Case 7
Presentation
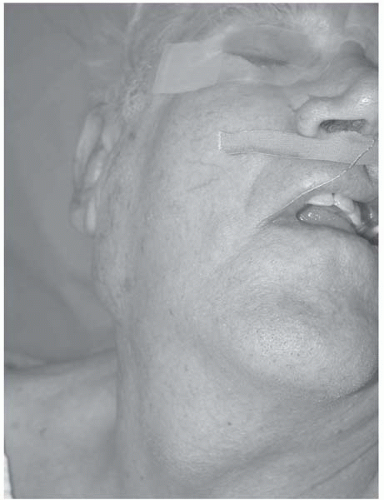
A 55-year-old, previously well man presents with a history of a painless, gradually enlarging mass in the region of the right parotid for about 7 months. He presents after noticing difficulty depressing the right angle of his mouth, and being unable to close his right eye fully for the previous week. He gives a 90-pack-year history of cigarette use and has chewed tobacco for 40 years. He previously had a heavy alcohol intake, but has drunk none in the past decade. There were, however, no symptoms related to the upper aerodigestive tract. Examination reveals facial asymmetry with weakness in the distribution of upper and lower divisions of the facial nerve. There is a firm, nontender mass overlying the right angle of the mandible, somewhat mobile but with a suggestion of fixity to the overlying skin. No adenopathy is palpable elsewhere in the neck. No mucosal lesions or cutaneous tumors are present.
Differential Diagnosis
This man has significant risk factors for mucosal carcinoma of the upper aerodigestive tract, and careful assessment is needed to exclude a mucosal tumor. However, the presence of a mass partially overlying the angle of the mandible, in association with facial nerve weakness, strongly suggests a malignancy arising in, or metastatic to, the parotid salivary gland. In some adult populations, metastatic cutaneous malignancy is the most common cause of a parotid mass, so evidence of a current or previous squamous cell carcinoma or cutaneous melanoma should be sought. A variety of primary parotid malignancies may be the cause; mucoepidermoid carcinoma and adenoid cystic carcinoma are the most common, and both are frequently associated with perineural tumor involvement. Nonepithelial primary malignancies such as sarcoma and lymphoma are less likely, but should be considered. Most parotid tumors are benign, but these are rarely associated with facial nerve weakness. A primary neurogenic tumor or an inflammatory lesion involving the nerve is possible, as is a synchronous benign tumor and unrelated neuropathy; however, active steps should be taken to exclude malignancy even if these diagnoses are suggested. No pulmonary lesion is seen on a chest radiograph.
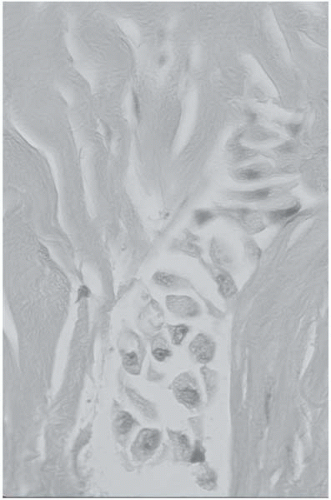
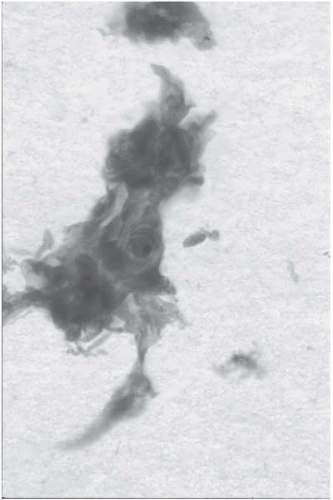
▪ Histopathology Slides
Histopathology Report
Fine-needle aspiration (FNA) biopsy reveals large, malignant pleomorphic cells with features thought likely to be associated with mucoepidermoid carcinoma. Cell block (A) and Papanicolaou stain (B) show malignant cells with dense cytoplasms and high nuclear grades.
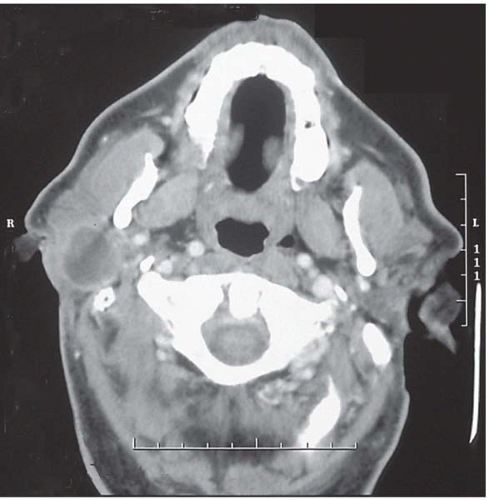
▪ CT Scan
CT Scan Report
Computed tomography (CT) scan of the parotid region of the head and neck shows a 4-cm enhancing mass involving the right parotid gland.
Discussion
FNA biopsy of salivary tumors has been established as an accurate and safe procedure, with a sensitivity and specificity well over 90% with experienced cytopathologists. FNA has been found to alter management of salivary masses in 35% of patients biopsied. In this case, the distinction needs to be made between a primary and a metastatic lesion that will effect management of the neck. Confirming the presence of malignancy allows appropriate counseling about the management of the facial nerve.
Imaging the parotid probably adds little to the assessment of benign lesions in the superficial lobe of the gland, but is necessary in an assessment of malignancy to accurately define the site and extent of the tumor and its relationship to neural and vascular structures and the base of the skull. Both CT scan and magnetic resonance imaging (MRI) can accurately define the relationship of the tumor to the gland and the extent of disease in the neck. CT offers better assessment of bony invasion. MRI would have provided far greater assessment of the extent of perineural spread.