrographic surgery versus excision with wide margins.
▪ Surgical Approach
In 1992, Brodland and Zitelli proposed the currently accepted guidelines for the margins of resection of primary cutaneous SCC. For low-risk tumors, they recommended excision to the level of the subcutaneous fat with margins of no less than 4 mm beyond the clinically definable tumor border. For high-risk tumors, a 6-mm margin was recommended. Their study did not include recurrent SCC, for which Mohs micrographic surgery is considered the treatment of choice.
Mohs surgery is performed in stages. The first stage begins with curettage of the visible tumor to define its gross limits. The area to be excised is then mapped and recorded. The tumor is excised with a narrow margin around the initial curetted site. The resulting specimen is color coded to record the orientation of the tumor. Frozen sections of the entire specimen margin are analyzed for the presence of tumor. If any tumor is present, subsequent stages are performed until the margins are clear. Once clear margins are achieved, the wound may be repaired or, less commonly, allowed to heal by secondary intention, depending on the size and the site of the defect.